Fig. 1
Limits (dashed lines) of the deep gluteal space beneath the gluteus maximus muscle: lateral, linea aspera; medial, sacrotuberous ligament and falciform fascia; superior, inferior margin of the greater sciatic notch; inferior, the distal border of the ischial tuberosity. PI piriformis muscle, OI obturator internus muscle, HS hamstring muscles
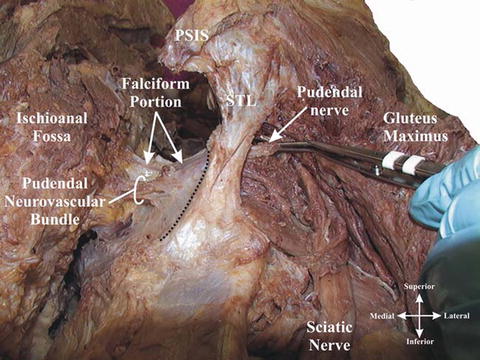
Fig. 2
Sacrotuberous ligament and the falciform process (Reprinted with permission from Loukas et al. [14])
The piriformis muscle occupies a central position in the buttock and is an important reference for identifying the neurovascular structures emerging above and below it (Fig. 3). This muscle arises from the ventrolateral surface of the sacrum, gluteal surface of the ileum, and sacroiliac joint capsule. The distal attachment of the piriformis is at the medial side of the upper border of the greater trochanter, often partially blended with the common tendon of obturator/gemelli complex [15–17]. Distal to the piriformis muscle is the cluster of short external rotators: the gemellus superior, obturator internus, gemellus inferior, and quadratus femoris muscle. At the ischial tuberosity, the long head of biceps femoris and semitendinosus have a common tendinous origin. The semimembranosus muscle also originates from the ischium, laterally and anteriorly to the long head of the biceps/semitendinosus muscles common origin [18] (Fig. 4).



Fig. 3
Schematic illustrating the nerve anatomy of the deep gluteal space (Reprinted from Filler [19])

Fig. 4
Origin of the hamstrings muscles at ischial tuberosity. (a) Posterolateral view of the hamstrings origin at the ischial tuberosity (dashed line) in a cadaver specimen. The semimembranosus muscle origin (Sm) is anterior and lateral to the conjoint origin of the semitendinosus and long head of the biceps femoris muscles (St/Bi). SN sciatic nerve. (b) Posterior view after detachment of the semitendinosus and long head of the biceps femoris muscles from the ischial tuberosity (blue demarked area). The semimembranosus origin (Sm) was preserved. Solid line marking the origin of the sm located lateral to the St/Bi origin at the ischial tuberosity
Seven neural structures exit the pelvis through the greater sciatic notch: posterior femoral cutaneous nerve, superior gluteal nerve, inferior gluteal nerve, nerve to obturator internus, nerve to quadratus femoris muscle, pudendal nerve, and sciatic nerve (Fig. 3). Table 1 is a summary of the usual motor and sensory functions for each nerve. Accompanying the respective nerves are the superior gluteal vessels, inferior gluteal vessels, and internal pudendal vessels.
Table 1
Summary of function of the nerves in the deep gluteal space
Nerve | Motor innervation | Sensory innervation |
|---|---|---|
Posterior femoral cutaneous nerve | Gluteal region, perineum, and posterior thigh and popliteal fossa | |
Superior gluteal nerve | Gluteus medius, gluteus minimus, and tensor fascia lata | |
Inferior gluteal nerve | Gluteus maximus | |
Nerve to obturator internus | Superior gemellus and obturator internus | |
Nerve to quadratus femoris | Inferior gemellus and quadratus femoris | Hip capsule |
Pudendal nerve | Perineal muscles, external urethral sphincter, and external anal sphincter | Perineum, external genitalia |
Sciatic nerve | Semitendinosus, biceps femoris, semimembranosus, extensor portion of the adductor magnus, and leg and foot musculature | Leg and foot, except for the saphenous nerve dermatome |
The anatomic positions of the inferior gluteal artery (IGA) and medial circumflex femoral artery (MCFA) are relevant within the deep gluteal space. The IGA enters the deep gluteal space with the inferior gluteal nerve and supplies the gluteus maximus muscle. This artery also gives a superficial arterial branch that crosses the sciatic nerve laterally between the piriformis and superior gemellus muscles. Another branch of the IGA is the descending branch, which runs along the posterior femoral cutaneous nerve in a frequency of 72 % according to a cadaveric study [21]. The MCFA follows the inferior border of the obturator externus and crosses over its tendon and under the external rotators and piriformis muscle (Fig. 5) [22]. The existence of an anastomosis between the inferior gluteal artery and the medial femoral circumflex artery is frequent [23].


Fig. 5
Deep branch of the medial femoral circumflex artery. Posterior aspect of the right hip, demonstrating the anatomic position of the deep branch of the medial femoral circumflex artery. (1) greater trochanter, (2) trochanteric branch of the medial femoral circumflex artery, (3) quadratus femoris muscle, (4) obturator externus muscle, (5) obturator internus and gemellus muscles, and (6) anastomotic branch to the inferior gluteal artery. Cran cranial, Lat lateral (Reprint with permission from Kahlor et al. [22])
Sciatic Nerve Anatomy and Biomechanics
The sciatic nerve is formed by the L4–S3 ventral rami in the sacral plexus. Nerve fibers of the fibular and tibial components maintain a pattern of fiber separation in these branches and in the sciatic nerve. The sciatic nerve physically splits in tibial and fibular divisions at highly variable locations from the pelvis to the popliteal fossa, although this split is more frequent at the distal thigh [24]. Often, the split is oblique and may not be seen in a uniplanar MRI view [25]. Most sciatic neural fibers are destined to motor and sensory innervation distal to the knee. However, important branches arise from the nerve in the deep gluteal space and thigh. A summary of the sciatic nerve branches in the thigh is depicted in Fig. 6 according to Seidel et al. [26] and Sunderland and Hughes [25].


Fig. 6
Schematic showing the branches of the sciatic nerve before the physical separation in tibial and fibular nerves. The mean distance from the ischial tuberosity (IT) to the branch emergence is described between brackets. GSN greater sciatic notch, IT ischial tuberosity. Sunderland and Hughes [24] served as reference for the location of the BSH branch and Seidel et al. [26] for the other branches
Neural tissue and nonneural tissue compose the sciatic nerve. The ratio neural/nonneural tissue changes from 2/1 at the level of piriformis muscle to 1/1 at the midfemur, i.e., there is an increase in the nonneural tissue contribution as the sciatic nerve courses distally [27] (Fig. 7). The composition of the sciatic nerve also varies during the aging process, with increase in connective tissue and decrease of myelinated nerve fibers [28].


Fig. 7
Nonneural and neural tissue composition of the sciatic nerve at different locations. (a) Schematic diagram showing four locations of analysis: midgluteal, subgluteal, midfemoral, and popliteal sciatic nerve. (b) Transversal view of the sciatic nerve at the four locations, with details of the demarcated neural contents (right; black dots) and epineural areas (gray fields). (c) Relative values (percentages) of neural versus nonneural tissue inside the epineurium (means SDs) (Reprint with permission from: Moayeri and Groen [27])
The nerve fibers of the sciatic nerve do not course between the tibial and fibular divisions [17]. However, fibers are often changing from one fascicle to another within each division [25]. Sunderland reported 6 mm as the maximum length of nerve trunk with a constant fascicular pattern, although an individual fascicle can maintain the same neural fibers for greater distances [25]. In general, most fascicles contain fibers for the majority, if not all, of the peripheral branches. Nevertheless, there is a tendency of grouping fibers for different muscles with similar function, for example, the fibers for the hamstring muscles are located anterior-medially in the proximal portion of the sciatic nerve. A progressive arrangement is found until the appearance of fascicles with nervous fibers exclusively destined to specific branches [25].
The sciatic nerve has a segmental arterial supply by branches of the IGA, MCFA, and perforating arteries of the thigh (usually the first and second) [29–31] (Fig. 8). The venous drainage of the sciatic nerve is performed through the perforators to the femoral profunda system in the thigh and to the popliteal vein at the knee [32] (Fig. 9). Nonfunctioning sciatic veins have been related to sciatic nerve symptoms [9].



Fig. 8
Nutrient arteries of the fetal sciatic nerve in the gluteal and posterior femoral region; left fetal lower extremity. MGM Gluteus medius muscle, PM piriform muscle, IGA inferior gluteal artery, AASN accompanying artery of sciatic nerve, SN sciatic nerve, CPN common peroneal nerve, TN tibial nerve. a = Branch of medial circumflex femoral artery, b = first perforating artery, c = second perforating artery, d = third perforating artery (Reprint with permission from Ugrenovic et al. [31])

Fig. 9
Schematic diagram of the venous drainage of the sciatic nerves. Arrows designate the level of the knee. From proximal to distal the dominant venous drainage of the sciatic nerve is via the perforators of the profunda system in the thigh and directly to the popliteal vein at the knee. In the leg, the tibial and peroneal nerves drain predominantly to the plexus around their accompanying arteries as well as to muscular veins (Reprint with permission from Del Pinãl and Taylor [32])
The sacral plexus is anatomically close to the internal iliac vessels, their branches, and tributaries. The superior gluteal vessels run either between the lumbosacral trunk (L4–L5 ventral rami) and first sacral ventral ramus or between the first and second sacral rami, whereas the inferior gluteal vessels lie between either the first and second or second and third sacral rami (Fig. 10) [17, 33]. The ovaries are close to the sacral plexus, although on the left side the sigmoid is usually between the ovary and sacral plexus. The intimate anatomic relation between the iliac vessels, ovaries, and sacral plexus is an important consideration in sciatica caused by sacral plexus vascular compression and endometriosis [34].


Fig. 10
Superior and inferior gluteal arteries crossing the sacral plexus before accessing the deep gluteal space
The sciatic nerve is the terminal branch of the sacral plexus and courses anterior to the piriformis muscle in the pelvis. Variation in the relationship between the sciatic nerve and the piriformis muscle is present in 16–17 % of the subjects and can be a cause of sciatic nerve entrapment [35, 36]. After leaving the piriformis muscle, the sciatic nerve runs posteriorly to the obturator/gemelli complex and quadratus femoris muscle, located at an average of 1.2 ± 0.2 cm from the most lateral aspect of the ischial tuberosity and maintaining an intimate relationship with the hamstring origin [18] (Fig. 4). The sciatic nerve then enters the thigh posteriorly to the adductor magnus muscle and crosses anteriorly the long head of the biceps femoris. Next, the nerve runs between the semimembranosus and biceps before accessing the popliteal fossa.
Under normal conditions, the sciatic nerve is able to stretch and glide in order to accommodate moderate strain or compression associated with joint movement. During a straight leg raise with knee extension, the sciatic nerve experiences a proximal excursion of 28.0 mm [37] at 70–80° of hip flexion. Strain of the sciatic nerve increases 6.6 % relative to the extended hip [37]. Fleming et al. measured the sciatic nerve strain throughout ten hip arthroplasty procedures [38]. The strain increased on average 26 % during hip flexion with the knee in extension. This amount of strain is significant and may cause nerve dysfunction. An animal study reported the nerve conduction was completely blocked after stretching of 12 % of the nerve length for 1 h [39]. At 6 % strain, the authors found a decrease of 70 % in amplitude of the action potential after 1 h [39]. The changes in femoral bone morphology may influence sciatic nerve kinematics during hip mobilization [2]. Therefore, it is always important to assess osseous parameters, including femoral and acetabular version (Figs. 11 and 12). Hip flexion, adduction, and internal rotation increases the distance between the greater trochanter and posterior superior iliac spine and the distance between the greater trochanter and ischial tuberosity. This hip position stretches the piriformis muscle and causes a narrowing of the space between the inferior border of the piriformis, the superior gemellus, and the sacrotuberous ligament [40].



Fig. 11
Superior view of the sciatic nerve (SN) excursion between the greater trochanter (GT) and ischial tuberosity (IT) in a cadaveric specimen, right hip. The sciatic nerve runs in a tunnel formed by the greater trochanter and ischial tuberosity when the hip is flexed with the knee extended. This pattern of excursion of the sciatic nerve may change according to the bone morphology, adjacent soft tissue restriction, and knee position (flexion or extension)

Fig. 12
Posterior view of the sciatic nerve (SN) excursion between the greater trochanter (GT) and ischial tuberosity (IT) in a cadaveric specimen, right hip. The sciatic nerve is forced posterior to the GT and ischium during increasing hip flexion and external rotation (images from left to right). The knee was flexed and the last figure represents a seated position. This pattern of excursion of the sciatic nerve may change according to the bone morphology, adjacent soft tissue restriction, and knee position (flexion or extension)
Etiology
The piriformis muscle and tendon are the most common source of extrapelvic sciatic nerve impingement. Yeoman first described the possibility of sciatic nerve entrapment by the piriformis muscle in 1928 [41]. The introduction of the term “piriformis syndrome” has been credited to Robinson, in 1947 [42]. The diagnostic resources have improved over the past decades, and a number of structures have been associated with sciatic nerve entrapment within the deep gluteal space: the piriformis muscle [2, 3, 11, 12, 43–49], fibrous bands containing blood vessels [2, 3, 43] (Fig. 13), gluteal muscles [1], gemelli-obturator internus complex [6, 7], hamstring muscles [4, 5], ischial tuberosity [8, 50], and space-occupying lesions [11, 12]. Additionally, vascular abnormalities [10, 47], prolonged surgery in the seated position [51], acetabular reconstruction surgery [52], and total hip replacement [53] have been reported to cause compression of the sciatic nerve. Considering the variation of anatomical structures causing the entrapment, the term “deep gluteal syndrome” [1] seems to be a more accurate description of this nondiscogenic sciatica.


Fig. 13
Entrapment of the sciatic nerve by fibrovascular scar band, endoscopic visualization. (a) The sciatic nerve is indicated by the open arrows and is anterior to a fibrovascular band (fvb) and another fibrous band (fb). (b) Same view demonstrating the blood flow through a vessel in the fibrovascular band (black arrow)
The piriformis muscle is the most common source of sciatic nerve entrapment [2, 3, 11, 12, 43–49]. The risk of nerve compressive symptoms is increased by the existence of variation in the relationship between the piriformis muscle and the sciatic nerve. Six categories of piriformis-sciatic nerve variations have been identified [35] (Fig. 14). The prevalence of anomalies was 16.9 % in a meta-analysis of cadaveric studies [36] and 16.2 % in a review of published surgical case series [36] (Table 2). It is important to mention that the anomaly itself may not be the etiology of the Deep Gluteal Syndrome symptoms. Martin et al. [2] reported on 35 patients endoscopically treated for deep gluteal syndrome. Eighteen patients involved the piriformis muscle as etiology, including the sciatic nerve passing through the piriformis muscle or a portion of piriformis muscle/tendon passing through or anterior to the sciatic nerve [2]. A thick piriformis tendon hidden under the piriformis belly has been indentified as a cause of sciatic nerve compression (Fig. 15). Hypertrophy of the piriformis muscle has also been associated with sciatic nerve compression [12, 46, 47, 54]. However, of 14 patients with posttraumatic piriformis syndrome, Benson and Schutzer found that only two had larger piriformis muscles on the symptomatic side and seven appeared smaller than the unaffected side [44].



Fig. 14
Schematic of piriformis/sciatic nerve variants. Six types of arrangement of the sciatic nerve, or of its subdivisions in relation to the piriformis muscle, arranged in the order of frequency [35]. Gluteal (external) view. The percentage incidence in 240 examples is indicated. Figures e and f were hypothetical in 1938 [35]. (a) Nerve undivided passes out of greater sciatic foramen, below piriformis muscle, (b) divisions of nerve pass through and below heads of muscle, (c) divisions above and below undivided muscle, (d) nerve undivided between the heads of muscle, (e) divisions of nerve between and above heads, and (f) undivided nerve above undivided muscle (Figure reprinted from Beaton and Anson [35])
Table 2
Characteristics of cadaveric studies: piriformis and sciatic nerve variants
Investigator | Number of cadavers (number of sides included) | Percentage of female cadavers | Laterality of the anomalies | Notes | ||
|---|---|---|---|---|---|---|
Unilateral | Bilateral (%)a | |||||
Parsons and Keith [91] | 69 | (138) | “Mostly men” | – | – | |
Bardeen [92] | 123 | (246)b | 30 | – | – | |
Trotter [93] | 232 | (464) | 21 | 24 | 48 (63.6) | |
Beaton and Anson 1937d | 60b | (120) | – | 5 | 14 (73.6) | |
Beaton and Anson [35]c | 60 | (120) | – | 3 | 2 (40.0) | Results presented in this study included data from a previous study |
Ming-Tzu [95] | 70 | (140) | “Mostly men” | 22 | 24 (52.2) | |
Misra [96] | 150 | (300) | – | – | – | |
Anson and McVay [97]c | 1,004b | (2,000) | – | – | – | This data set incorporated data from Beaton and Anson’s two previous studies |
Nizankowski et al. [98] | 100 | (200) | 45 | – | – | |
Lee and Tsai [99] | 84 | (168) | 13 | – | – | |
Pecina [100] | 65 | (130) | – | – | – | |
Chiba [101] | 257 | (511) | 46 | – | – | Three lower limbs of males excluded |
Chiba et al. [102] | 221 | (442) | – | – | – | |
Pokorny et al. [103] | 51 | (102) | – | – | – | |
Fishman et al. [104] | 38 | (76) | – | 1 | 10 (91.0) | This data was found in a study presenting data on the usage of H-reflex latencies for diagnosing piriformis syndrome |
Benzon et al. [71] | 36 | (66) | – | 1 | 0 | In six cadavers, only one side was studied |
Agur and Dalley [105] | 320b | (640) | – | – | – | |
Ugrenovic et al. [106] | 100 | (200) | – | – | – | This study was carried out on human fetuses |
Pokorny et al. [107] | 91 | (182)b | – | – | – | |
Guvencer et al. [108] | 25 | (50) | 0 | – | – | |
Total | See Table 3 | 56 | 98 (63.6)e | |||

Fig. 15
Ancillary musculotendinous branch through the sciatic nerve
Atypical fibrovascular scar bands and hypertrophy of the greater trochanteric bursae have been reported in many cases of sciatic nerve entrapment [2, 3] (Fig. 13). In 27 of the 35 patients previously described by Martin et al. the greater trochanteric bursa was found to be excessively thickened, and large fibrovascular scar bands were present in many patients [2]. The fibrovascular bands extended from the posterior border of the greater trochanter to the gluteus maximus on to the sciatic nerve and then proximally to the greater sciatic notch [2]. The obturator internus/gemelli complex is commonly overlooked in association with sciatica-like pain [6, 7, 15]. As the sciatic nerve passes under the belly of the piriformis and over the superior gemelli/obturator internus, a scissor effect between the two muscles can be the source of entrapment. In one case, Martin et al. found the obturator internus penetrating the sciatic nerve.
The sciatic nerve courses close to the hamstrings origin at the most lateral aspect of the ischial tuberosity (Fig. 4). Avulsions of the hamstring tendons or congenital fibrotic bands can affect the sciatic nerve causing symptoms of entrapment [4, 5, 55–57]. Other sources of sciatic nerve entrapment within the deep gluteal space include malunion of the ischium or healed avulsions, greater trochanter ischium impingement (Fig. 16), tumor, sciatic nerve venous varicosities [9] (Fig. 17), and gluteus maximus (from a prior iliotibial band release). Intra-articular hip disorders may also be involved with sciatic nerve symptoms. Patients submitted to surgical treatment of femoroacetabular impingement often recover hip mobility or can move the hip without having intra-articular pain. Considering that neural structures are sensitive to strain [39], increased mobility can lead to strains greater than normal in the sciatic nerve, triggering the sciatic nerve entrapment symptoms in patients with variations in the piriformis-sciatic nerve relationship. This factor may be even more important in patients with capsular laxity and abnormal bone morphologies, such as increased femoral version, retroversion, or greater trochanteric dysmorphism.



Fig. 16
Endoscopic view of sciatic nerve (SN) compression between the greater trochanter (GT) and ischial tuberosity. With hip flexion and external rotation, the sciatic nerve was not able to move due to the ischial outgrowth of bone

Fig. 17
Varicose veins within the sciatic nerve. (a) Schematic drawing of varicose veins within the perineurium and the sciatic nerve. (b) Sciatic nerve at midthigh with varicose veins within the nerve (arrow) in a patient who presented with pain and swelling. A larger refluxing vein is seen as an adhesion with the nerve (Reprinted with permission from Labropoulos et al. [9])
The fibers of the sciatic nerve can be also entrapped in the lumbar spine, pelvis, extrapelvic, and thigh. A discussion regarding intrapelvic etiologies of sciatic nerve entrapment will be provided in the differential diagnoses section. The table 3 summarizes the etiologies of sciatic nerve entrapment reported within the literature.
Table 3




Entrapments of the sciatic nerve within the deep gluteal space in key publications
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








