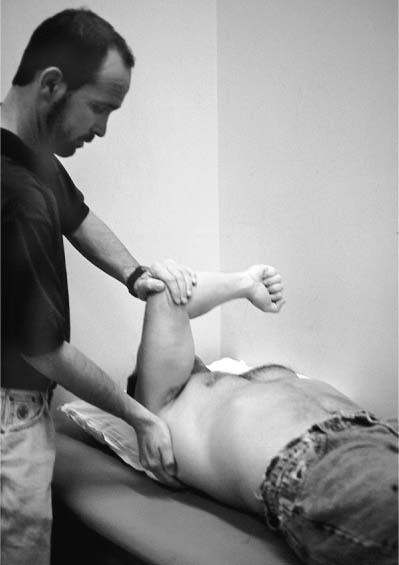
Case 13 A 20-year-old college football player presents with a 2-year history of posterior shoulder pain accompanied by occasional episodes of “shifting out” of the joint. Also, the athlete states that his shoulder has required relocation in the emergency room on two occasions. He is an offensive lineman and has difficulty blocking with his arms outstretched because of shoulder pain. Also, he relates a history of several subluxation events occurring with the arm in front of the body while blocking. He denies any numbness or weakness. The patient is strong and muscular, with normal range of motion and no atrophy or asymmetry of the shoulder. He is neurovascularly intact. Strength testing demonstrates no abnormality, but he does have tenderness in the area of posterior rotator cuff musculature near the joint line. Translation testing demonstrates no significantly increased anterior translation and no appreciable sulcus sign. But he does have 2+ increased posterior translation and pain during posterior translation. He also has a positive forward flexion–internal rotation compression test for pain. This test is accomplished by applying a longitudinal compression force on the glenohumeral joint with the patient’s arm forward flexed 90 degrees, maximally internally rotated, and neutrally adducted (Fig. 13–1). He also has a negative apprehension sign and relocation test. Figure 13–1. The forward flexion–internal rotation compression test is often positive for pain in patients with posterior instability. 1. Posterior rotator cuff tear 2. Superior labrum anterior and posterior (SLAP) lesion 3. Recurrent posterior shoulder instability 4. Suprascapular nerve injury Anteroposterior (AP), axillary, and scapular Y views of the shoulder failed to demonstrate any abnormalities. Recurrent Posterior Shoulder Instability. Posterior shoulder instability is diagnosed based primarily on the complaints of the patient, the history of recurrent subluxation and dislocation events, and the physical examination, particularly as it relates to translation testing. This patient clearly demonstrated increased translation posteriorly, and this increased translation reproduced the patient’s symptoms. Diagnosis of posterior shoulder instability can be difficult at least partly due to the relatively uncommon incidence of this instability pattern. This is especially true in an athletic population, in whom anterior shoulder instability occurs very commonly. A careful history and thorough physical examination is required to accurately diagnose the direction of instability. Patients with recurrent posterior shoulder instability often relate no history of subluxation events, but only report shoulder pain. This patient did have a history of recurrent dislocation and subluxation events. Posterior instability may present with pain referred to the posterior and/or anterior area of the shoulder. Pain and other symptoms can be related to a reverse Bankart lesion or anterior capsular contracture, if present. The abnormal joint bio-mechanics due to persistent instability may also lead to rotator cuff inflammation. The resulting impingement symptoms may become more disabling than the instability itself. Patients with posterior instability will often describe a sensation of crepitation and/or clicking in the involved shoulder when in the appropriate position. On physical examination, patients with recurrent posterior shoulder instability frequently have a loss of internal rotation, particularly with the arm in 90 degrees of abduction. The grading of the amount of humeral head translation is important particularly in comparison to the contralateral shoulder. Instability is graded 1+ if there is increased translation relative to the other shoulder without subluxation of the humeral head; 2+ if the humeral head can be translated over the glenoid rim, but spontaneous reduction occurs; and 3+ if locking of the humeral head over the glenoid without spontaneous reduction occurs. A careful examination for elements of multidirectional instability should be performed in all patients, but particular attention should be paid to patients in whom posterior instability is diagnosed. Careful assessment should be made for generalized ligamentous laxity. Four parameters are frequently used: the degree of thumb hyperabduction with wrist flexion, the degree of index finger metacarpal phalangeal (MCP) joint hyperextension with wrist extension, the degree of elbow hyperextension, and the degree of knee hyperextension. Nonoperative measures, including an extensive exercise program focusing on the rotator cuff musculature, particularly as it pertains to resisting posterior subluxation, is valuable in helping to manage these patients. Pain is often the patient’s primary problem. Nonsteroidal antiinflammatory medications, activity restrictions, and an exercise program can often reduce or even alleviate the symptoms. However, the length of time that nonoperative measures should be continued in such patients must be individualized. In patients with findings compatible with multidirectional instability, or patients in whom low physical demands are required, an extensive nonoperative treatment program of 6 months or more should be carried out. Patients with traumatic posterior subluxation without evidence of multidirectional instability and with high activity levels, such as college athletes, are more likely to respond to surgical intervention. Nevertheless, even in these high-level athletes, exercise programs of 3 months or more are commonly carried out prior to surgical intervention. A number of open surgical stabilization procedures for recurrent posterior shoulder instability have been described. Arthroscopic techniques, which show some promise, have also been developed. However, no procedure has yet demonstrated a success rate comparable to techniques developed for recurrent anterior shoulder instability. This is most likely due to differences between anterior and posterior anatomy, as well as to differences between patients who develop posterior shoulder instability and those who develop anterior instability. The patient in the present case is a large, muscular, high-level athlete who places tremendous demands on his shoulder. In such a patient, an extensive capsular shift, with or without reverse Bankart repair, is likely to be required. The authors prefer to perform arthroscopy on all patients undergoing stabilization for posterior shoulder instability to assess for reverse Bankart lesions, to evaluate the quality of the posterior capsule and ligamentous structures, and to rule out any additional pathologies such as rotator cuff tearing. A decision is then made following arthroscopic evaluation and examination under anesthesia as to the best technique to affect repair and/or reconstruction. In patients with high degrees of posterior shoulder instability, the authors often perform a combination of arthroscopic and open stabilization procedures, which may include a combination of an arthroscopic reverse Bankart lesion repair, an arthroscopic rotator interval plication, and a limited, open posterior capsular plication. Another procedure combination commonly performed by the authors includes an arthroscopic rotator interval plication along with an open posterior lateral capsular shift, performed with or without a reverse Bankart lesion repair. PEARLS • Supplementation of the posterior capsulorrhaphy using a portion of the infraspinatus tendon can be valuable when posterior capsular and ligamentous structures are thin or poorly defined. • Arthroscopic plication of the rotator interval capsule serves as a valuable supplement to any posterior shoulder stabilization procedure. Plication of the rotator interval serves to significantly decrease both posterior and inferior glenohumeral translations.
History and Physical Examination
Differential Diagnosis
Radiologic Findings
Diagnosis
Surgical Management
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree