• Acute deformity correction can be performed with subsequent gradual distraction for lengthening at the same osteotomy site. • Double femoral osteotomies can be performed for deformity correction at one site and lengthening at the second site. • Figure 1 shows an example of a patient with congenital femoral deficiency that is undergoing a femoral lengthening. A double-level osteotomy has been performed for acute deformity correction both proximally and distally with concurrent lengthening at the distal osteotomy site. • Concurrent contractures or joint/bony abnormalities must be documented. • Concurrent joint instabilities and ligamentous deficiencies must be documented. • Malalignment and malorientation tests are performed to determine concurrent deformity and location of deformity. • Limb lengths are assessed (the pelvis should be leveled with blocks and the number of blocks noted on the radiograph). • The radiographs are checked for fixed flexion deformity of the knee. • A malorientation test is performed to determine the presence and location of sagittal plane deformity. • The radiographs are checked for joint subluxation (significant anterior-posterior instability). • Significant dysplasia will result in increased risk of hip dislocation. • Significant dysplasia requires pelvic osteotomy prior to femoral lengthening (Dega osteotomy, triple osteotomy, periacetabular osteotomy). • This structure will be penetrated by the laterally placed half-pins. • If a preoperative contracture is present, then a prophylactic release is required at the time of surgery. • These nerves are not directly at risk during the external fixation application or osteotomy. • Rapid lengthening or concurrent deformity correction can place tension on the neural elements. • Significant instability will result in increased risk of joint subluxation or dislocation. • Severe knee instability should be addressed with ligamentous reconstruction and patella realignment prior to femoral lengthening. • This marks the limb’s mechanical axis. • If the mechanical axis runs through the center of the knee joint, then a straight lengthening can be performed without concurrent deformity correction. • If an abnormal mechanical axis is present, then preoperative planning is required to determine the level of the deformity.
Femoral Lengthening with External Fixation
Indications
 Femoral shortening with or without concurrent limb deformity
Femoral shortening with or without concurrent limb deformity

 Femoral shortening greater than 7–8 cm will require sequential lengthenings or a combination of lengthening and epiphysiodesis.
Femoral shortening greater than 7–8 cm will require sequential lengthenings or a combination of lengthening and epiphysiodesis.
 Femoral shortening greater than 3 cm that cannot be treated with more conservative methods (shoe lifts or epiphysiodesis)
Femoral shortening greater than 3 cm that cannot be treated with more conservative methods (shoe lifts or epiphysiodesis)
Examination/Imaging
Physical Examination
 Range of motion of the hip, knee, and ankle joints
Range of motion of the hip, knee, and ankle joints
 Special consideration must be given to knee fixed flexion deformity. The cause (soft tissue contracture vs. bony deformity) must be determined.
Special consideration must be given to knee fixed flexion deformity. The cause (soft tissue contracture vs. bony deformity) must be determined.
 Clinical limb-length assessment
Clinical limb-length assessment
Radiographic Examination
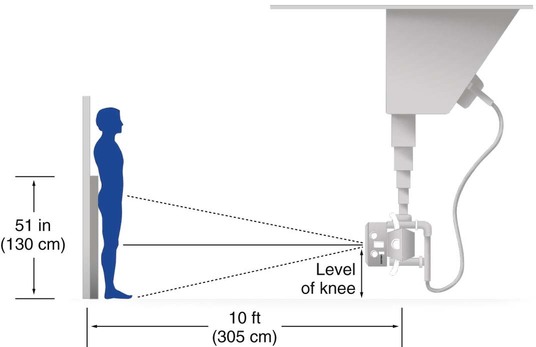
 Anteroposterior (AP) and lateral standing long-leg radiographs are obtained (taken at a distance of 10 feet using a 51-inch cassette) (Figs. 2 and 3).
Anteroposterior (AP) and lateral standing long-leg radiographs are obtained (taken at a distance of 10 feet using a 51-inch cassette) (Figs. 2 and 3).
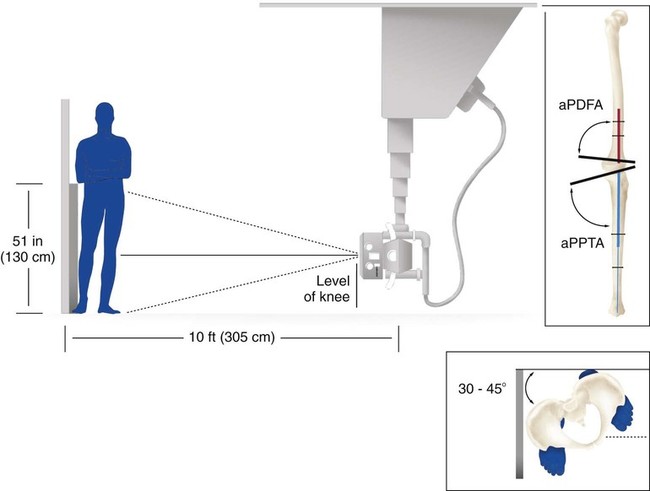
 Standing long-leg lateral radiographs (with maximum knee extension) are obtained (Fig. 4).
Standing long-leg lateral radiographs (with maximum knee extension) are obtained (Fig. 4).

 Significant joint or limb deformity should be assessed on a separate radiograph centered on the joint or limb segment of interest.
Significant joint or limb deformity should be assessed on a separate radiograph centered on the joint or limb segment of interest.
 A supine AP pelvis radiograph should be obtained prior to lengthening to assess the integrity of the hip joint (center-edge angle and appearance of the sourcil).
A supine AP pelvis radiograph should be obtained prior to lengthening to assess the integrity of the hip joint (center-edge angle and appearance of the sourcil).
Surgical Anatomy
 Tensor fascia lata/iliotibial band (ITB)
Tensor fascia lata/iliotibial band (ITB)
 At the end of the procedure, the knee must be maximally flexed to stretch/tear the fascia lata around the half-pins.
At the end of the procedure, the knee must be maximally flexed to stretch/tear the fascia lata around the half-pins.
 If the fascia lata is not stretched, a postoperative knee extension contracture will result with minimal knee flexion.
If the fascia lata is not stretched, a postoperative knee extension contracture will result with minimal knee flexion.
 The sciatic nerve is tethered as the common peroneal nerve enters the lateral compartment of the lower leg.
The sciatic nerve is tethered as the common peroneal nerve enters the lateral compartment of the lower leg.
 Peroneal nerve tension or irritation initially will result in pain on the anterior aspect of the lower leg and dorsum of the foot and altered sensation in the first web space. Late findings include weakness of dorsiflexors or footdrop. Young patients will often hold the toes up with their hands or continuously rub their foot. Treatment involves slowing the rate of distraction, allowing the hip to extend and the knee to flex, and decompression of the peroneal nerve.
Peroneal nerve tension or irritation initially will result in pain on the anterior aspect of the lower leg and dorsum of the foot and altered sensation in the first web space. Late findings include weakness of dorsiflexors or footdrop. Young patients will often hold the toes up with their hands or continuously rub their foot. Treatment involves slowing the rate of distraction, allowing the hip to extend and the knee to flex, and decompression of the peroneal nerve.
 A contracted ITB will result in rotatory subluxation of the knee joint with concurrent knee flexion contracture and patella dislocation.
A contracted ITB will result in rotatory subluxation of the knee joint with concurrent knee flexion contracture and patella dislocation.
 Contracted hamstrings will result in posterior subluxation/dislocation of the knee joint.
Contracted hamstrings will result in posterior subluxation/dislocation of the knee joint.
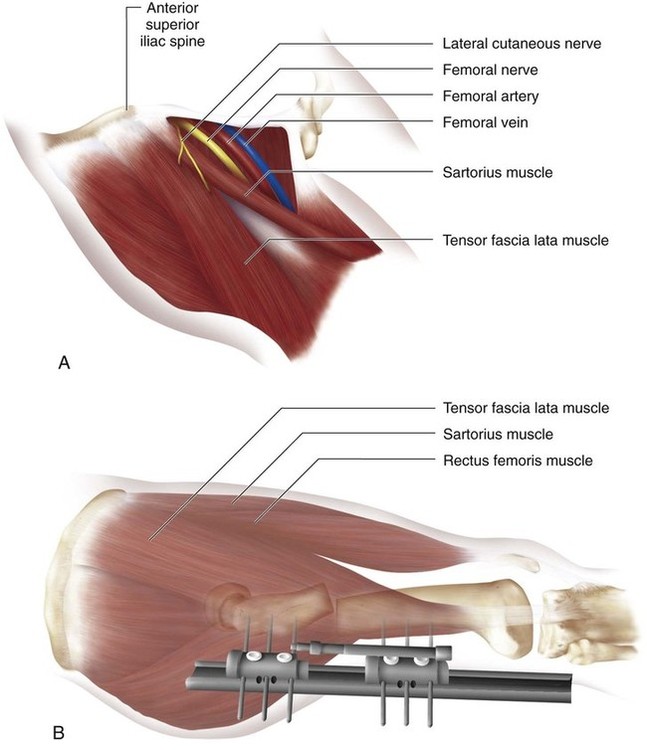
 Figure 5 illustrates the neurovascular structures of the proximal anterior thigh region that are located medial to the sartorius muscle (Fig. 5A) and the typical placement of the monolateral external fixator for femoral lenghthening (Fig. 5B). Note that the external fixation pins are placed from the lateral position posterior to the tensor fascia lata muscle and away from the neurovascular elements.
Figure 5 illustrates the neurovascular structures of the proximal anterior thigh region that are located medial to the sartorius muscle (Fig. 5A) and the typical placement of the monolateral external fixator for femoral lenghthening (Fig. 5B). Note that the external fixation pins are placed from the lateral position posterior to the tensor fascia lata muscle and away from the neurovascular elements.
Positioning
 The patient is placed supine on a radiolucent table that allows visualization from the hips to the ankles.
The patient is placed supine on a radiolucent table that allows visualization from the hips to the ankles.
 The fluoroscopy machine is placed on the opposite side of the operating room (OR) table and perpendicular to the involved extremity.
The fluoroscopy machine is placed on the opposite side of the operating room (OR) table and perpendicular to the involved extremity.
 A small bump is placed under the ipsilateral sacrum to allow the lower extremity to rest in a patella-forward position.
A small bump is placed under the ipsilateral sacrum to allow the lower extremity to rest in a patella-forward position.
 The entire lower extremity is prepped and draped to include the groin area, gluteal region, and iliac crest to the subcostal margin.
The entire lower extremity is prepped and draped to include the groin area, gluteal region, and iliac crest to the subcostal margin.
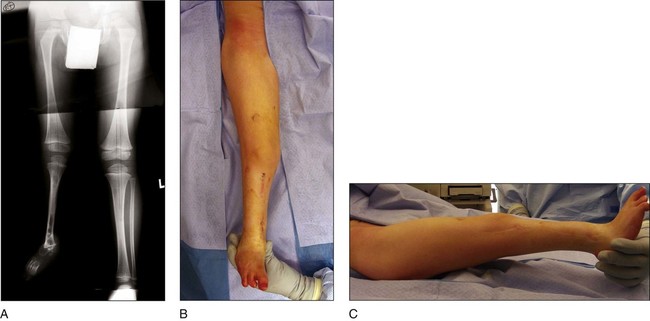
 Figure 6 shows a patient with fibular hemimelia with significant concurrent congenital femoral deficiency (Fig. 6A). The patient’s lower extremity is draped to allow entire access from the pelvis to the foot (Fig. 6B and 6C).
Figure 6 shows a patient with fibular hemimelia with significant concurrent congenital femoral deficiency (Fig. 6A). The patient’s lower extremity is draped to allow entire access from the pelvis to the foot (Fig. 6B and 6C).
Procedure: External Fixator Placement
Step 1
 The limb is held patella forward and the patient is adjusted so a line on the radiopaque grid runs through the center of the hip joint.
The limb is held patella forward and the patient is adjusted so a line on the radiopaque grid runs through the center of the hip joint.
 The limb is adducted or abducted to center the ankle on the same radiopaque line that runs through the hip.
The limb is adducted or abducted to center the ankle on the same radiopaque line that runs through the hip.





























































