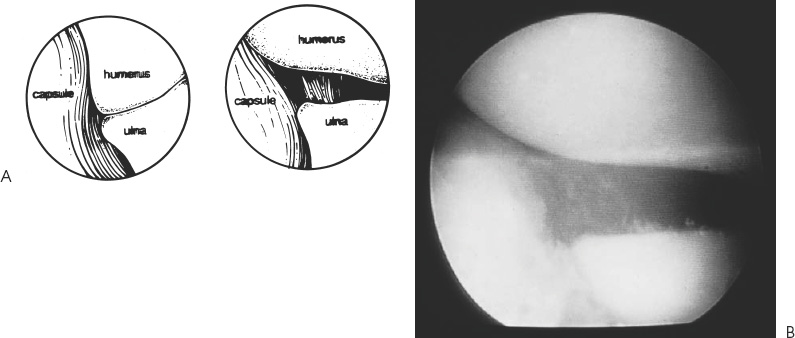
Case 39 A 20-year-old aspiring college baseball pitcher presents with a 6-month history of persistent medial-sided elbow pain that started following an acute, painful pop while pitching. Six months of organized exercises and physical therapy under the guidance of an athletic trainer has not significantly improved his symptoms. Currently, he is unable to pitch at the college level because of persistent medial elbow pain. He denies any locking or catching symptoms. Range of motion of the elbow is normal. No tenderness is exhibited to palpation except inferior to the medial epicondyle over the area of the sublime tubercle of the ulna. Valgus stress testing with the elbow in 30 degrees of flexion causes medial elbow pain and allows for asymmetric opening of the medial ulnohumeral joint. The patient has a negative Tinel’s sign at the elbow and at the wrist. He has no tenderness over the medial epicondyle itself. 1. Ulnar neuritis 2. Medial epicondylitis 3. Medial ulnar collateral ligament (MUCL) disruption 4. Ulnohumeral arthritis Anteroposterior (AP) and lateral radiographs of the elbow demonstrate no abnormalities. Medial Ulnar Collateral Ligament Disruption with Chronic Valgus Instability. The key to making the correct diagnosis of MUCL insufficiency is a detailed history and thorough physical examination. Patients with MUCL ruptures sometimes complain of a sudden pop or an acute onset of pain, but often they do not remember an inciting event. This is particularly true in overhead-motion athletes. At presentation, patients complain primarily of medial sided elbow pain during the acceleration phase of throwing. Rest and nonsteroidal medications tend to help only temporarily. However, symptoms generally recur with resumption of throwing activities. Interestingly, symptoms are usually absent or very minimal when no throwing activities are engaged in. Overuse is generally considered to be the primary cause of MUCL injuries in the throwing athlete. There is point tenderness over the ligament and pain to valgus stress testing. The tenderness over the ligament can be variable, but is most often near the insertion of the ligament at the sublime tubercle of the ulna. Often, careful evaluation of and comparison with the contralateral elbow will demonstrate increased valgus opening with a firm end point only to closing, similar to that felt with medial collateral ligament disruptions of the knee (Fig. 39–1). Figure 39–1. Valgus stability of the elbow can be assessed by applying a valgus stress to the elbow while it is flexed approximately 20 to 30 degrees. Chronic valgus instability also predisposes to a number of other elbow symptoms. Ulnar nerve irritation may occur following acute MUCL tears, or in the presence of chronic valgus instability causing traction neuritis. Chronic MUCL insufficiency may also induce the formation of posterior medial gutter osteophytes that cause pain, loose bodies, and synovitis. Chronic overload of the radiocapitellar joint can also occur with valgus instability, leading to radiocapitellar degeneration, osteophytes, and loose body formation. Though many athletes report a history of acute elbow pain with throwing, patients often report a prodrome of symptoms with an acute episode superimposed. Chronic injury due to repetitive microtrauma to the MUCL with repeated attempts at healing can produce weakness and ultimate failure of the ligament. The valgus extension overload test is another measure of MUCL competency. It is accomplished by bringing the arm into extension while a valgus stress is applied to the elbow. Posteromedial olecranon gutter impingement that results from subluxation associated with MUCL disruption causes pain. As this process continues with repeated overhead activities, osteophytes and progressive impingement symptoms occur. Loose bodies may ultimately be generated, producing a stiff and painful elbow. Treatment of chronic MUCL insufficiency depends on the degree of instability, the activity level of the patient, and the patient’s goals. The great majority of athletes with MUCL disruption do not require surgical intervention, particularly when daily activities or athletics do not require overhead throwing. Simple conservative measures, including nonsteroidal antiinflammatory medications and avoidance of certain activities, are usually all that is required. Even when dealing with overhead-motion athletes, a period of rest from overhead-motion sports combined with an exercise program and nonsteroidal medications will usually lead to symptomatic recovery. However, high-performance athletes require a near-normal elbow, particularly with regard to valgus stability, and often fail to improve sufficiently. At this juncture, discussion with the patient to determine his interests and goals is important. A thorough explanation of the indications for the surgery and the extensive rehabilitation that is required is given. The authors make a specific point of explaining to the patient that the operation to repair or reconstruct the MUCL is being carried out primarily so that the patient can continue in his/her overhead-motion sport and that MUCL insufficiency will likely not cause long-term disability or permanent functional limitations if overhead-motion sports are reduced or eliminated. • Arthroscopy is a valuable adjunct in the diagnosis and treatment of chronic valgus instability, and the authors recommend it for those surgeons experienced with it. • If Jobe and colleagues’ (1986) figure-of-eight reconstruction technique is used, passage of the suture and graft through the distal bony tunnel can be easily accomplished by employing a ductile wire. A 20-gauge wire can simply be cut and fashioned to create a bent-over doubled hook, which can passed through the distal bony tunnel. The leading edge of the suture can be then be passed through the doubled wire and pulled through the bony tunnel. • It is important to recognize that as the MUCL courses distally toward the sublime tubercle, the ulnar nerve converges toward the tubercle as well. Therefore, as one works more distally on the ligament, the ulnar nerve is in progressively closer proximity, and extreme care to retract and protect the nerve is encouraged. Surgical repair or reconstruction of the MUCL is generally reserved for a select subgroup of athletes, as most other athletes improve sufficiently with conservative measures. Surgical treatment involves repair or reconstruction of the MUCL. Surgical intervention consists of two options. Repair of a disrupted MUCL can occasionally be performed, particularly in the acute setting. The other alternative involves reconstruction of the MUCL, usually employing an ipsilateral palmaris longus tendon graft. If reconstruction is considered, preoperative confirmation of the presence of a palmaris longus tendon is extremely important. Reconstructive procedures are designed to re-create a functioning anterior bundle of the MUCL. This bundle has been demonstrated in a number of cadaveric studies to be the primary stabilizing structure to valgus stress. The authors perform elbow arthroscopy at the time of MUCL repair or reconstruction in all patients. One of us (L.D.F.) prefers placing the patient in the supine position for elbow arthroscopy when MUCL reconstruction is to be carried out. The supine position is preferred especially if ulnar nerve transposition is planned. Arthroscopy allows for a thorough intraarticular examination of the elbow, as patients with chronic valgus instability often have secondary changes. These changes include posteromedial gutter osteophytes, olecranon and coronoid process osteophytes, and radiocapitellar joint changes. The MUCL cannot be visualized directly using the arthroscope. However, an indirect measure of valgus instability has been developed. Andrews and Carson (1985) reported an arthroscopic valgus instability test designed to assess the competency of the MUCL. Arthroscopic visualization of the most medial aspect of the ulnohumeral joint while applying a valgus stress with the elbow in 70 degrees of flexion will demonstrate opening of the joint if medial collateral ligament insufficiency is present (Fig. 39–2). The authors have further defined this test by demonstrating that often only 1 mm of ulnohumeral joint opening occurs, even after the entire anterior bundle of the MUCL is sectioned. In the author’s experience, an opening of 1 mm to valgus stress under direct visualization sometimes will respond to simple anterior bundle repair with imbrication of the ligament. However, a significantly increased opening of 2 to 4 mm is unlikely to respond to simple repair and plication, making formal ligament reconstruction necessary. Figure 39–2. The arthroscopic valgus instability test allows for indirect assessment of the competency of the medial ulnar collateral ligament (MUCL). (A) When the anterior bundle of the MUCL is disrupted, valgus stress on the elbow, while held flexed approximately 70 degrees, will allow for ulnohumeral joint opening. (B) An arthroscopic photograph demonstrating pathologic ulnohumeral joint opening. (See Color Plate 39–2B.) • Failure to identify MUCL insufficiency will sometimes lead to worsening symptoms, along with the development of secondary symptoms from continued valgus overload. • Simple ligament repair is usually inadequate treatment for MUCL insufficiency, and formal reconstruction is required. • Failure to place the graft in a near-isometric position may limit motion and result in progressive deformation of the graft with subsequent loosening.
History and Physical Examination
Differential Diagnosis
Radiologic Findings
Diagnosis
Surgical Management
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree