Chapter 61 Disorders of the Patellofemoral Joint
Basic Anatomy and Biomechanics
Patellar shape, however, is not constant. Three different patellar types have been described by Wiberg,110 and a type 4 was later described by Baumgartl, the “Jaegerhut” patella, with no medial facet and consequently no median ridge (Fig. 61-1).
A rich arterial plexus supply is present. A complex vascular anastomotic ring lying in the thin layer of loose connective tissue that covers the dense fibrous rectus expansions surrounds the patella. Six main arteries compound this ring. Two intraosseous systems were described by Scapinelli93: the mid patellar vessels, which enter the vascular foramina situated in the anterior surface; and a second system, which arises from the polar vessels, from the anastomosis behind the patellar ligament. Later, Bjorkstrom8 described vessels entering from the quadriceps and from the medial and lateral retinacula.
The TG deepens distally, and some controversy still exists regarding its orientation. If its deepest points are taken into account, the natural TG is most often aligned so that it deviates distally and laterally in relation to the femoral shaft axis.97
The quadriceps muscle is formed by four parts: rectus femoris, vastus medialis, vastus lateralis, and vastus intermedius. These muscles converge to a tendon 5 to 8 cm superior to the patella. Fibrous expansions arise from the vastus lateralis and medialis, blending with the lateral and medial retinacula, respectively. The most inferior part of the vastus medialis is known as the vastus medialis obliquus (VMO) and inserts in the patella at a mean of 47 ± 5 degrees from the femoral axis in the coronal plane.34 Similarly, a vastus lateralis obliquus can be described, with a more vertical orientation (35 ± 4 degrees).
The patellar tendon arises from the inferior pole of the patella. Its average length is 4.6 cm (3.5 to 5.5 cm), and its width is between 24 and 33 mm.87 It inserts in the tibial tubercle, which usually is a little lateralized in relation to the long axis of the tibia; thus the distal orientation of the patellar tendon is also lateralized (valgus). The posterior part of the patellar tendon is separated from the synovial membrane of the joint by the infra-patellar fat pad, and from the tibia, more distally, by a bursa.
Medially, the retinacular expansion of the vastus medialis merges with layers 1 and 2. Other portions of the middle layer persist as a separate layer, forming the medial patellofemoral ligament (MPFL), below the deep fascia and superficial to the joint capsule. The MPFL runs transversely from the patella to the femur. Some controversy exists about its femoral insertion, but it seems reasonable to define it as near the medial epicondyle, just proximal and posterior to it, distal to the adductor tubercle. The patellar attachment is wider than the femoral one, extending from the proximal and medial corner of the patella over approximately half of its length.5 The mean length of the MPFL is 53 to 55 mm, and its width varies between studies, ranging from 3 to 30 mm and widening at its attachments.5,19,87,106 As it approximates the patella, it is overlaid by the distal part of the VMO, and some of its fibers merge into the deep aspect of the muscle. Other bands with secondary functions have been described that link the patella to the tibia and the medial meniscus.
The patella increases the moment arm of the extensor mechanism. It concentrates the tension of the converging quadriceps fibers and transmits it to the patellar tendon. In complete extension, a coronal result is produced, and no sagittal forces are expected (this is not completely true, as the retinacula exert some posterior displacement forces in the patella when the knee is near extension). As the knee flexes, however, a posteriorly directed force vector becomes clear, and this raises the patellofemoral joint reaction force. The greater the degree of flexion, the greater is the resultant force vector53 (Fig. 61-2).
Also in the coronal plane, multiple quadriceps insertions should be noted, along with their different angles of action. The VMO and the vastus lateralis obliquus (VLO) mainly act in an oblique manner in relation to the longitudinal direction. Based on this, malfunctioning of one (VMO) or hyperfunctioning of the other (VLO) can cause coronal displacement and, to a greater extent, instability. If the force-producing capacity of each muscle head is proportionate to its cross-sectional area, the VMO could contribute 10% to total quadriceps tension, and if completely relaxed, it can cause tension to swing laterally to approximately 6 degrees34 (Fig. 61-3).
Soft tissue restraints also play a fundamental role in coronal plane force balance. In complete extension, normal patellae are not engaged in the trochlear groove. This engagement starts at approximately 20 degrees of flexion, when the distal and lateral part of the patella touches the upper and proximal part of the trochlea, which comprises the lateral facet. Because the patella is not engaged before this point, only soft tissue stabilizers act to ensure its coronal location. On the lateral side, the retinaculum is directly linked to the ITB, and tension in the ITB causes the patella to track in a more lateral direction.63 On the medial side, the MPFL contributes 50% to 60% of the restraint to patellar lateral displacement at 0 to 20 degrees of flexion, with a mean failure load of 208 N.5,79 Although MPFL insufficiency is not the cause of lateral dislocation, one cannot assume lateral dislocation without its insufficiency or rupture.
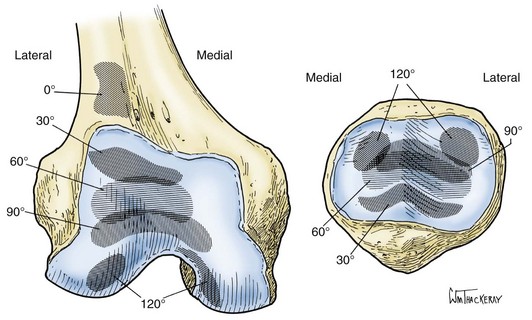
With initial patellofemoral contact, as a result of the articular surface orientation, a medial patellar shift is produced when the patella engages and follows the trochlear groove. As the flexion angle of the knee is increased, the contact area of the patella progresses proximally, while the trochlear contact area progresses distally. From extension to 90 degrees of flexion, the patella holds the quadriceps tendon away from the femur, but with additional degrees of flexion, an extensive area of contact is formed between the tendon and the trochlea. At between 90 and 135 degrees of flexion, the patella rotates and the ridge that separates the medial and odd facets engages the femoral condyle. At 135 degrees, separate lateral and medial (limited to the odd facet) contact areas are formed40,41 (Fig. 61-4).
Patellofemoral Disorders: Analysis
Clinical Symptoms
Physical Examination
With the patient supine and the hips and knees extended, the Q angle measurement can be done effectively. Care should be taken because a laterally displaced patella will cause underestimation of its value. Knee flexion can correct this by bringing the patella into the center of the trochlear groove, but no agreement has been reached on the best Q angle measurement method (flexion or extension), or even on its applicability.99 Normal individuals, in general, will not present with values greater than 20 degrees.
Imaging
X-ray Analysis
AP View
The anteroposterior (AP) view must be done in monopodal stance as long as the patient is able to do so. In younger patients (before 50 years old), it should be performed in 15 to 20 degrees of flexion; in older patients and in those who have antecedents of knee trauma or surgery, it should be done in 30 or 45 degrees of knee flexion (Schuss or Rosenberg). The AP analysis is not really helpful for patellofemoral problems. It will allow bone quality analysis, alignment assessment, and evaluation of femorotibial-associated pathology or arthritis. Gross patellar instability or displacement (Fig. 61-7) can also be observed in this view, along with malformations such as bipartite patella or fracture. A loose body in the lateral gutter may be found, representing a lateral condyle fracture that occurred during patellar dislocation.
In the AP view, we can observe a bipartite or a multipartite patella. It is the result of incomplete fusion of an ossification center and is described to have a frequency between 0.005% and 1.66%.10,102 The accessory fragments commonly are located close to the superolateral border. The edges of the fragment are smooth, and this allows differentiation from fracture. Bipartite or multipartite patellae are often bilateral.
Lateral View
Trochlea
In a normal knee, Blumensaat’s line is continued anteriorly by the trochlear groove line, which should stay posterior to the projection of the femoral condyles (facets). In 1987, Henri Dejour described the crossing sign, which characterizes trochlear dysplasia on the sagittal view. The crossing point represents the exact location where the deepest point of the trochlear sulcus reaches the same height as the femoral condyles, meaning that the trochlea becomes flat in this location (Fig. 61-8).
The position of the trochlear sulcus line is abnormal in relation to the anterior femoral cortex. In a study performed by Dejour and associates,30 in normal knees the trochlear sulcus line was at a mean distance of 0.8 mm posterior to a line projected from the anterior femoral cortex, and in those knees with dysplastic trochleae its mean position was 3.2 mm forward to the same line. This increases the contact force between the patella and the trochlea (anti-Maquet effect) (Fig. 61-9).
The crossing sign has been found in 96% of the population with antecedents of true patellar dislocation, and in only 3% of healthy controls.29 The first published classification (Henri Dejour) divided dysplasia into three grades, according to the level of the crossing sign. Other noted signs included the following: (1) the deepness of the trochlea as measured by a line that traced 15 degrees from another one perpendicular to the femoral shaft and tangential to the posterior condyles (see Fig. 61-9), and (2) the “bump,” which was defined as the distance between a line drawn tangential to the anterior femoral cortex and the highest point of the trochlea.
The classification in three grades has some limitations, as was corroborated by the work of Remy and colleagues.89,90 They showed that interobserver reproducibility of trochlear analysis was low, especially for type II dysplasia. This led to a new study performed in 1996 by Dejour and Le Coultre, which analyzed 177 cases of patellar instability and included radiographs along with preoperative and postoperative CT scans. Based on this analysis, a new and more precise classification with four grades of trochlear dysplasia was defined.26,28 Two new signs were added to the crossing sign. The first is the supratrochlear spur, which represents a global prominence of the trochlea and plays a role similar to a ski jump when the patella engages the trochlea. The second sign is the double contour, which is the radiographic line that ends below the crossing sign and represents the subchondral condensation of the hypoplastic medial facet on the lateral view. In 2002, the Lillois group conducted a new interobserver study91 and concluded that “this new classification system is more reproducible than the former 3-type system proposed. The crossing sign and the supratrochlear spur are the most reproducible signs” (Fig. 61-10).
This classification system (Figs. 61-11 and 61-12) is based mainly in the lateral view, although CT may assist in differentiation between types. Four types, based on the three dysplastic signs described, are included:
Patella
Grelsamer et al44 did a study describing three types of patella, based on the ratio between the length of the patella and the length of the articular surface. Most patellae exhibit a ratio between 1.2 and 1.5 and are classified as type I. Those with a ratio greater than 1.5 give the appearance of having a long nose; this is type II. Those with a ratio less than 1.2 (short nose) are type III (Fig. 61-13).
The shape of the patella on the lateral view is correlated with the tilt and with the global morphology of the patella. In a normal patella, with no tilt, the most posterior part visible in the lateral view should be the median longitudinal ridge. The lateral facet projection is located slightly anterior. In tilted patellae, these relations are lost, and the overall anteroposterior size of the patella appears increased (Fig. 61-14).
The tilt evaluation has been described by Maldague and Malghem.69 Three positions are described: normal position, in which the lateral facet is in front of the crest; mild tilt, in which the two lines (lateral facet and crest) are on the same level; and severe tilt, which shows the lateral facet behind the crest (Fig. 61-15).
Patellar Height
Axial View
The axial view has been described at different angles of knee flexion and different positions of the x-ray cassette. Our common approach is to perform 30-degree axial views as described by Ficat, who also described axial views at 60 degrees and 90 degrees (Fig. 61-19). Radiographs are obtained with the knee flexed over the edge of the table, the beam directed proximally, and a perpendicular cassette in place. Images beyond 45 degrees of flexion, however, are less informative as they show the lower part of the trochlea and the patella as fully engaged, many times correcting tracking abnormalities (Fig. 61-20). These high–flexion angle images are not necessary.23 Lower flexion angles, although capable of showing better the maltracking signs, are technically demanding and at times impossible. With a well done image, one can assess the relation between the femoral trochlea (at 30 degrees, the lateral facet should appear with two-thirds total trochlear width) (Fig. 61-21) and the patella (with the lateral facet also composing two thirds). Tilt, congruence, and cartilage thickness can also be appreciated.
Alternative methods have been proposed. The main choices are discussed in the following sections.
Merchant View76
Laurin View64,65
Malghem and Maldague Lateral Rotation View (30 Degrees LR)70
In acute or chronic patellofemoral instability, medial patellar avulsions (Figs. 61-27 and 61-28) can be demonstrated and should not be confused with bipartite patella. Other important data provided by axial views include patellar shape and joint line thickness. Patellar shape is evaluated according to Wiberg’s classification (Fig. 61-29). Joint space thickness is diminished in arthritis. Axial views at 30 degrees allow assessment of which side of the articulation is affected (usually the lateral side). Information on the size of osteophytes and on joint line narrowing is provided. Iwano and coworkers57 used the following simple staging system of lateral patellofemoral osteoarthritis (OA) (Fig. 61-30):
Computed Tomography
Many parameters observed in CT images are similar to those observed in axial views. The contribution of CT in this aspect, however, is its ability to produce such images in complete extension and perform measurements. This is particularly helpful when patellofemoral tilt or subluxation is considered, because flexion of the knee causes the patella to engage the trochlear sulcus, thus correcting (or at least reducing) these abnormalities55,95 (Fig. 61-31). CT also provides a constant reference for measures: the posterior femoral condyles, otherwise not visualized in axial views.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree