Degenerative Joint Disease of The Ankle and Hindfoot
Todd A. Kile
Christopher Y. Kweon
Degenerative joint diseases include various clinical entities that are all linked by their common pathologic finding: the destruction of the joint interface. The ankle and the different hindfoot joints can be affected separately or in combination depending on the etiology (Fig. 10.1). Review of the degenerative joint diseases that affect the ankle and hindfoot is made easier by separating these entities using biomechanical and anatomic criteria.
This chapter highlights the important concepts needed to understand ankle degenerative joint disease. The second section discusses the hindfoot. Finally, this chapter presents some of the unique principles regarding combined lesions of the hindfoot and ankle joints.
ANKLE DEGENERATIVE JOINT DISEASE
The ankle joint combines the functions of a weight-bearing surface and allows motion that permits a normal gait cycle. The tibiotalar portion of the ankle joint transmits approximately 80% of the forces crossing the ankle. Shear forces coupled with compression forces are transmitted through this articulation. Compressive forces reach up to five times the body weight at heel rise. Shear forces reach up to 70% of body weight during flatfoot phase. As a result, the cartilage surfaces play a central role in the function of the joint. These surfaces are protected by two primary stabilizing mechanisms: the bony architecture surrounding the talus, shaped in a mortise, and the ligamentous support linking the distal tibia and fibula to the hindfoot. The destruction of either of these mechanisms by a degenerative process of the ankle joint creates unique clinical and radiologic findings, which, when recognized and understood, may help direct both nonsurgical and surgical treatments for patients affected by this disease.
PATHOGENESIS
The commonest cause of degenerative joint disease in the ankle is trauma. Ankle fracture, tibial plafond fracture, talus fracture, chondral trauma, and residual instability represent various pathways that can lead to degenerative arthrosis of the ankle joint. In these cases, the initial trauma is followed by a cascade of events, with all the biochemical and biomechanical changes that occur, leading ultimately to destruction of the joint cartilage.
Systemic diseases can result in ankle degeneration (Box 10.1), but they are less common. Among the inflammatory etiologies, rheumatoid arthritis is the most prevalent with its classic inflamed lymphoid follicles creating the pannus responsible for cartilage and subchondral bone destruction. Psoriatic arthritis can also affect the ankle joint as well as the surrounding skin and soft-tissues.
Metabolic crystalline arthropathies, such as gout or pseudogout, can cause acute and recurrent arthritis of the hindfoot and ankle. These flares, left untreated, can lead to eventual joint destruction. The inflammatory mediators, together with the hypertrophic synovium, cause irreversible injuries to the articular surface. The same kind of destructive pattern can occur in septic arthritis and osteomyelitis, which can cause degenerative joint disease in any joint affected by this condition. Proteolytic enzymes combined with increased intra-articular pressure and lack of nutrition ultimately lead to destruction of the cartilage.
Neuroarthropathy represents a characteristic condition, often confused with infection, which can result in destruction and deformity of the joints. Although the exact pathophysiology is not well understood, it is believed that the loss of protective sensation combined with unrecognized trauma (often subclinical or microtrauma) generates damage that is not adequately protected. This begins a cascade of clinical events—which can be seen radiographically—that can progress to dramatic bone and joint destruction. Diabetes mellitus, nerve and spinal cord
dysfunction (paralytic injury or trauma), and myelodysplasia represent additional causes of neuroarthropathy at the foot and ankle levels. Interestingly, congenital insensitivity to pain can create similar problems, but remains an unusual clinical entity and seldom leads to destruction of joints.
dysfunction (paralytic injury or trauma), and myelodysplasia represent additional causes of neuroarthropathy at the foot and ankle levels. Interestingly, congenital insensitivity to pain can create similar problems, but remains an unusual clinical entity and seldom leads to destruction of joints.
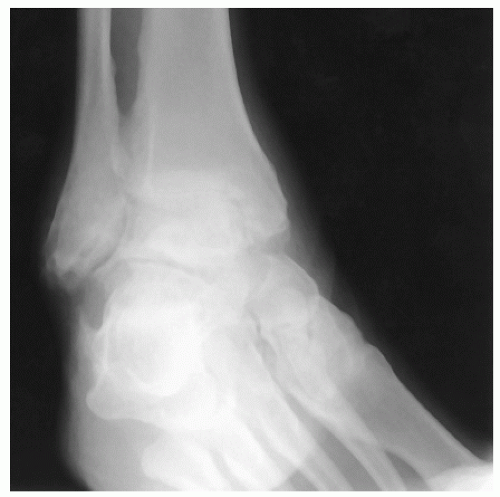 Figure 10.1 Oblique ankle X-ray of a 51-year-old man who shows posttraumatic ankle and subtalar degenerative joint disease. |
Hemorrhagic effusions secondary to hemophilia or chronic warfarin therapy can also cause progressive articular destruction. In hemophilia, recurrent hemarthroses create a chronic inflammatory state of the synovium that can eventually affect the integrity of the joint itself by an enzymatic digestion process. Degeneration from septic arthritis and a similar inflammatory and degradative process is also well described.
Other causes of joint degeneration include bone or softtissue tumors of the ankle area, iatrogenic trauma, or primary idiopathic degenerative joint disease of the ankle—a diagnosis made by exclusion.
DIAGNOSIS
Physical Examination and History
Despite significant technologic advances in imaging, a complete history remains the most important diagnostic tool when evaluating patients with joint pain. Details regarding any of the possible etiologies previously discussed can be determined and may influence treatment options. Previous trauma should be explored thoroughly because it is the most frequent cause of degenerative joint disease of the ankle. The patient’s age, occupation, level of activity and autonomy, and past medical and surgical history as well as other joint involvement are important. When surgery is considered, the patient’s discontinuation of tobacco use may help to reduce wound or bone healing problems, particularly because decreased fusion rates have been identified in smokers.
Ankle osteoarthritis usually presents with pain and mechanical symptoms at the anterior aspect of the ankle joint.
Pain, which is increased with weight bearing and decreased with unloading, is the most common presenting complaint.
Morning pain and stiffness on arising or start-up pain is common.
Previous treatments such as shoe modifications, orthotics, braces, medications, and changes in activity and their results should be reviewed.
Neuroarthropathy represents a unique situation in which the patient may notice the appearance of swelling, deformity, and instability associated with relatively little pain at the level of the ankle.
Clinical Findings
The ankle joint examination is similar to that for other major weight-bearing joints.
A complete examination includes gait analysis, inspection, palpation, neurovascular evaluation, active and passive ranges of motion of the ankle and the adjacent joints, strength testing, and ligament stability evaluation.
This examination should be compared with the contralateral lower limb findings.
Gait analysis in the presence of ankle degeneration reveals a decreased velocity and stride length. An antalgic gait pattern is frequently observed.
Weight-bearing evaluation reveals the clinical magnitude of any deformity.
Ankle degenerative joint disease commonly presents with decreased range of motion at the ankle joint and usually reproduces the patient’s pain.
Normal sagittal motion ranges from 25° of dorsiflexion to approximately 30° of plantarflexion rotating about an axis crossing the tip of the medial and the lateral malleoli.
Because this approximated axis of rotation is relatively oblique compared with the longitudinal axis of the leg, ankle dorsiflexion is associated with external rotation and plantarflexion with internal rotation of the foot.
Tendon function and muscle strength are assessed to provide a more complete understanding of the patient’s limitations.
Ligament stability on both the medial and the lateral aspects of the ankle is assessed functionally on examination as well as radiographically, if necessary.
Radiographic Findings
Degenerative joint disease of the ankle is best visualized using standardized weight-bearing plain X-rays.
The degree of joint degeneration can be underestimated when the X-ray is performed non—weight bearing.
Most institutions use weight-bearing X-rays to ensure a more accurate measurement of the extent of cartilage involvement and to provide a more dynamic picture of the status of the ankle and hindfoot joints (Fig. 10.2).
Three views—the anteroposterior (AP), lateral, and mortise—of the ankle joint are usually sufficient to reveal the majority of pathologies related to degenerative joint disease of the ankle.
Positive findings should be correlated with clinical findings.
The radiographic signs most commonly associated with osteoarthritis include the following:
Joint space narrowing
Subchondral sclerosis
Cysts
Osteophytes
Other radiographic findings may depend on the etiology that led to the degenerative joint disease, such as gout or rheumatoid arthritis.
In patients with inflammatory arthropathies, such as rheumatoid arthritis, symmetric joint involvement with periarticular osteopenia and marginal erosion is common. In addition, the ankle joint and hindfoot frequently demonstrate a severe valgus deformity.
In the crystalline arthropathies, early involvement of the ankle joint presents as an effusion with softtissue swelling.
Gout is progressive, eventually creating punched-out erosions beneath the joint surfaces.
Pseudogout or calcium pyrophosphate deposition disease eventually leads to chondrocalcinosis within the joint.
Other imaging modalities include MRI, which is used to evaluate soft tissues, tendons, cartilage lesions or talus viability in cases of avascular necrosis, and CT scanning, which provides improved three-dimensional visualization of the bony architecture through the hindfoot.
Technetium bone scans are a high-sensitivity and lowspecificity assessment of changes in bone metabolism and may be helpful when evaluating for occult fractures or acute and subacute chondral injuries. However, the utility of bone scans with respect to degenerative joint disease of the ankle is somewhat limited.
Diagnostic Injections
When doubts persist about the origin of the patient’s pain, diagnostic injections of the ankle joint remain an excellent tool to clarify the clinical situation. A typical injection of approximately 5 mL of 1% or 2% Xylocaine with no epinephrine into the ankle joint is performed through the anterolateral (lateral to peroneus tertius) or anteromedial approach (medial to tibialis anterior). The injection may be done under fluoroscopic control, with or without contrast, to ensure intra-articular positioning that can be helpful with severe joint space collapse. Following the injection, the patient evaluates the level of pain and how long this change lasts.
TREATMENT
Nonoperative Treatment
Many nonsurgical options exist for patients with ankle arthritis. Often, the patient is unaware of these options or has not been willing to try them. However, when presented with the surgical risks and a lengthy postoperative recovery process, the patient may opt for a less aggressive approach. General recommendations for treatment of symptomatic degenerative joint disease is similar for all weight-bearing joints of the body and include anti-inflammatory medications, ambulatory aids, and bracing. Although nonsurgical treatment does not cure the degenerative changes, many patients can experience significant pain relief and may be
able to postpone definitive surgical reconstruction until it is more convenient or their symptoms progress.
able to postpone definitive surgical reconstruction until it is more convenient or their symptoms progress.
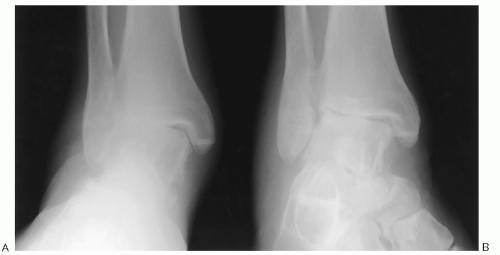 Figure 10.2 Weight-bearing ankle X-ray (A) compared with non—weight-bearing view (B), demonstrating the value of weight-bearing X-rays to better evaluate the status of the joint. |
Symptomatic pain relief can be obtained by using local and systemic medications.
The local injection of intra-articular steroids two to three times per year may provide substantial relief of the symptoms, especially for inflammatory arthropathy.
Systemic medications may include acetaminophen on a regular basis, nonsteroidal anti-inflammatories, or nutritional supplements such as glucosamine and chondroitin sulfate, but narcotics should be avoided.
Activity modifications, use of ambulatory aids such as a cane or walker, and orthotic appliances can also be helpful.
It is important to adapt the treatment to the patient’s needs and lifestyle.
The University of California Biomechanics Laboratory (UCBL) insert is a low-profile orthosis designed for active patients (Fig. 10.3A). It allows correction of flexible malalignment, but does not immobilize the ankle joint, and it may not work well for end-stage disease.
A flexible brace, such as a lace-up brace, decreases motion and provides some support.
A custom-molded rigid ankle—foot orthosis (AFO) controls ankle motion and remains the gold standard for bracing in ankle degenerative joint disease (see Fig. 10.3C).
Each of these orthotic appliances can be combined with a rocker bottom shoe modification to encourage a more normal gait pattern.
Surgical Treatment
When nonsurgical treatment fails to adequately control the patient’s symptoms, surgical intervention may become necessary.
Synovectomy, Loose Body Removal, and Ankle Joint Cheilectomy
The management of early or mild cases of ankle degenerative joint disease is selected according to the underlying etiology.
Chronic inflammatory synovitis, as seen in rheumatoid arthritis or chronic synovitis attributed to recurrent hemarthrosis in hemophilia—which has been symptomatic for greater than 6 months with no satisfactory response to nonsurgical treatment—may be addressed with open or arthroscopic synovectomy. It is important to discuss the goals of the procedure with the patient, which is merely to alleviate the pain. With regrowth of the synovium, the patient usually experiences recurrence of symptoms.
Symptomatic loose bodies in the ankle joint can be excised to control mechanical symptoms and to limit the progression of further cartilaginous lesions. Traumatic lesions with damaging loose bodies, impinging synovial chondromatosis, and displaced intra-articular orthopaedic implants are some other examples that may respond well to excision, either arthroscopic or through open arthrotomy.
Some selected mild and moderate cases of ankle osteoarthrosis with a preserved joint space may benefit from removal of osteophytes (cheilectomy). Osteophytes can be visualized on the anterior distal part of the tibia and the dorsal aspect of the talus (Fig. 10.4), but in one cadaveric study, they were found to rarely be in close contact on forced dorsiflexion. Even so, many patients report symptoms related to anterior impingement with painful limited dorsiflexion of the ankle, which respond well to surgical debridement. In more advanced cases, the patient generally does not feel relief because of the underlying joint disease. When planning incisions, it is important to keep in mind the high likelihood for further surgery in this area, including possible ankle fusion or arthroplasty.
Ankle Arthrodesis
Ankle arthrodesis remains the gold standard for surgical treatment of patients with advanced degenerative joint disease of the ankle that has failed conservative management.
Current surgical techniques designed to obtain bony union continue to rely on basic orthopaedic principles: a large surface area of healthy bleeding cancellous bone apposition combined with compression at the level of the intended fusion site and rigid fixation. In general, patients with rheumatoid arthritis have a higher union rate, possibly because of their relative lack of dense, hypertrophic
cortical bone. Patients with a higher risk for delayed union or nonunion include smokers or those who are noncompliant and patients with spasticity, significant bone defects, poorly vascularized lower limbs, and infected or neuroarthropathic cases. These conditions may have a significant impact when choosing a particular operative technique or the postoperative management.
cortical bone. Patients with a higher risk for delayed union or nonunion include smokers or those who are noncompliant and patients with spasticity, significant bone defects, poorly vascularized lower limbs, and infected or neuroarthropathic cases. These conditions may have a significant impact when choosing a particular operative technique or the postoperative management.
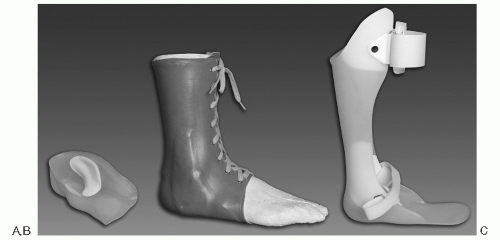 Figure 10.3 Nonsurgical treatment devices: (A) example of the UCBL, (B) the Arizona Brace, and (C) custom-molded rigid AFO. |
Biomechanical Principles.
A successful ankle arthrodesis not only provides predictable results with regard to pain relief, but also requires the adjacent joints and low back to compensate for motion loss by absorbing increased stresses. This may lead to early degenerative changes in those areas and should be discussed with the patient before surgery. Ankle fusion eliminates the motion contribution from that joint, which in turn limits sagittal plantarflexion and dorsiflexion by approximately 70%.
The position in which the tibiotalar joint is fused remains paramount to minimizing postfusion-related problems. Obtaining a solid union in neutral dorsiflexion and approximately 5° of hindfoot valgus is optimal. The arthrodesis should also be positioned at about 10° of external rotation, or symmetric to the contralateral ankle (if uninvolved). Slight posterior translation of the talus relative to the distal tibia may provide some biomechanical advantage to assist the fusion while minimizing the tendency to vault over the foot during gait.
Technical Options.
Over the years, many different techniques have been described for ankle arthrodesis. Although no one technique has proved clearly superior to the others, several principles have emerged to enhance the chances of a successful outcome. When evaluating each case, several factors may influence the choice of technique, including the patient’s biologic makeup (soft tissues, body habitus, expected union rate, quality of bone, etc.), the patient’s psychological makeup, the surgeon’s experience, and possibly the patient’s preference. No single technique is appropriate for every case.
The spectrum of surgical options ranges from arthroscopic joint preparation with limited internal or external fixation devices to open fusion with more substantial internal fixation using only screws or plates and screws (Box 10.2). Each surgical technique possesses its inherent advantages and disadvantages.
The preparation of the fusion interface can be accomplished arthroscopically in cases that do not require significant correction of deformity or position. This procedure is a less invasive approach, minimizing soft-tissue trauma and postoperative pain, but it carries a significant learning curve for the surgeon (Fig. 10.5A). Alternatively, open debridement permits more extensive visualization of the articular surfaces while allowing the surgeon to correct malalignment more easily. The more recent development
of mini-open approaches, which use extended arthroscopic portal incisions, combines some of the advantages of both open and arthroscopic debridements.
of mini-open approaches, which use extended arthroscopic portal incisions, combines some of the advantages of both open and arthroscopic debridements.
BOX 10.2 SURGICAL OPTIONS FOR ISOLATED ANKLE ARTHRODESIS
Articular Surface Debridement
Arthroscopic
Mini-open
Open
Fixation Techniques
External Fixation
Uniplanar (Charnley)
Triangular (Calandruccio)
Circular (Ilizarov)
Internal Fixation
Steinman pins
Cannulated compression screws
Plates and screws
Blade plate
Surgical Technique
Open ankle arthrodesis remains the standard procedure.
In the supine position, draping is performed, taking care to allow complete access to the tibia and the knee.
A thigh tourniquet is routinely used by most surgeons.
Several approaches can be considered, taking into account the quality of soft tissues, previous incisions, and surgeon’s experience.
A single longitudinal midline anterior approach between the extensor hallus longus and the tibialis anterior tendon has been described, but the disadvantages of this approach include poor access to the medial and lateral gutters and possible neurovascular injury.
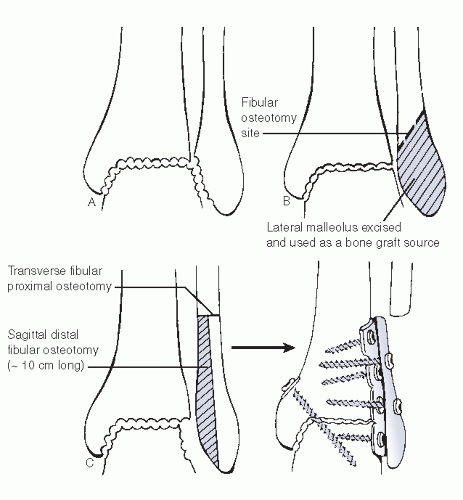
The most common approach uses bilateral longitudinal medial and lateral incisions with a lateral malleolus osteotomy. A skin bridge of at least 7 cm is maintained to protect the vascular supply to the skin. Distal fibular osteotomy allows excellent visualization and constitutes a good autologous source of bone graft (see Fig. 10.5B).
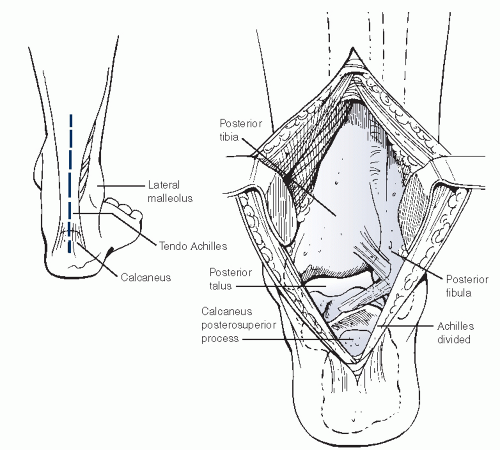
The posterior approach may be considered in cases with significant soft-tissue scarring anteriorly or multiple prior incisions elsewhere. The Achilles tendon is split longitudinally, and the flexor hallus longus muscle belly is progressively detached from the posterior aspect of the fibula and retracted medially, protecting the tibial nerve and posterior tibial vessels (Fig. 10.6).
The joint surfaces are debrided to healthy cancellous bone, preserving as much bone stock as possible. Osteotomes and rongeurs theoretically avoid thermal trauma created by saws and burrs, which may diminish the rate of fusion.
Bone surface apposition should be maximized while preparing the fusion; feathering or shingling the surfaces to ensure that the sclerotic subchondral bone has been adequately debrided can be helpful.
Fixation has evolved over the years, ranging from external to internal fixation, with most surgeons presently using internal fixation. External fixation devices remain an important tool in the surgeon’s armamentarium, especially in cases with infection or occasionally compromised soft tissues. Sir John Charnley developed a uniplanar external fixation device that has evolved into multiplanar external transfixing devices to apply compression more evenly across the ankle fusion site. Ilizarov’s principles using circular wire fixators have also been applied, which progressively add compression across the joint.
Internal fixation can be accomplished with various devices.
When bone quality permits, screws allow the use of lag technique to create compression across the fusion site.
Parallel screws, in theory, generate continued compression along the axis of the screws.
In practice, crossed screws provide even greater purchase with an increased load to failure (Fig. 10.7).
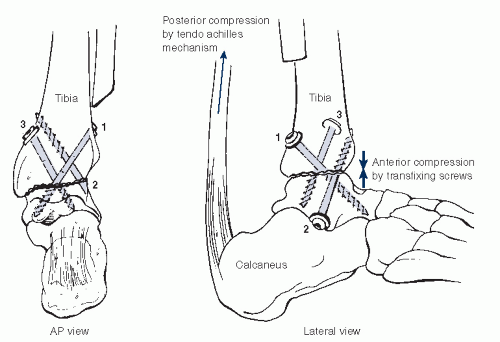
Figure 10.7 Ankle fusion technique utilizing anterior compression screws, with the tendo-Achilles posteriorly theoretically providing compression across the fusion site.
In patients with poor bone quality, such as those on chronic steroid therapy or rheumatoid arthritis, Steinman pins may be the only fixation possible.
Alternatively, an “anterolateral tension-band plate technique” creating compression through a reconstruction plate represents one of the most rigid fixation techniques, especially in cases with preoperative moderate to severe deformity (see Figs. 10.8 and 10.5C).
Finally, blade plates provide yet another option to the surgeon for more rigid fixation and have been used with success, particularly in osteoporotic patients or when large bone defects are present.
Bone Grafting.
Routine use of bone grafting in primary ankle arthrodesis remains common, but may be unnecessary. Some ankle fusions may be complicated by a significant bone defect or by insufficient bone-to-bone apposition and thus require grafting. Attempting to fuse any unhealthy bone end to another is a risk that can be avoided by adequate debridement, taking into consideration the resulting defect. The use of bone graft should not be considered a replacement for proper preparation of bone surfaces. Although the use of graft material to help in those circumstances is a well-established practice, there is paucity of evidence-based literature to rely on when it comes to choosing one type of graft over another. A great deal of interest has prompted an increase in research regarding bone grafts and bone graft substitutes, and their results need to be closely scrutinized for variables and appropriate controls.
Depending on the size of the defect, a structural or morcellized graft can be used.
Large defects can be best filled with a tricortical iliac crest graft to fill the space and maintain the length of the lower limb.
Autologous graft, allograft products, and synthetic substitutes represent a variety of bone graft options, with their respective advantages and disadvantages.
Postoperative Management
Following the procedure, a compressive dressing and splint are applied to control swelling and maintain appropriate alignment.
The use of a popliteal block for postoperative pain relief can significantly reduce the need for narcotics, both during and after surgery.
Most patients are highly satisfied with their postoperative pain control following a popliteal block. The use of narcotics and hospital stay are also decreased with the use of this block, which lasts on average of 12 to 26 hours.
The technique uses a nerve stimulator or ultrasound and can be safely performed after the patient is under general anesthesia with bupivacaine or ropivicaine (Fig. 10.9).
When swelling allows, a non—weight-bearing short leg fiberglass cast is applied to help maintain neutral alignment.
The expected duration to fusion can vary depending on several factors, and the immobilization is adjusted for each case on the basis of on regular clinical and radiologic assessments.
In general, the patient is kept non—weight bearing for 6 weeks and then put in a walking cast for an additional 4 to 6 weeks. A walking cast boot can be used thereafter until satisfactory bony and clinical union is achieved.
In some cases, such as neuroarthropathy, the period of non—weight bearing and total length of cast immobilization may need to be adjusted, sometimes doubling or tripling the usual recovery process.
Results.
Successful ankle arthrodesis occurs in approximately 85% to 90% of cases, but rates have varied widely over the years, from 50% to more than 90%. Long-term follow-up studies, at more than 25 years, reveal the results to be durable and the patients to be satisfied, despite additional degenerative changes seen in the adjacent joints. Some patients may benefit from rocker bottom shoe modifications following ankle fusion, which can improve their gait, particularly if the hindfoot joints have some ankylosis.
Complications.
Nonunion remains the most frequent significant complication associated with ankle arthrodesis. Causes vary widely and include biologic and mechanical factors. The initial treatment for symptomatic nonunion includes bracing, activity modification, and other nonsurgical modalities. However, when these fail to control the symptoms, a revision arthrodesis may be considered. In those cases, it is important to identify risk factors for pseudoarthrosis, such as smoking, poor vascularization, patient noncompliance with weight-bearing restrictions, infection, technical errors, or hardware failure. Despite improved techniques, implants, and graft materials, revision ankle arthrodesis continues to yield a disappointing 20% nonunion rate in nonneurologic conditions. Neuroarthropathic patients have a much higher nonunion rate (50% or more).
Malunion of an ankle arthrodesis constitutes another complication. Malposition during surgery or progressive adjacent joint deformity can lead to clinical symptoms. Mild or moderate varus or valgus deformity may be compensated with shoe modifications or orthotic appliances. Relative plantarflexion creates a vaulting type of gait pattern and leads to symptomatic knee pain resulting from a hyperextension or back knee component during the midstance phase of gait. Excessive external or especially internal rotation is difficult to compensate for and can lead to significant gait disturbances. Major malposition may require correction with an osteotomy.
Persistent pain despite solid fusion can often be attributed to underlying subtalar pathology that might have been present preoperatively or might have developed subsequent to the ankle arthrodesis. Diagnostic injection may help to confirm this. Other long-term complications include biomechanical effects due to increased stress and motion in adjacent joints. Overuse of these joints at a supraphysiologic level can lead to progressive degeneration in these articulations as well.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree