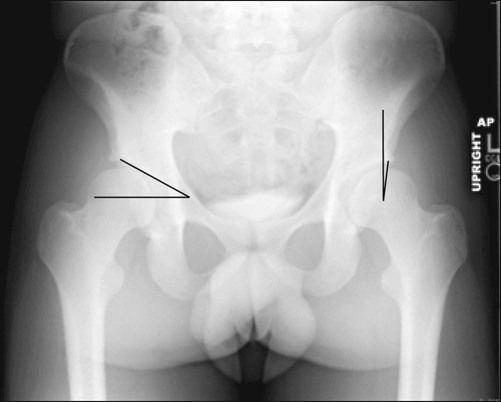
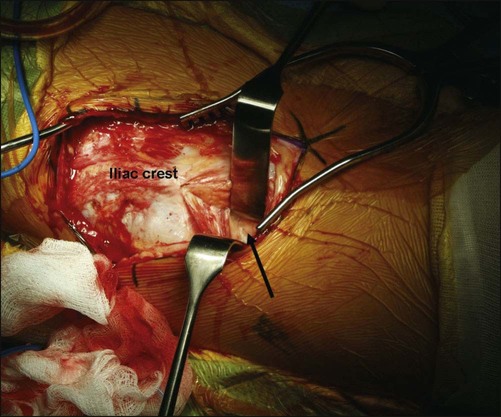
• Examination should begin with review of standing posture with careful attention to limb-length discrepancy, pelvic tilt, and weakness in single-limb stance. Gait evaluation for an abductor lurch, positive Trendelenburg’s sign, and dynamic rotational alignment is essential. • Seated and recumbent examination should include careful neurologic and musculoskeletal assessment, with attention to subtle asymmetry in limb size (thigh circumference), sensation, and motor function. While complete examination should include all muscle groups, focus upon hip abductor strength and fatigue is paramount. Evaluation of iliopsoas tendon tenderness, snapping, and function should be included. • Range-of-motion testing and provocative maneuvers remain a mainstay of clinical evaluation. At a minimum, testing should include evaluation for hip flexion contractures, rotational profiles in flexion and extension, and provocative tests for instability and impingement. The apprehension test, anterior and posterior impingement tests, and evaluation for tenderness overlying the piriformis muscle are helpful tools to investigate symptoms of discomfort. • Figure 1 shows a standing bilateral AP radiograph of the hips. On the left hip, the lateral center-edge angle of Wiberg is drawn. On the right hip, the Tönnis acetabular roof angle is drawn. Note that the edge line is drawn to the end of the edge of the weight-bearing sourcil. • Figure 2 shows a standing false profile view of the hip. The anterior center-edge angle of Lequesne is drawn. Note that the edge line is drawn to the end of the edge of the weight-bearing sourcil. • Figure 3 shows a supine AP radiograph of the pelvis with the hips in abduction and internal rotation. This is to simulate what the hip would look like following reorientating periacetabular osteotomy (PAO). Congruency is measured on this view preoperatively and on the standing AP radiograph postoperatively. • The first window is created proximally by dissection of the external oblique fascia off the iliac crest. Subperiosteal dissection of the iliacus along the inner table of the pelvis should ensue. • In the second, more distal window, the compartment of the tensor fascia lata is entered and the muscle bluntly dissected off the septum with the sartorius muscle. This is in an effort to protect the lateral femoral cutaneous nerve. The floor of this compartment is identified proximally until the anterior ilium is palpated. Dissection along the deep interval between the rectus femoris and gluteus medius includes division of the reflected head of the rectus femoris (Fig. 6). Once this dissection has been carried down to the hip capsule, the two windows are connected through an osteotomy and reflection of the ASIS with its attached sartorius muscle.
Bernese Periacetabular Osteotomy
Examination/Imaging
 Symptoms of hip dysplasia are commonly overlooked, leading to significant delays in diagnosis. Seemingly benign complaints of pain overlying the inguinal structures, greater trochanter, and buttocks are frequently dismissed by patients and physicians alike. Complaints of weakness, instability, locking, or catching are often noted. Referred pain to the ipsilateral knee and lumbosacral spine should be investigated appropriately.
Symptoms of hip dysplasia are commonly overlooked, leading to significant delays in diagnosis. Seemingly benign complaints of pain overlying the inguinal structures, greater trochanter, and buttocks are frequently dismissed by patients and physicians alike. Complaints of weakness, instability, locking, or catching are often noted. Referred pain to the ipsilateral knee and lumbosacral spine should be investigated appropriately.
 Family history remains a vital aspect of clinical evaluation. Strong evidence supports an underlying genetic link for dysplasia and subsequent arthrosis. Not uncommonly, evaluation and history of a young adult patient reveals parents and extended family affected by late-stage disease. Similarly, children of patients demonstrating symptoms of dysplasia should be carefully evaluated.
Family history remains a vital aspect of clinical evaluation. Strong evidence supports an underlying genetic link for dysplasia and subsequent arthrosis. Not uncommonly, evaluation and history of a young adult patient reveals parents and extended family affected by late-stage disease. Similarly, children of patients demonstrating symptoms of dysplasia should be carefully evaluated.
 Medical history should include careful review for prior hospitalizations, use of corticosteroids, neonatal sepsis, and childhood trauma. The history and examination should elicit information regarding the variety of syndromes that predispose to abnormal hip development, including Marfan syndrome, Ehlers-Danlos syndrome, Charcot-Marie-Tooth disease, trisomy 21, and cerebral palsy.
Medical history should include careful review for prior hospitalizations, use of corticosteroids, neonatal sepsis, and childhood trauma. The history and examination should elicit information regarding the variety of syndromes that predispose to abnormal hip development, including Marfan syndrome, Ehlers-Danlos syndrome, Charcot-Marie-Tooth disease, trisomy 21, and cerebral palsy.
 Systematic, thorough physical examination is imperative to evaluation of the dysplastic hip.
Systematic, thorough physical examination is imperative to evaluation of the dysplastic hip.
 Standard workup should include an anteroposterior (AP) pelvis radiograph centered on the femoral heads, the frog-leg lateral and false profile views popularized by Lequesne, and abduction-internal rotation views as described by Von Rosen. Careful attention should be paid to measurement of the Tönnis angle, anterior and lateral center-edge angles, femoral head sphericity as described by Nötzli, head-neck offset, acetabular version, the presence of a posterior wall sign, and joint congruity.
Standard workup should include an anteroposterior (AP) pelvis radiograph centered on the femoral heads, the frog-leg lateral and false profile views popularized by Lequesne, and abduction-internal rotation views as described by Von Rosen. Careful attention should be paid to measurement of the Tönnis angle, anterior and lateral center-edge angles, femoral head sphericity as described by Nötzli, head-neck offset, acetabular version, the presence of a posterior wall sign, and joint congruity.


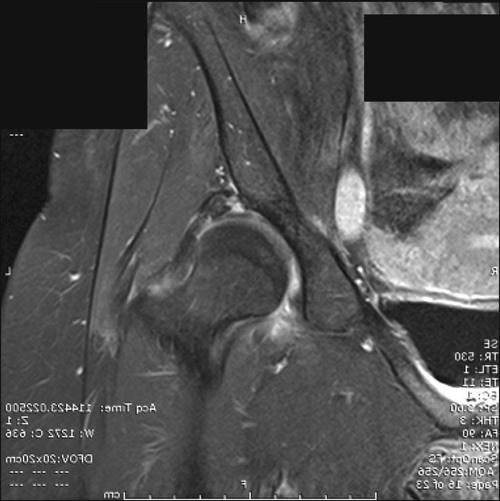
 Advanced imaging modalities, including magnetic resonance imaging (MRI; Fig. 4), computed tomography, and ultrasound, offer valuable insights for perioperative planning. Recent investigations have detailed the valuable prognostic utility of intravenous gadolinium–enhanced MRI for patients being considered for Bernese PAO.
Advanced imaging modalities, including magnetic resonance imaging (MRI; Fig. 4), computed tomography, and ultrasound, offer valuable insights for perioperative planning. Recent investigations have detailed the valuable prognostic utility of intravenous gadolinium–enhanced MRI for patients being considered for Bernese PAO.
Surgical Anatomy
 The lateral femoral cutaneous nerve should be protected throughout the procedure. The tensor-sartorius surgical interval may be approached by entering the tensor fascia lata just distal and lateral to the anterior superior iliac spine (ASIS). Once the fascia is incised in line with its fibers, blunt dissection may be carried out medially to enter the appropriate interval. Patients should be counseled preoperatively regarding possible neurapraxia.
The lateral femoral cutaneous nerve should be protected throughout the procedure. The tensor-sartorius surgical interval may be approached by entering the tensor fascia lata just distal and lateral to the anterior superior iliac spine (ASIS). Once the fascia is incised in line with its fibers, blunt dissection may be carried out medially to enter the appropriate interval. Patients should be counseled preoperatively regarding possible neurapraxia.
 The sciatic nerve is at risk primarily during the osteotomy of the posterior column. The osteotomy of the posterior column should initially be performed to, but not through, the lateral cortex. The osteotomy may be carefully completed with a Ganz osteotome just prior to correction of the acetabular fragment.
The sciatic nerve is at risk primarily during the osteotomy of the posterior column. The osteotomy of the posterior column should initially be performed to, but not through, the lateral cortex. The osteotomy may be carefully completed with a Ganz osteotome just prior to correction of the acetabular fragment.
 The femoral nerve is at heightened risk during osteotomy of the ischium. Tension should be relieved by placing a large bump underneath the operative extremity, thereby flexing the hip and reducing tension on the nerve.
The femoral nerve is at heightened risk during osteotomy of the ischium. Tension should be relieved by placing a large bump underneath the operative extremity, thereby flexing the hip and reducing tension on the nerve.
 The medial femoral circumflex artery can potentially be injured during distal dissection along the ischium in preparation for osteotomy. Care should be taken not to dissect distal to the obturator externus tendon during preparation for this cut, which begins in the infracotyloid groove just distal to the transverse acetabular ligament.
The medial femoral circumflex artery can potentially be injured during distal dissection along the ischium in preparation for osteotomy. Care should be taken not to dissect distal to the obturator externus tendon during preparation for this cut, which begins in the infracotyloid groove just distal to the transverse acetabular ligament.
Positioning
 The patient is positioned supine on a radiolucent Jackson table. A preoperative supine radiograph is helpful for correlation with intraoperative correction.
The patient is positioned supine on a radiolucent Jackson table. A preoperative supine radiograph is helpful for correlation with intraoperative correction.
 Epidural analgesia is commonly used for perioperative pain management.
Epidural analgesia is commonly used for perioperative pain management.
 The shoulder of the operative side may be gently positioned in abduction and external rotation to facilitate surgical access to the operative site, with care taken to avoid excessive traction on the brachial plexus.
The shoulder of the operative side may be gently positioned in abduction and external rotation to facilitate surgical access to the operative site, with care taken to avoid excessive traction on the brachial plexus.
 The entire lower extremity should be prepped and draped freely to facilitate intraoperative assessment of joint motion.
The entire lower extremity should be prepped and draped freely to facilitate intraoperative assessment of joint motion.
Portals/Exposures
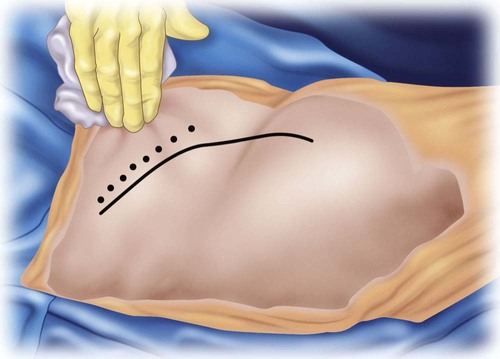
 Surgical technique relies on a modified iliofemoral approach. While an extended skin incision curving longitudinally may improve access, poor wound healing and cosmesis may result. More limited incisions paralleling the ilioinguinal ligament and iliac wing may provide sufficient exposure and improved wound healing.
Surgical technique relies on a modified iliofemoral approach. While an extended skin incision curving longitudinally may improve access, poor wound healing and cosmesis may result. More limited incisions paralleling the ilioinguinal ligament and iliac wing may provide sufficient exposure and improved wound healing.
 A “bikini line” incision is used after administration of local anesthetic. A mixture of normal saline with epinephrine may be injected to reduce blood loss. The incision varies in size with patient body habitus. Typical incisions are 12–14 cm in length, paralleling but just distal to the iliac crest, terminating medially 1–2 cm beyond the palpated tensor-sartorius interval (Fig. 5).
A “bikini line” incision is used after administration of local anesthetic. A mixture of normal saline with epinephrine may be injected to reduce blood loss. The incision varies in size with patient body habitus. Typical incisions are 12–14 cm in length, paralleling but just distal to the iliac crest, terminating medially 1–2 cm beyond the palpated tensor-sartorius interval (Fig. 5).
 The initial exposure relies on the creation of two windows.
The initial exposure relies on the creation of two windows.
Musculoskeletal Key
Fastest Musculoskeletal Insight Engine






