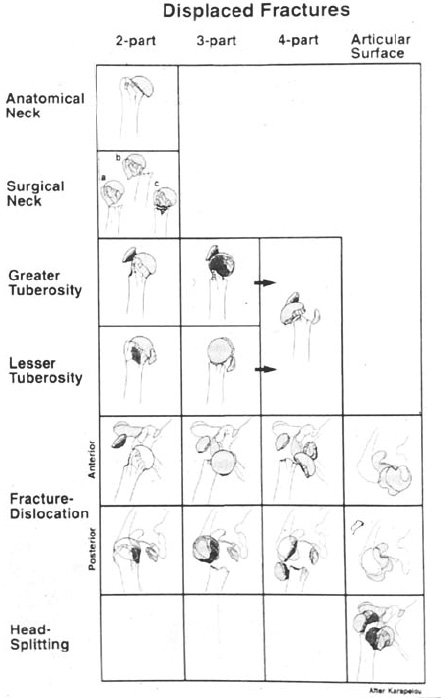
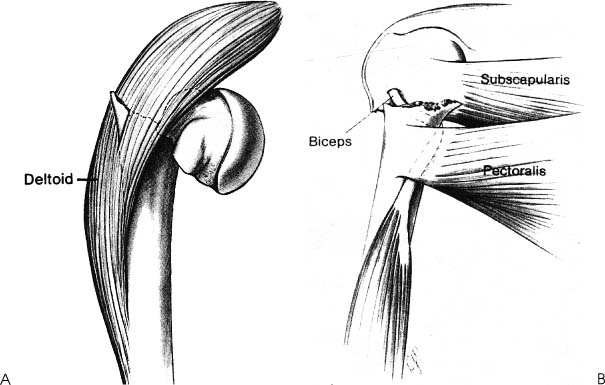
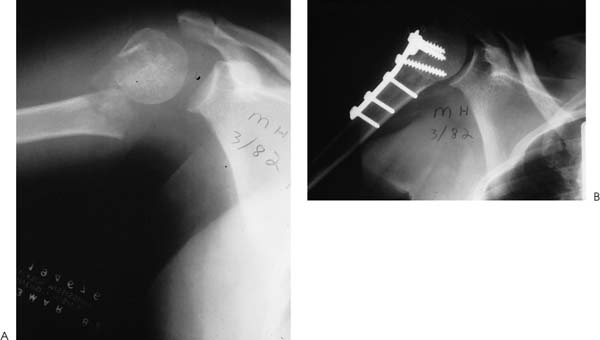
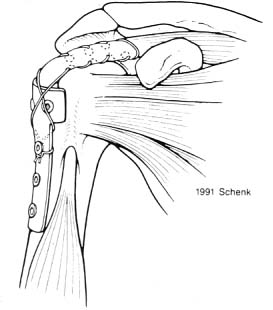
Case 2 A 45-year-old man presents to the office several hours after falling 8 feet from a ladder onto his shoulder. He reports pain, crepitus, and weakness in the shoulder. He denies any numbness or other significant abnormality. Range of motion is limited secondary to pain. Crepitus is felt through the limited range of motion that is possible. Careful neurologic and vascular examination demonstrates normal distal pulses, excellent capillary refill, and intact sensation in the area of the shoulder. Also, isometric contraction of the three heads of the deltoid can be palpated. Moderate swelling is present about the shoulder. Figure 2–1. An anteroposterior (AP) (A), axillary (B), and scapular Y (C) view of the shoulder. 1. Shoulder dislocation 2. Proximal humerus fracture 3. Scapular fracture 4. Rotator cuff tear A three-view trauma series is obtained (Fig. 2–1). Displaced Surgical Neck Fracture. The swelling and crepitus at initial presentation make a shoulder fracture a likely possibility. Radiographs confirm the fracture pat tern. Displacement of surgical neck fractures can generally be assessed on a routine radiograph, but computed tomography (CT) scans can be performed if there are questions about the degree of displacement and/or orientation of the humeral head. As in all fractures of the proximal humerus, a careful and thorough neurovascular examination should be performed. Axillary nerve and arterial injury does occur. Particular attention should be paid to the axillary nerve, with careful assessment of sensation about the shoulder. Also, although swelling about the shoulder may limit the ability to assess deltoid function, careful palpation of each of the three heads of the deltoid will usually allow for confirmation of the patient’s ability to contract this muscle. Most surgical neck fractures of the proximal humerus are minimally displaced and stable, and may be treated nonoperatively. A determination of the degree of displacement and angulation of the fracture fragments is important in selecting the best form of treatment. Neer (1970) has done much to characterize proximal humerus fracture patterns and has pointed out that three types of displaced surgical neck fractures are seen: impacted and angulated, unimpacted, and comminuted (Fig. 2–2). This classification system is based on the displacement and angulation of the fracture fragments relative to each other. If there is 1 cm of displacement or 45 degrees of angulation between fracture fragments, then these fracture fragments are considered displaced relative to one another. However, this characterization of relative displacement of the fracture fragments should be used only as a guide to treatment. Fracture management must be individualized based on age, activity level, and goals of the patient. CT scanning can be very helpful in more accurately determining displacement and angulation. It is routinely performed by the authors when surgical intervention is not clearly indicated. Figure 2–2. The Neer classification system for proximal humerus fractures. Most two-part surgical neck fractures can be managed nonoperatively. Impacted fractures, even if angulated, usually maintain adequate stability after closed reduction. The rationale for closed reduction is to decrease the amount of angulation of the fracture, which might result in permanent limitation of shoulder motion. Gentle traction on the arm usually allows for disimpaction of the angulated fracture fragments after which time a reduction is attempted. We perform an initial reduction attempt in the emergency room. The arm is generally placed in an immobilizer or Velpeau dressing with the arm in adduction, to relax the anteromedial pull of the pectoralis muscle on the humeral shaft. If radiographs demonstrate an unsatisfactory reduction, then further attempts at closed reduction should be carried out in the operating room. For unimpacted and angulated fractures, persistent displacement will often result, and the authors generally perform open reduction and internal fixation in such cases. If adequate closed reduction cannot be obtained in the operating room, or if the fracture displacement is best treated by open reduction and internal fixation, surgery is carried out. For those fractures amenable to an attempt at closed reduction, such reduction can be carried out under general endotracheal anesthesia. If a closed reduction can be achieved, but is unstable and difficult to maintain, either open reduction and internal fixation or percutaneous pin fixation may be carried out. If a satisfactory reduction can be achieved but not maintained, percutaneous pins may be used to hold the reduction during the early healing period (Fig. 2–3). Several Kirschner wires (K-wires) or threaded pins can be placed using fluoroscopic imaging and a power drill. Patient positioning is important when hardware is used in the shoulder. The authors prefer to use a large beanbag and the beach chair position, which provide for significant lateral translation of the patient off the edge of the operating table, allowing the fluroscopy unit complete access to the shoulder. If the reduction and pin position are satisfactory, the pins can be cut beneath the surface of the skin and the arm immobilized. Gentle pendulum exercises may be started after 2 to 3 weeks, but the pins are not removed until radio-graphic evidence of healing is seen. This usually occurs at 4 to 6 weeks postoperatively. Figure 2–3. Displaced two-part surgical neck fracture treated with percutaneous pin fixation. (A) An AP X-ray of a displaced two-part surgical neck fracture. (B) An axillary view following percutaneous pin fixation demonstrating good alignment. When a satisfactory closed reduction cannot be achieved, open reduction and internal fixation is carried out. In these cases, soft tissue interposition from the biceps tendon or deltoid is a common cause of persistent displacement despite attempts at closed reduction (Fig. 2–4). Various techniques have been proposed for displaced two-part surgical neck fractures: skeletal traction, external fixation, plates and screws, intramedullary nails, percutaneous pins, and tension band intramedullary wires or sutures. The choice of fracture fixation technique depends on the fracture pattern, the bone quality, and the presence or absence of comminution. The authors generally prefer plate and screw fixation in young, healthy individuals with good bone quality. Alternative approaches include the use of figure-of-eight nonabsorbable sutures or wires with or without supplementation using intramedullary devices. A long deltopectoral approach is used, preserving the deltoid origin and insertion. The cephalic vein is identified and retracted laterally with the deltoid, and a self-retaining retractor is placed in the deltopectoral interval. The clavipectoral fascia and the coracoacromial ligament are released. The fracture site is then visualized and cleaned of clot and debris. Any soft tissue interposition is documented, and reduction accomplished. Figure 2–4. Soft tissue interposition can prevent adequate reduction of two-part proximal humerus fractures. (A) Deltoid muscle interposition can prevent fracture realignment. (B) Biceps tendon interposition between the fracture fragments can limit the ability to reduce the fracture. (From Peimer A. Surgery of the Hand and Upper Extremity. New York: McGraw-Hill, 1996. With permission of The McGraw-Hill Companies.) Figure 2–5. Fracture fixation of a displaced surgical neck fracture using an AO T plate. (A) Preoperative AP radiographs demonstrate a displaced surgical neck fracture irreducible after attempts at closed reduction. (B) An AP radiograph demonstrating reduction and fixation of the surgical neck fracture. Once adequate exposure and reduction is achieved, fixation is accomplished. When an AO T plate and screws are used, the plate is applied to the lateral border of the humeral head and shaft, and screws sequentially placed. Care must be taken to maintain the plate relatively low on the humeral head, so as to avoid postoperative impingement of the plate with forward flexion and abduction (Fig. 2–5). Fluoro scopic evaluation is used to confirm reduction and hardware position. Also, prior to final tightening of the screws, a no. 5 nonabsorbable suture can be passed in a Bun-nell-type fashion or figure-of-eight fashion through the rotator cuff and under the plate to supplement the stability achieved by the plate alone (Fig. 2–6). An assessment of stability through a range of motion is carried out intraoperatively under direct visualization. Routine closure of the deltopectoral interval, soft tissues, and skin is carried out over a drain. Figure 2–6. An illustration demonstrating a nonabsorbable suture used to supplement plate fixation for a displaced surgical neck fracture. PEARLS • Accurate assessment of the reduction is sometimes difficult because of the depths of the wound. Use of the fluoroscopic unit can help confirm adequate reduction. • Use of supplemental nonabsorbable sutures under the plate and through the rotator cuff tendon in a figure-of-eight fashion will help to effectively supplement the stability achieved by the plate and screw construct.
History and Physical Examination
Differential Diagnosis
Radiologic Findings
Diagnosis
Surgical Management
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree