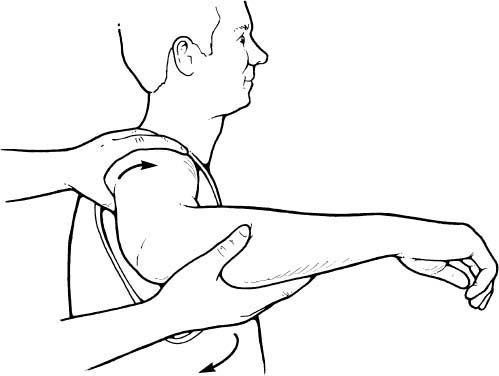
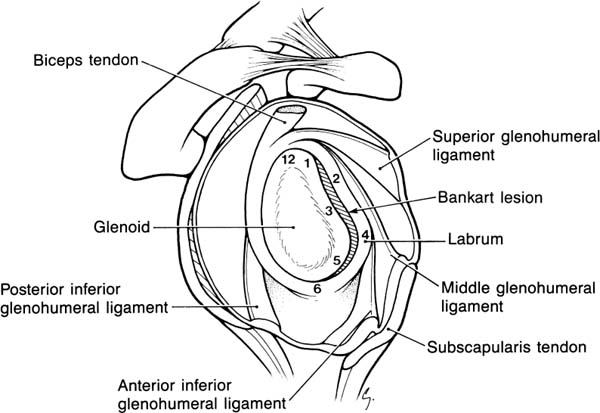
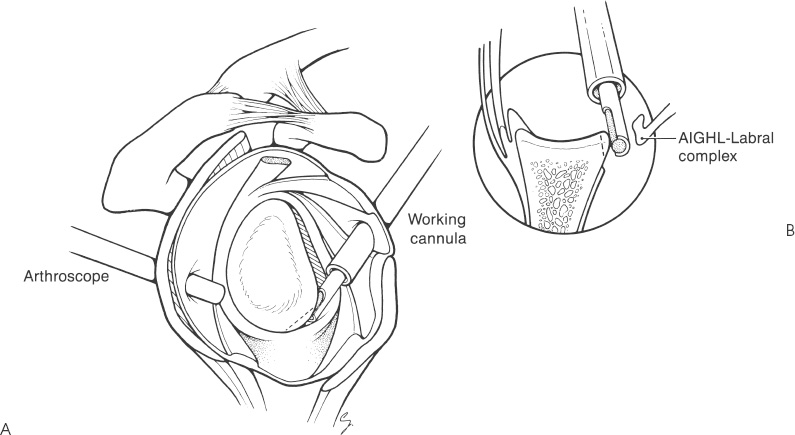
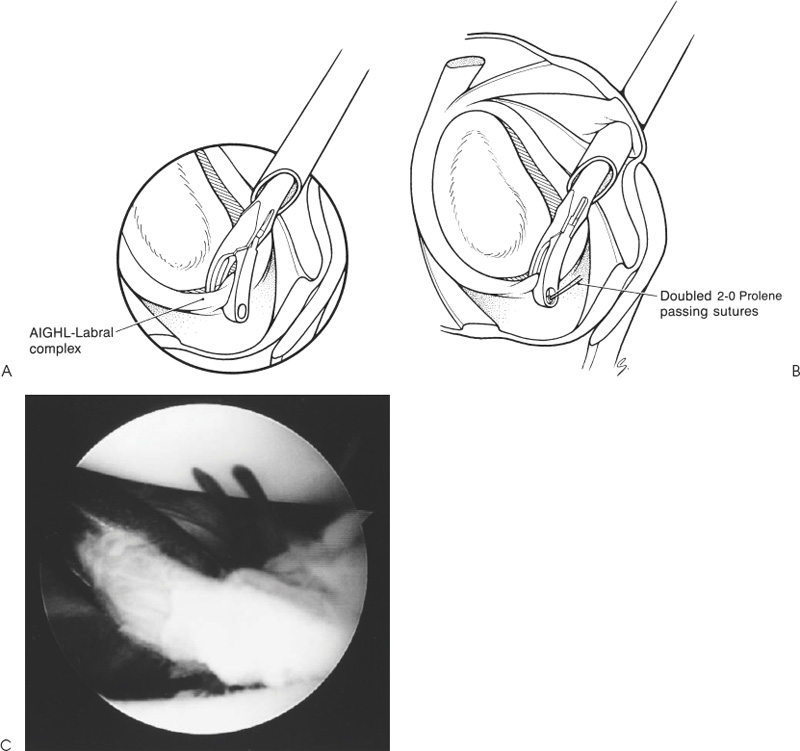
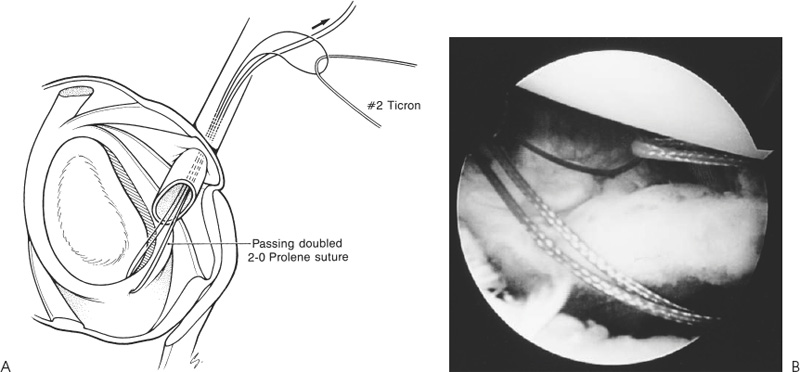
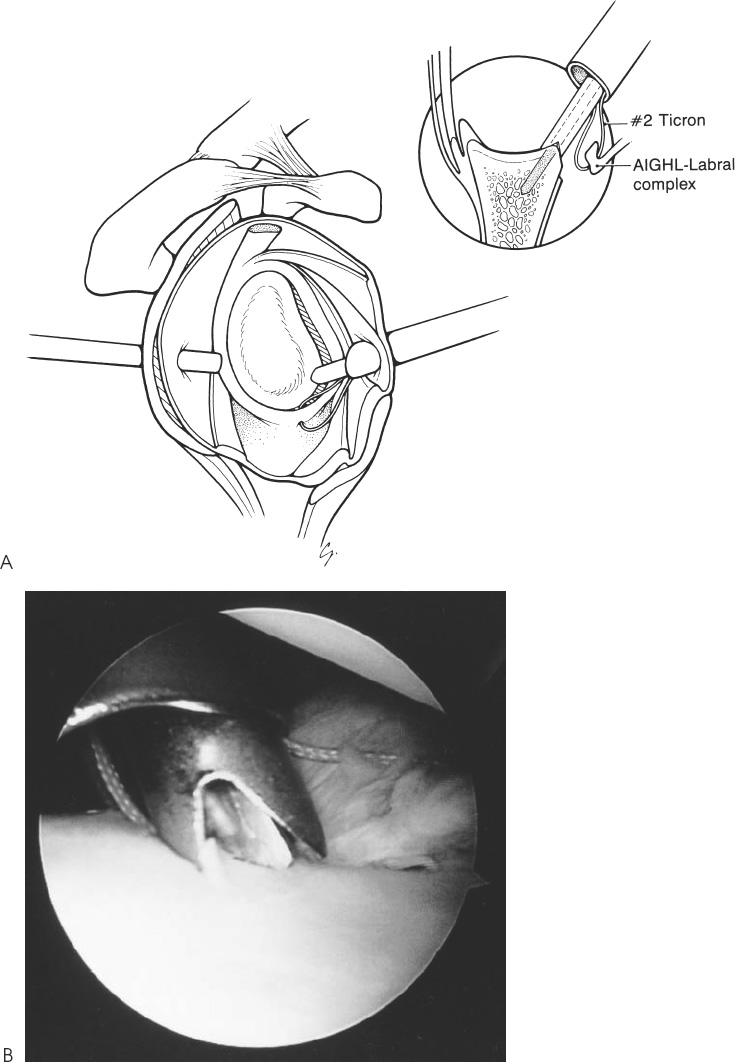
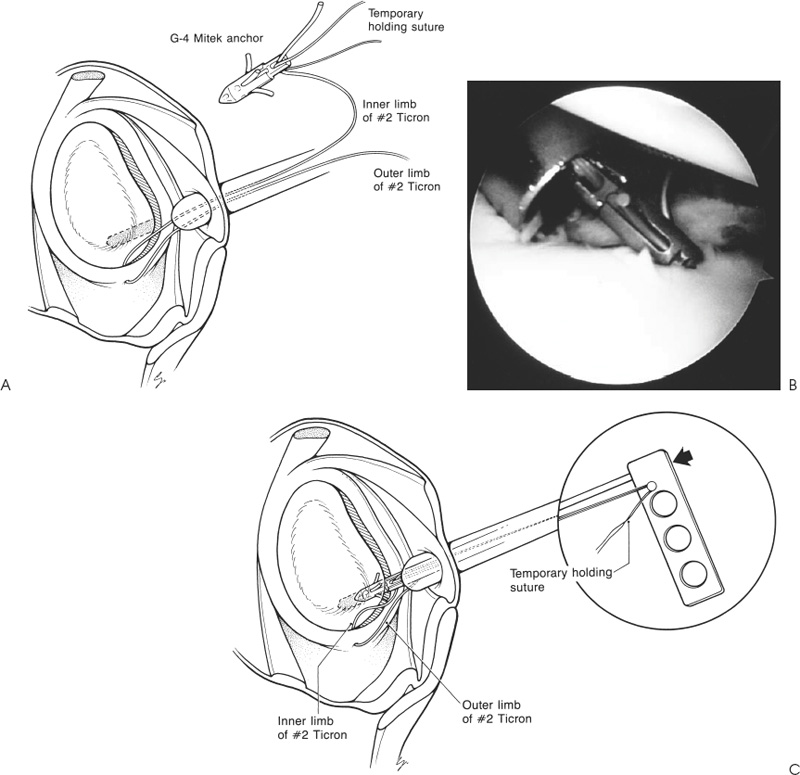
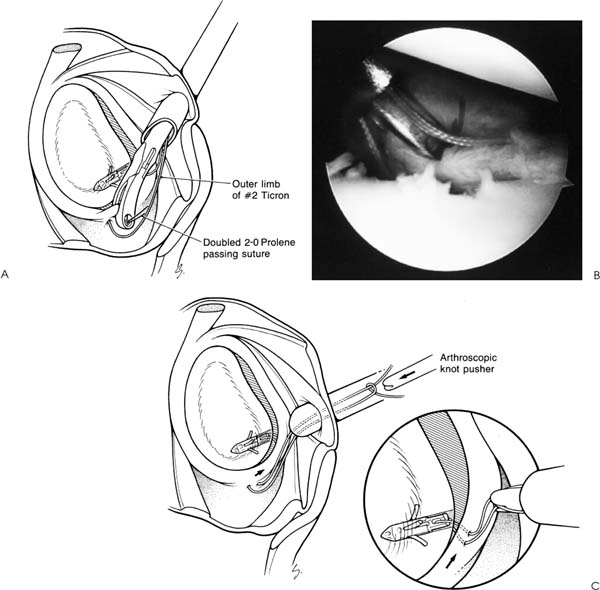
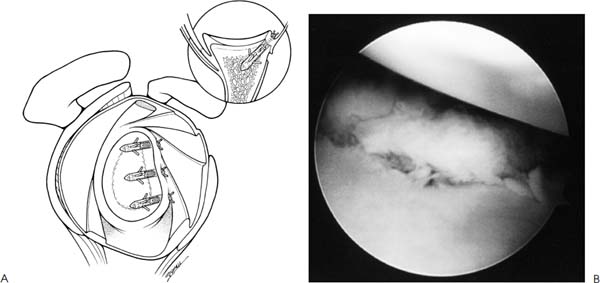
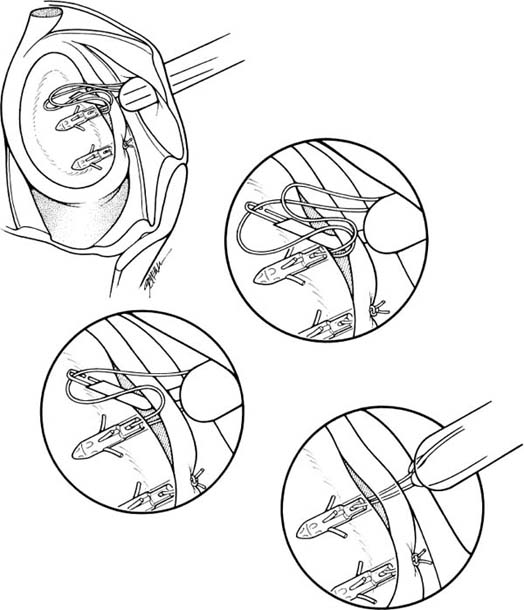
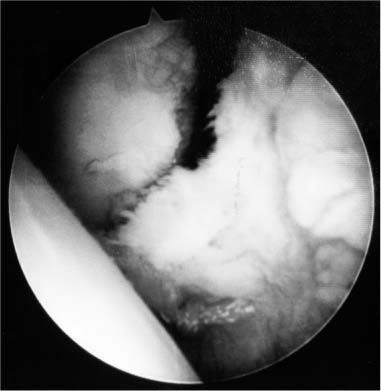
Case 12 A 19-year-old man presents 5 days following an injury to his shoulder while playing touch football. He reports an inability to use his arm because of pain in the shoulder and states that he had to have the shoulder reduced in the emergency room. He also reports a history of four previous episodes, all requiring reduction in the emergency room. He denies any numbness or other symptomatology. Range of motion of the shoulder is normal and strength testing demonstrates only a slight decrease with forward flexion. He is neurovascularly intact. Stability testing demonstrates 2+ increased anterior translation, normal posterior translation, and no sulcus sign. He demonstrates a positive apprehension test and positive relocation test. 1. Full-thickness rotator cuff tear 2. Recurrent anterior shoulder instability 3. Recurrent posterior shoulder instability An anteroposterior (AP), axillary view, and scapular Y view of the shoulder failed to demonstrate any obvious abnormalities. Recurrent Anterior Shoulder Instability. The patient’s history of recurrent dislocations requiring reduction makes the diagnosis straightforward. However, determining the direction of the instability is of great importance. A careful history should be obtained regarding the activities that result in shoulder dislocation and the position of the arm at the time of dislocation. Often, the patient will specifically relate the position of the arm that leads to dislocation of the shoulder. Although anterior shoulder instability is much more common than posterior instability, recurrent posterior shoulder dislocations do occur. A careful physical examination will also help to determine the direction of instability. Careful translation testing both anteriorly and posteriorly allows the physician an opportunity to assess the restraining function of the glenohumeral ligaments. Comparison with the opposite extremity is of paramount importance, as great variability exists in normal shoulder translations. However, some variability may exist between the shoulders of an individual without preceding injury or symptoms. Finally, provocative maneuvers such as the apprehension test and relocation test help in determining the direction of instability. Positioning the patient’s arm in maximum abduction and external rotation may reproduce a feeling of impending instability. Posterior translation of the humeral head during this test that alleviates the sense of apprehension is considered a positive relocation test. These are both excellent tests to evaluate for anterior instability if true apprehension is elicited during the exam. However, merely eliciting pain in the position of abduction and external rotation is much less sensitive for anterior shoulder instability and often results from rotator cuff pathology. Figure 12–1. Zone-specific loading of the glenohumeral joint aids in the determination of the specific instability pattern. The high likelihood of persistent, recurrent dislocations in this young, active man makes nonoperative measures unlikely to eliminate subsequent dislocations. The decision-making process centers around the operative technique best suited for such an individual. This patient has a very high likelihood of having a Bankart lesion identified at the time of surgery. If such a lesion is present, either arthroscopic or open techniques for repair are considerations. The choice of technique depends on a number of factors including the age and activity level of the patient, and the technical experience of the surgeon. Both an open Bankart repair and an arthroscopic repair can be challenging for the surgeon. Zone-specific load and shift maneuvers can be valuable in helping to rule out a multidirectional instability pattern and may influence the surgeon’s choice of operative technique. In zone-specific testing the examiner’s thumb is used as a fulcrum for loading the anterior stabilizing structures. To examine the right shoulder, the surgeon stands behind the patient. The surgeon’s left hand is used to stabilize the scapula, the left thumb is placed behind the humeral head, and the right hand, while the holding the patient’s flexed elbow, is used to load the joint (Fig. 12–1). Using this method the anterior-superior, direct anterior, and anterior-inferior components of stability can be individually evaluated. After adequate induction of general or interscalene regional anesthesia, the patient is placed in the standard lateral decubitus position rolled posteriorly 30 degrees. Alternately, the patient can be placed in the beach chair position. Stability testing is then performed to confirm the degree and direction of instability. With one hand, the examiner applies an axial load at the elbow to center the humeral head on the glenoid. The other hand is then used to translate the humeral head anteriorly and posteriorly. Grading is recorded as 1+ when increased translation is present compared with the opposite extremity but is insufficient to cause humeral head subluxation over the glenoid rim. An instability grading of 2+ is assigned when the examiner could subluxate the humeral head over the glenoid, but the head spontaneously reduces to its anatomic position when the force is removed. A 3+ grading signifies the ability of the examiner to lock the humeral head over the glenoid rim. Following an exam under anesthesia, a standard sterile prep and drape is then performed and the arm suspended with 10 to 15 pounds of traction in 45 degrees of abduction and 20 to 30 degrees of forward flexion, if the lateral decubitus position is employed. Figure 12–2. The Bankart lesion, and the positioning of anchors (1, 3, 5) and sutures (2, 4, 6). A posterior portal is initially established in the interval between the infraspinatus and teres minor tendons and a diagnostic arthroscopic examination performed. The presence of a Bankart lesion is confirmed and other pathology noted. A second portal is established anteriorly utilizing an outside-in technique to ensure proper positioning of this anterior portal. The portal should be established so that the surgeon will have access at a proper angle in three planes to the glenoid rim for anchor placement at the 1, 3, and 5 o’clock positions, as well as access to the anterior and inferior capsulolabral ligamentous complex for suture placement at the 2, 4, and 6 o’clock positions (Fig. 12–2). Localization with a spinal needle prior to placement of the cannula ensures adequate placement. A cannula for instrumentation is then inserted into the joint at the upper edge of the subscapularis tendon running through the lower aspect of the rotator interval, just lateral to or above the middle glenohumeral ligament. The labral edge is debrided of degenerative tissue, and the capsulolabral ligamentous complex is completely released from the glenoid neck down to the 6 o’clock position (Fig. 12–3). A high-speed burr is then used to abrade the anterior and inferior glenoid neck down to the 6 o’clock position. The debridement and abrasion are necessary to allow an adequate vertical shift of the damaged capsulolabral structures and adequate healing of the repair once the reconstruction is completed. Often the avulsed labrum has healed or partially healed medially on the glenoid neck. Extensive freeing of the labrum in this area must be performed to allow adequate mobilization. This may be accomplished with rasps, shavers, burrs, or knives. Figure 12–3. (A) The capsular release and glenoid neck abrasion are taken to the 6 o’clock position inferiorly. (B) The notchplasty abrader is taken across the anterior glenoid down to the 6 o’clock position. A nonmodified Caspari suture punch (Linvatec) is then inserted through the anterior portal. A 48-inch doubled 2.0 Prolene suture (Ethicon) is loaded with the two free ends passed into the suture punch and the loop portion remaining proximally (Fig. 12–4A). The suture punch is inserted into the joint and used to pass this double suture through the inferior glenohumeral ligament, lateral to its labral attachment, at approximately the 6 o’clock position (Fig. 12–4A,B). The suture punch is withdrawn, pulling both the free ends and the loop end outside of the same cannula. A no. 2 Ticron suture is then placed in the loop. By pulling on the two free ends the suture is passed through the inferior glenohumeral ligament (Fig. 12–5). The drilling guide is placed into the joint through the suture punch cannula. The first or inferior hole is drilled at the edge of the glenoid articular surface at approximately the 5 o’clock position. The guide tip is wedged onto the glenoid neck-face junction and fulcrumed downward against the soft tissues so that the drill is perpendicular to the vertical axis of the glenoid (Fig. 12–6). The pilot hole is drilled, maintaining adequate visualization from the posterior portal. While visualizing from the posterior portal, it is critical that the drill hole is placed with at least half the diameter of the hole into the edge of the articular surface of the glenoid, thereby assuring optimal anchor placement. The anchor is loaded on the inserter and held in position with an absorbable 2-0 Vicryl suture. The inner limb of the Ticron suture is threaded through the anchor and the anchor inserted into the previously drilled pilot hole (Fig. 12–7). The anchor is carefully tested by pulling on the 2-0 Vicryl suture, which is removed after adequate holding power is confirmed. The suture punch is reinserted into the joint and a second doubled Prolene placed through the inferior glenohumeral ligament approximately 5 mm more superiorly than the initial suture (5:30 to 5:45 clock position). This Prolene is used to pull the inner limb of the Ticron suture through the inferior glenohumeral ligament, creating a horizontal mattress suture and allowing capsular plication (Fig. 12–8A,B). An arthroscopic knot tying device is used to tie the two ends of the Ticron suture, repairing the inferior glenohumeral ligament to the glenoid, while advancing it superiorly. This will eliminate inferior capsular redundancy (Fig. 12–8C,D). Figure 12–4. (A) The suture punch is used to thread a 48-inch doubled 2-0 Prolene suture through the inferior glenohumeral ligament complex at approximately the 6 o’clock position. (B,C) The suture punch positioned on the inferior capsule as it is pulled superiorly. The two strands of the 2-0 Prolene suture are then threaded into the glenohumeral joint. (See Color Plate 12–4C.) Figure 12–5. (A) The doubled 2-0 Prolene suture is used to retrieve a no. 2 Ticron braided nonabsorbable suture through the inferior glenohumeral ligament complex. (B) The Prolene can be seen pulling the no. 2 Ticron suture through the inferior glenohumeral ligament and back out the anterior cannula. (See Color Plate 12–5B.) Figure 12–6. (A) The drill guide is placed on the glenoid neck-face junction at approximately the 5 o’clock position. It should be placed so that approximately half the diameter of the drill is on the articular surface, as illustrated in the inset. (B) In this view from the posterior portal, the drill guide and drill can be seen in position for the 5 o’clock anchor placement. (See Color Plate 12–6B.) Figure 12–7. (A) The inner limb of the no. 2 Ticron is passed through the Mitek G4 anchor, along with a 2-0 Vicryl suture. The Vicryl is used to hold the anchor onto the guide. (B) The Mitek G4 anchor is inserted into the drill hole previously made in the glenoid neck. (See Color Plate 12–7B.) (C) The anchor is tapped into position. Figure 12–8. (A) The suture punch with a second doubled 48-inch 2-0 Prolene passing suture is placed through the inferior glenohumeral ligament complex approximately 5 mm superior to the no. 2 Ticron. (B) The outer limb of the no. 2 Ticron suture can be seen passing through the inferior glenohumeral ligament complex and out the anterior cannula while the inner limb comes directly from the anchor and out the cannula. The doubled 2-0 Prolene suture is exiting the suture punch through the inferior glenohumeral ligament complex. This Prolene is used to retrieve the inner limb of the Ticron through the inferior glenohumeral ligament complex. (See Color Plate 12–8B.) (C) Once the two limbs of the Ticron are retrieved through the inferior glenohumeral ligament complex, the sutures can be tensioned, shifting the capsule superiorly and plicating the inferior glenohumeral ligament complex. Standard arthroscopic knot tying techniques are used to secure the capsulolabral ligaments to the anterior glenoid neck. (D) In this anterior view the initial suture knot as the most inferior aspect of the reconstruction can be well visualized. (See Color Plate 12–8D.) Each step is then repeated, inserting a second and third anchor in similar fashion (Fig. 12–9). The sutures are generally placed at the 6, 4, and 2 o’clock positions into the capsule, with the anchors inserted at the 5, 3, and 1 o’clock positions on the glenoid rim (Fig. 12–2). Placing the sutures inferior to the anchor allows a superior shift of the capsule, eliminating inferior redundancy and correcting any plastic deformity that may exist in the capsular or ligamentous tissues. Mattressing the suture allows plication of the capsule and helps eliminate redundancy. Figure 12–9. (A) In most cases three anchors are inserted into the glenoid neck, shifting the capsule superiorly and repairing the avulsed capsulolabral structures to the glenoid. (B) This view from the posterior portal demonstrates the repaired capsulolabral complex, restoring a normal buttress in the anterior aspect of the shoulder. (See Color Plate 12–9B.) An alternative method allows placement of the anchor into the glenoid first, followed by retrieval of both limbs of the suture through the capsule. This technique is utilized for preloaded anchors or those with eyelets of insufficient width to allow two sutures (holding suture and repair suture) to be placed into the anchor simultaneously. In this variation the 5 o’clock hole is placed and the anchor with attached no. 2 nonabsorbable suture is inserted into the glenoid. The suture punch is used to place a doubled 40-inch, 2-0 Prolene passing suture through the capsule at the 6 o’clock position. The Prolene is used to retrieve one limb of the Ticron through the capsule and out the cannula. The suture passing step is then repeated to create a mattress suture, thereby shifting the capsule superiorly and simultaneously plicating it. These strategies are then repeated for the 3 and 1 o’clock anchors. As an alternative to the above techniques, the Ticron sutures of the 3 o’clock and 1 o’clock anchors can be pulled through the labrum with a retrograde suture retriever (Innovasive Devices) (Fig. 12–10). This is accomplished by placing the 15-, 30-, 45-, or 60-degree suture retriever through the anterior cannula and then passing it through the labrum at the same location described for the Caspari punch. This will reproduce the horizontal mattress suture and capsular plication required for the repair. This device simplifies the suture passing, but is unable to efficiently reach the 6 o’clock position on the labrum required for the inferior suture. Harryman and colleagues (1992) have shown that the most secure knot configurations are achieved by reversing half-hitch throws while alternating the post (Fig. 12–11A). Using this technique, five throws are recommended. A modified slipknot, called the Roeder knot, can also be used. The authors prefer a modification of the Roeder knot; it is accomplished by throwing the first half of a square knot leaving one end long and one end short (Fig. 12–11B). The long end is then passed around both limbs of the suture three times, then once around the short limb. The long limb of the suture is then passed through the loop adjacent to the half square knot (Fig. 12–11C). The knot is then compressed by spreading the distal limbs while holding the short limb as a post (Fig. 12–11D). The knot is advanced by pulling on the short limb. It is imperative that the long limb is not pulled until the knot is snug against the soft tissues and has approximated the Bankart lesion, because this will lock the knot. The knot is then secured by at least one single half hitch using the short limb as a post. Once the repair is completed, the shoulder is tested for adequate stability while visualizing the glenohumeral articulation from both the anterior and posterior portals. Specific attention is directed toward any laxity of the posterior-inferior gleno humeral ligament and rotator interval. In most cases in which the above technique has been performed correctly, there has been no laxity posteriorly. Figure 12–10. Alternate method of passing suture through the labrum for the 3 o’clock and 1 o’-clock anchors using the 30-degree suture retriever (Linvatec). The importance of the rotator interval in shoulder instability has been established in cadaveric and clinical reports. Arthroscopic plication of the rotator interval is sometimes carried out after arthroscopic Bankart repair to supplement the labroligamentous reapproximation. The rotator interval may be plicated by one of two methods. Maintaining the arthroscope in the posterior portal, a transporter or suture retrieval device is inserted through the capsule adjacent to the subscapularis tendon and through the middle glenohumeral ligament. Occasionally a small portion of the subscapularis may be included in this repair, but it is important to include the capsule anterior to the subscapularis as well as a portion of the middle glenohumeral ligament. A spinal needle is then placed through the skin in the area of the anterior-superior portal, adjacent to the anterior-lateral corner of the acromion, and through the capsule adjacent to the anterior margin of the supraspinatus tendon. A no. 1 Pro lene suture is then passed through the spinal needle and retrieved out the anterior portal, using the transporter device (Fig. 12–12). This suture will close or plicate the more lateral portion of the rotator interval. The transporter can then be placed back down the anterior cannula and through the capsule medial and superior to the first stitch, allowing passage of a second or third stitch as needed. PEARLS • Adequate abrasion of the anterior and inferior glenoid neck is important in encouraging a healing response following capsulolabral reapproximation. • Superior advancement of the anterior and inferior capsulolabral structures is key in retensioning the complex and providing adequate postoperative stability. Inferior placement of the suture through the capsulolabral tissue at the 6 o’clock position allows for superior advancement of these tissues with suturing. • Placement of the suture anchors at the articular cartilage margin of the glenoid, as opposed to more medially on the glenoid neck, allows for reap-proximation of the labral tissue over the articular rim of the glenoid. This serves not only to properly retension the ligaments, but also to provide an effective bumper or “door-stop” effect to reduce anterior translation and reestablish articular cartilage cohesion. • Arthroscopic rotator interval plication may help to supplement and “off load” the capsulolabral repair. It is routinely carried out by the authors at the time of arthroscopic Bankart repair.
History and Physical Examination
Differential Diagnosis
Radiologic Findings
Diagnosis
Surgical Management
Suture-First Technique
Anchor-First Technique
Alternate Technique for 3 and 1 o’clock Anchors
Knot Tying
Rotator Interval Closure
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree