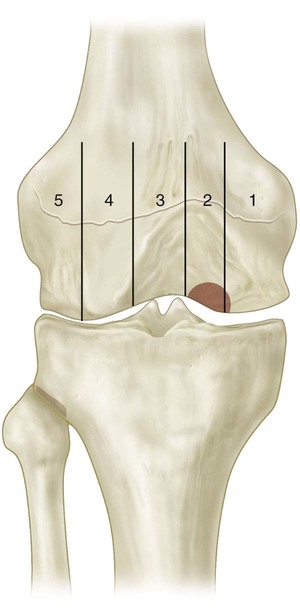
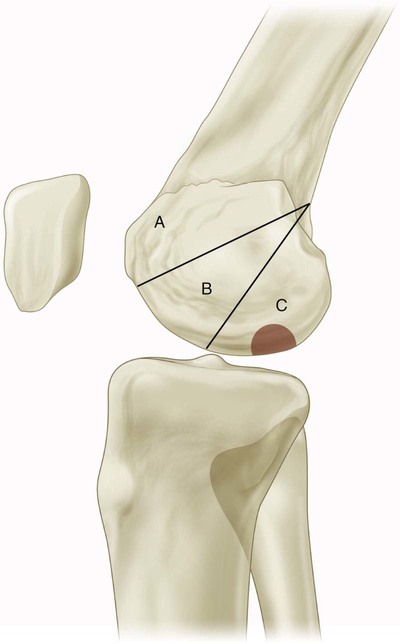
• Radiographic grading (Berndt and Harty)—anteroposterior, lateral, sunrise, and notch views • Bone scan grading (Cahill and Berg) useful for determining healing potential • MRI staging (Hefti et al.) (Figs. 1–3) • Arthroscopic grading (Ewing and Voto/International Cartilage Repair Society) • Posterolateral medial femoral condyle—70% (often only seen on notch view) (Figs. 4 and 5) • Inferocentral lateral femoral condyle—20%
Osteochondritis Dissecans Fixation
Examination/Imaging
 The patient often reports aching, activity-related anterior knee pain. The presentation can be quite similar to patellofemoral syndrome. The presence of OCD should be considered when making the diagnosis of patellofemoral stress syndrome.
The patient often reports aching, activity-related anterior knee pain. The presentation can be quite similar to patellofemoral syndrome. The presence of OCD should be considered when making the diagnosis of patellofemoral stress syndrome.
 Other findings on physical examination include an antalgic gait.
Other findings on physical examination include an antalgic gait.
 Lesions of the medial femoral condyle can present with external rotation gait and pain with internal rotation (Wilson’s sign)
Lesions of the medial femoral condyle can present with external rotation gait and pain with internal rotation (Wilson’s sign)
 It is important to remember that 25% of these chondral lesions occur bilaterally, stressing the importance of checking both knees for symptoms.
It is important to remember that 25% of these chondral lesions occur bilaterally, stressing the importance of checking both knees for symptoms.
 Radiographs, bone scans, and magnetic resonance imaging (MRI) are useful to determine the presence and stage of the OCD lesion.
Radiographs, bone scans, and magnetic resonance imaging (MRI) are useful to determine the presence and stage of the OCD lesion.
 I—visible on radiograph, normal bone scan
I—visible on radiograph, normal bone scan
 II—increased uptake in lesion only
II—increased uptake in lesion only
 III—increased uptake in lesion + femoral condyle
III—increased uptake in lesion + femoral condyle
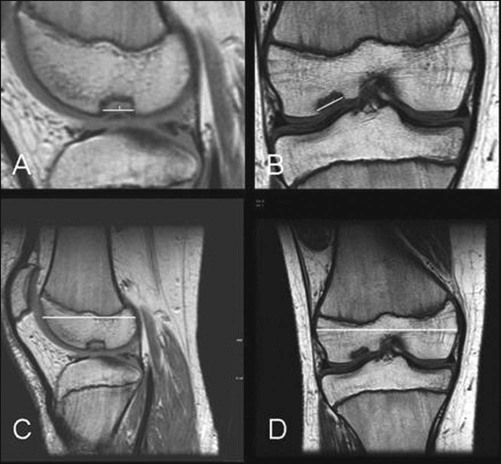


 Stage I—small signal change, no clear margins
Stage I—small signal change, no clear margins
 Stage II—fragment with clear margins without fluid between fragment and bone
Stage II—fragment with clear margins without fluid between fragment and bone
 Stage III—fluid partially visible between fragment and bone
Stage III—fluid partially visible between fragment and bone
 Stage IV—fluid completely surrounds fragment
Stage IV—fluid completely surrounds fragment
Surgical Anatomy
 It is important to perform a complete arthroscopic survey of the knee when evaluating OCD. Fissuring of the chondral surface can lead to loose bodies. These loose bodies should be removed at the time of the operation (Fig. 6)
It is important to perform a complete arthroscopic survey of the knee when evaluating OCD. Fissuring of the chondral surface can lead to loose bodies. These loose bodies should be removed at the time of the operation (Fig. 6)![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


36: Osteochondritis Dissecans Fixation



























