CHAPTER 29 Wrist Arthritis
Arthroscopic Synovectomy, Abrasion Chondroplasty, and Radial Styloidectomy of the Wrist
The wrist, with its many articular surfaces, is a crucial anatomic link between the hand and forearm. When afflicted by arthritis and conditions limiting the range of motion, the wrist greatly affects the daily lives of patients. The advent of arthroscopy has revolutionized the practice of orthopedic and hand surgeons. Newer techniques and significant application of wrist and small joint arthroscopy can be attributed to many pioneers.1,2
Wrist arthroscopy has provided a tool with which to examine and treat intra-articular abnormalities. Early results for arthroscopic synovectomy of the wrist showed that it reduced pain and swelling and improved joint function.3–6 The transitory or permanent effects depend mainly on the activities of the patient and underlying cause of arthritis. Abrasion chondroplasty of the wrist has not been described at length, but it is known that “repair cartilage” (i.e., fibrocartilage) replaces articular cartilage, as demonstrated in several canine models.7 Abrasion chondroplasty appears to have a therapeutic role in patients with proximal pole hamate arthrosis or radiocarpal arthrosis. Preliminary results of this procedure have been excellent.8–10 This chapter surveys the indications and techniques for arthroscopic synovectomy, abrasion chondroplasty, and radial styloidectomy.
ANATOMY AND PHYSIOLOGY
Matrix metalloproteinases and proinflammatory cytokines (e.g., interleukin-1) are important mediators of cartilage destruction in patients with primary osteoarthritis. Interleukin-1 increases the synthesis of matrix metalloproteinases and thereby plays an important role in osteoarthritis.
Scaphoid fractures can result in osteoarthritis by three mechanisms:
PATIENT EVALUATION
Diagnostic Imaging
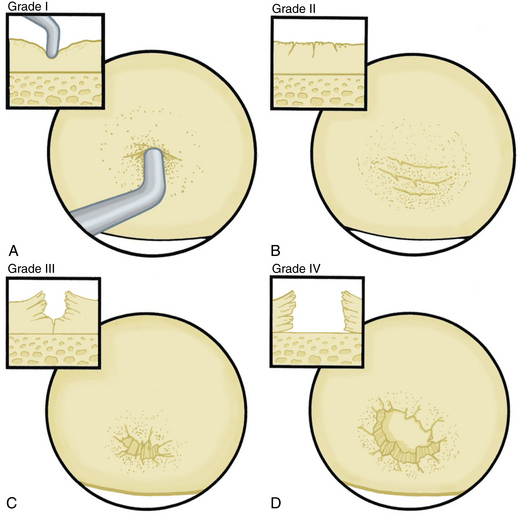
The radiographic evaluation system we use for wrist arthritis is the Outerbridge classification of cartilage defects (Fig. 29-1). We have found that with an appropriate clinical history, dedicated articular cartilage imaging has a sensitivity and specificity reaching the 95% confidence interval. This tool has been confirmed by arthroscopic findings and clinical correlations. However, Haims and colleagues think that magnetic resonance imaging (MRI) of the wrist (41 indirect MR arthrograms and 45 unenhanced [nonarthrographic] MR images) was not adequately sensitive or accurate for diagnosing cartilage defects in the distal radius, scaphoid, lunate, or triquetrum, as demonstrated by correlating MRI with arthroscopic findings.11 In cases of synovitis and ulnar-sided pathology, MRI results are a strong indicator of which areas need to be addressed with the arthroscope. Cartilage defects are often confirmed after diagnostic arthroscopy is completed.
Arthroscopic abrasion arthroplasty, subchondral drilling, and microfracture can be performed for focal chondral defects in patients with moderate degenerative wrist arthritis or when plain radiographs indicate vascular necrosis. MRI is a sensitive method for excluding the diagnosis of avascular necrosis and for evaluating the extent to which fibrocartilaginous repair tissue has formed postoperatively. These methods have been demonstrated for knee pathology, and we have established the same protocols for wrist defects.11.12
TREATMENT
Indications and Contraindications
Arthroscopic synovectomy provides effective treatment of patients with rheumatoid arthritis, juvenile rheumatoid arthritis, systemic lupus erythematosus, and postinfectious arthritis.3–5 Patients with post-traumatic joint contractures and septic arthritis of the wrist after failed systemic antibiotics and lavage also benefit from arthroscopic synovectomy. For rheumatoid patients, we follow the protocol established by Adolfsson.5
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree