Wound Care for Vulnerable Feet
Edward Mahoney and Carolyn B. Kelly
Learning objectives
At the conclusion of this chapter the reader will be able to do the following:
1. Explain the relationship between diabetes and foot ulceration.
2. Identify the interactive factors that contribute to ulceration in the high-risk foot.
3. Describe the components of an effective high-risk foot examination.
4. Explain the importance of each component of a thorough wound examination.
6. Determine which wounds would benefit from the addition of therapeutic modalities.
7. Develop a comprehensive treatment plan to manage vulnerable feet, including those with open wounds.
The thought of losing a limb has to be one of the most frightening things a person will ever face. For the majority of the population, the idea likely conjures up some sort of catastrophic event that can be pushed to the back of the mind as something that is unlikely to occur. Unfortunately, individuals with a high-risk foot face the very real possibility of losing a limb in the foreseeable future. A high-risk foot is one that has an underlying disease process that puts the tissues at a greater risk of breakdown. The largest group of people with high-risk feet in the United States is the diabetic population. In 2006, approximately 65,700 amputations were performed on patients with diabetes, which accounted for more than 60% of all nontraumatic amputations performed that year.1 In the simplest designation, amputations can be divided into traumatic and nontraumatic causes. Trauma can result in extensive tissue damage and is often complicated by infection and foreign materials in the wound bed, but healing generally proceeds appropriately when these factors are corrected. Nontraumatic causes of amputations are not as straightforward. Unlike traumatic wounds, there may not be an isolated incident that can be identified as a causative factor in nontraumatic wounds. In many cases, the wound is the result of an underlying disease, such as diabetes, or condition that will negatively affect wound healing. In these individuals, the key to effective treatment is often early intervention. This chapter is designed to assist the reader in identifying feet at risk of ulceration and implementing comprehensive examination and treatment strategies to prevent or minimize the need for amputation.
Normal wound healing
To fully appreciate the impact of different disease states on wound healing, it is necessary to begin with an understanding of normal wound healing. Wound healing involves a coordinated interaction of three phases: inflammation, proliferation, and remodeling. Although these stages do overlap to some degree, they are discussed individually for purposes of clarity. The body’s first response to injury during the inflammatory phase is to stop the bleeding at the site of injury through a process known as hemostasis. In response to an injury, platelets, which are formed in bone marrow and are free floating in the vascular system, are attracted to the injury site. The platelets also undergo activation, which causes them to change from a round shape into a sticky form that enables them to adhere to the injured area.2 The platelet plug may be enough to stop the bleeding in minor injuries, or it may be augmented by the coagulation cascade to form a larger clot. An in-depth discussion on the coagulation cascade is beyond the scope of this chapter. In terms of wound healing, coagulation is only one part of the role of the platelet. The second role, which is critical to wound healing, is the secretion of numerous growth factors and cytokines that set the stage for later phases of wound healing.
The first cells to arrive at the wound site in response to the coagulation cascade are granulocytes, which are a form of white blood cells. Neutrophils are the most abundant of the granulocytes and are found in the wound within 24 hours after injury. These cells are nonspecific and phagocytic, which is crucial for disposing of damaged cells in the area. Other granulocytes include phagocytic eosinophils and basophils, which release histamine. The next leukocytic cells to respond are monocytes, which become macrophages in the wounded area. Macrophages are phagocytic, but can also be thought of as growth factor factories because they play such a critical role in producing the growth factors that guide the remainder of the healing process.
Toward the latter stages of the inflammatory response, the wound is well into the proliferative phase of healing. The goal of this phase is to resurface the wound with a layer of viable epithelium. For this to occur, a well-vascularized dermal matrix is laid down in the wound bed. To accomplish this, new blood vessels are formed (neovascularization), and collagen is created by fibroblasts (fibroplasia). At the same time, new skin is being produced through the process of reepithelialization, and wound contraction is occurring, which helps to approximate the wound margins and make the resultant scar smaller. The duration of this phase is greatly influenced by the size of the wound, but is generally considered to last up to several weeks. Despite wound closure, the healing process is not yet complete as tissues continue to remodel. In fact, the remodeling phase is by far the longest and can last for more than a year from wound closure until the tissues have reached their maximum strength. Even after the wound has completely remodeled, it will not regain the same strength that uninjured tissue has, and will continue to require close monitoring and protection to prevent reulceration.
Assessment of the high-risk foot
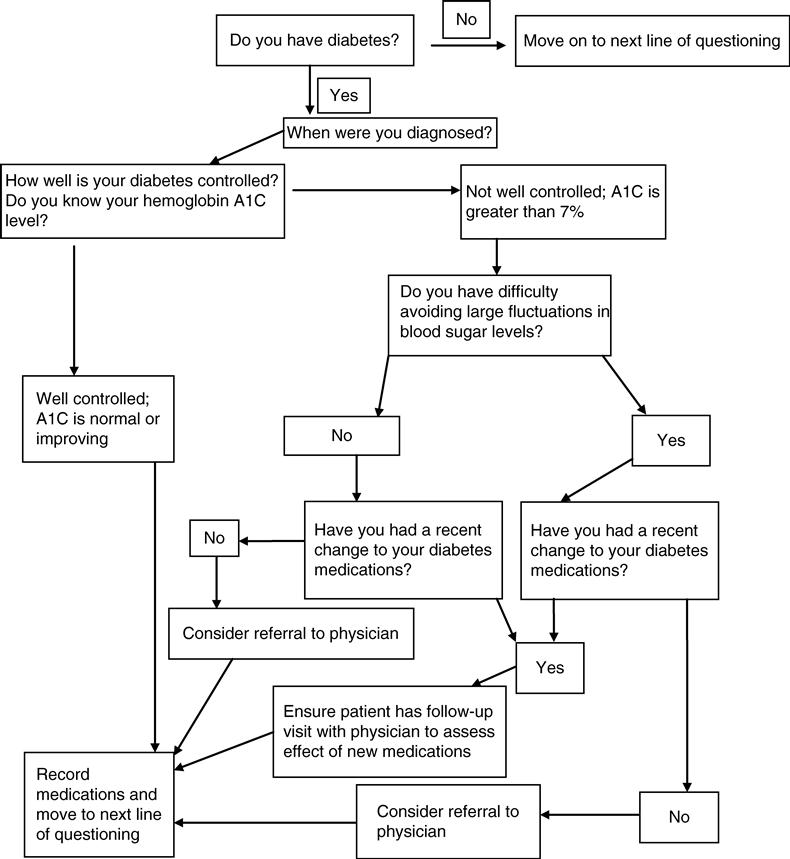
According to the most recent data from the Centers for Disease Control, approximately 60% of all nontraumatic lower-extremity amputations were the result of diabetes in 2006.3 With that in mind, it is of particular importance to assess the patient’s diabetes status (Figure 18-1).
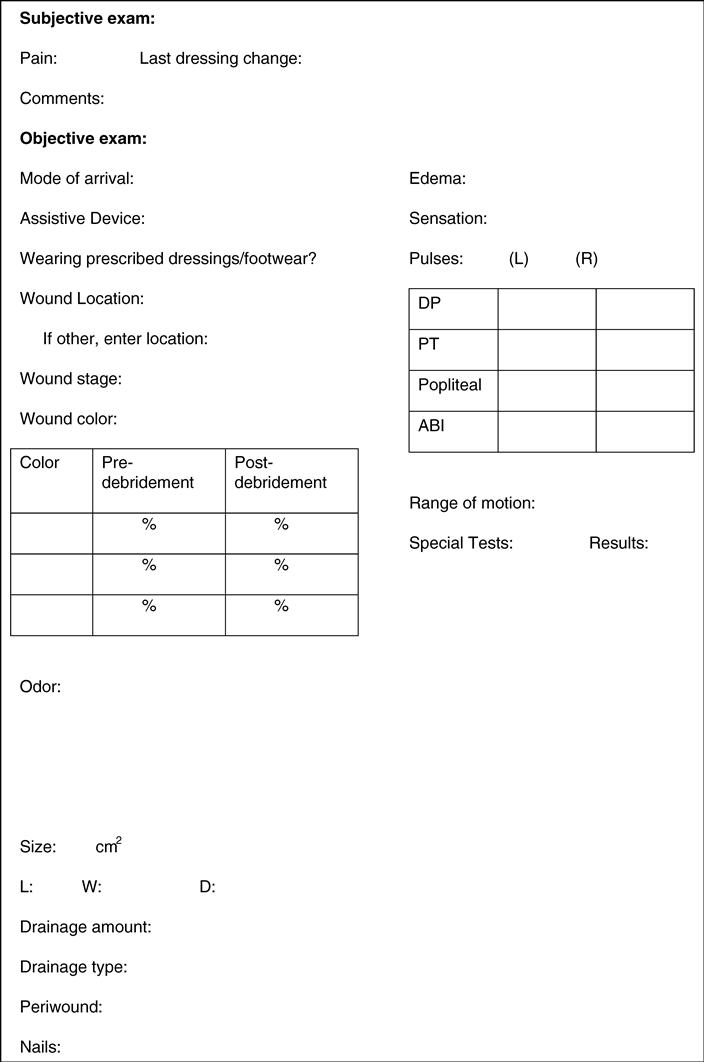
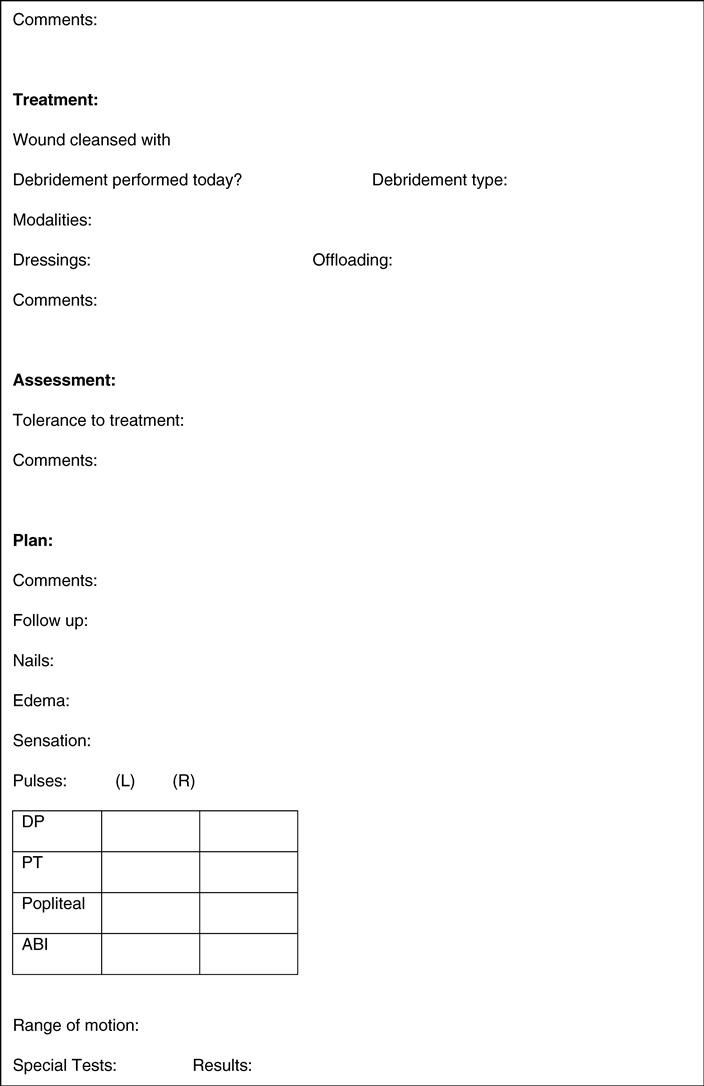
Following a thorough review of systems, a quick, but thorough objective examination of the foot should occur. This examination should include assessments of the vascular, sensory, motor, and autonomic systems, as well as a mobility assessment and footwear inspection.
Vascular Assessment
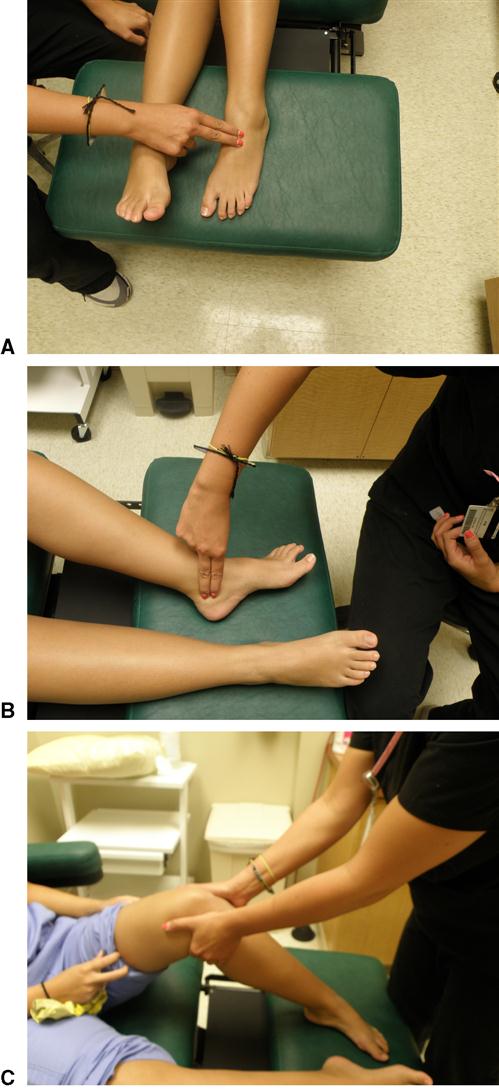
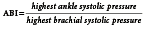
It could be argued that a thorough vascular assessment is the most crucial aspect of the evaluation of a high-risk foot. Not only can impaired blood flow be a causative agent for the development of ulceration, it will impact healing of ulcers regardless of the etiology. A clinical vascular examination can be performed quickly, and help the clinician decide if circulation is adequate or if further, more advanced testing is required. The examination should begin with an assessment of the pedal pulses (dorsalis pedis and posterior tibial). Pulses can be recorded as present or absent, or can be graded on a more qualitative basis (Figure 18-2):
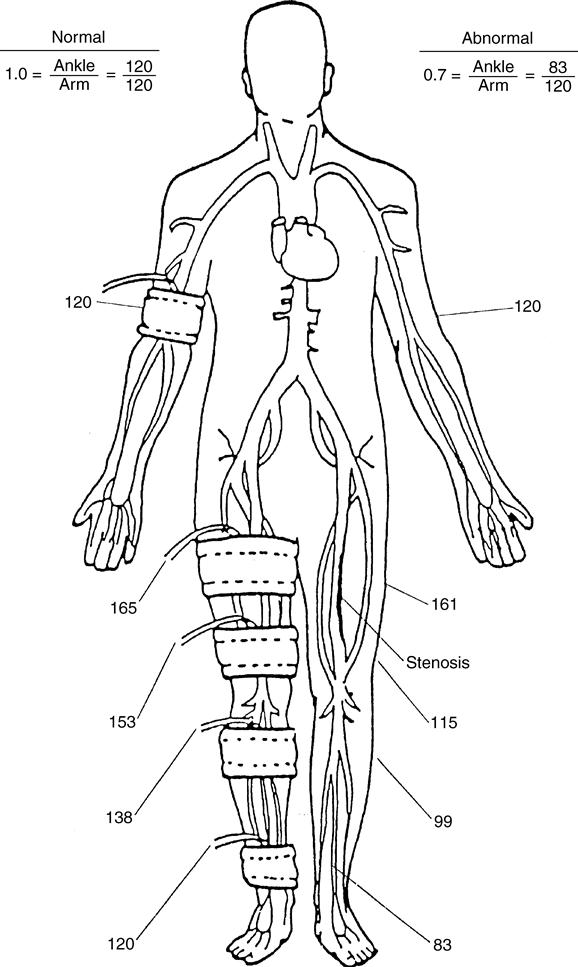
The assessment of pulses should not be used alone to determine the extent of arterial compromise, but should be correlated with other findings from the clinical examination. The lack of a palpable pulse (grade 0) is not sensitive for the detection of peripheral arterial disease. In a study by Collins and colleagues, more than two-thirds of limbs with diagnosed peripheral arterial disease still had palpable pulses.4 Pulse palpation may be most useful for the comparison between the left and right limb to detect abnormalities. If there is any question as to the arterial status of a limb, an ankle-brachial index (ABI) should be performed. The ABI is a comparison of the systolic blood pressure of the pedal arteries with the brachial artery. The systolic pressure is recorded in both arms, unless contraindicated (lymphedema, dialysis port), and the higher of the two values should be used. In the foot, the dorsalis pedis and posterior tibial artery are both assessed and the highest value is used (Figure 18-3).
A normal ABI is 1.0, which indicates normal arterial blood flow to the foot. If an ABI value of less than 0.8 is obtained, referral to a vascular specialist is warranted for further testing. In the case of individuals with longstanding diabetes, an ABI greater than 1.2 may be obtained because of calcified vessels in the lower extremity. If this is the case, the ABI value is of no significance as it pertains to arterial flow and further testing is required. One test that can be performed is a toe pressure. By using a specially designed cuff that fits over the digit and a Doppler flowmeter, the pressure in the digital arteries, which are less affected by calcification, can be assessed (Figure 18-4). A systolic toe pressure greater than 50 mm Hg is generally considered normal; an increased risk of amputation and failure to heal is associated with pressures less than 30 mm Hg.5
Another noninvasive vascular assessment technique is transcutaneous oxygen pressure (TcPO2). Low TcPO2 measurement, a measurement of skin perfusion, is a predictor of ulceration4 and healing.6 In 1999, the American Diabetes Association’s Consensus Development Conference on Diabetic Foot Wound Care recommended use of abnormal toe systolic pressures and TcPO2 measurements to predict poor outcomes.7 Generally, no single noninvasive test provides enough information to make decisions about vascular intervention. Analysis is usually done by a vascular specialist who interprets the results of a combination of tests.
If signs of arterial insufficiency are present and the patient has a foot wound, or if the patient has none of the typical symptoms of ischemia but has a nonhealing wound despite adequate control of infection and external pressure, referral for further vascular evaluation is warranted. Many patients have significant arterial disease but few clinical signs, such as pain or open wounds, that warrant the risks involved with an invasive vascular procedure. They should still be educated in foot care and proper shoe fit. Because better circulation may be necessary to heal an open wound than to keep unbroken skin intact, the goal for patients with arterial insufficiency is to prevent foot wounds from occurring.
Sensory Assessment
Patients in all settings, with many different diagnoses, may have impaired sensation. Diabetes is the most common reason for impaired sensation, but it is also associated with chronic alcoholism, syphilis, Hansen’s disease (formerly leprosy), spinal cord injury, and peripheral nerve injuries. Regardless of the cause, when the ability to perceive an external stimulus is diminished, it increases the risk for ulceration. In patients with diabetes, a loss of protective sensation is the leading cause of foot ulceration.8 Simply put, if a patient cannot feel discomfort, there is no stimulus to change anything. In the case of a foot rubbing on a shoe or brace, an individual with intact sensation will stop to adjust the problem because of discomfort, whereas the person with impaired sensation may be unaware of the problem until the shoes are removed and blood is seen on the sock.
Protective sensation can be assessed in several different ways in the clinic, with very little special equipment needed. The two simplest methods are Semmes-Weinstein monofilaments, and tuning forks. A 5.07 monofilament, which takes 10 g of perpendicular force to bend, is the most widely used clinical tool for the assessment of protective sensation (Figure 18-5).

The patient is instructed to close his or her eyes and the monofilament is applied perpendicular to the skin surface with enough pressure to cause it to bend. Inability to sense the monofilament is considered to be a positive test for the loss of protective sensation. Care must be taken to avoid areas with thick callus, as the test results will not be valid. Alternatively, a tuning fork can be used for vibratory testing. A study by Oyer and associates found a vibrating 128-Hz tuning fork placed on the toe was more sensitive to the onset of neuropathic changes than monofilament testing.9 In this testing procedure, a clanging tuning fork is placed on the area to be tested and remains there until the subject can no longer feel the vibration. The tuning fork is then quickly moved to an area of known intact sensation on either the subject or examiner. If the vibration can still be felt in that site, the test is positive for a loss of vibratory sensation. Other authors have found similar results using similar methods with tuning forks of different frequencies, for example, 512 Hz, which may be more convenient as the 512 Hz tuning fork is smaller (Figure 18-6).10

Motor Assessment
A thorough musculoskeletal evaluation is necessary to determine a given patient’s likelihood for ulceration. Deformities and abnormal biomechanics often change pressure distribution in the foot and can lead to discomfort, callus, and, ultimately, ulceration. The clinician can begin to assess for motor impairments while the patient is seated. The wear pattern on shoes, as well as the presence of calluses on the foot, can identify potential pathologies that ultimately may lead to ulcer formation. Following a visual inspection of the feet and footwear, a musculoskeletal examination that includes reflexes, strength, and range of motion should be performed. Particular attention should be paid to toe extension and dorsiflexion range of motion, as limitations in either one greatly increases weight-bearing forces through the forefoot in the latter stance phases of gait. This becomes increasingly important to assess if the patient has diabetes, as a loss of dorsiflexion has been widely documented in that population.11,12 If a patient is ambulatory, a gait assessment should be a standard part of the high-risk foot assessment. Major deviations from the normal gait pattern can be assessed with a quick visual inspection. For example, patients with peroneal nerve injuries have difficulty with foot clearance and have a shorter loading response, which increases pressure at the forefoot. Alternatively, a patient could have increased forefoot pressure in terminal stance as a result of limited dorsiflexion range of motion. A mild limitation in motion may present as an early heel rise, while a more severe restriction can lead to excessive knee flexion for clearance during the swing phase of gait. With a static foot assessment, it may be apparent that both individuals have increased forefoot pressure, but the cause would not be known, with the result that the optimal intervention could not be selected. With careful gait analysis, the clinician can determine the cause of the pressure and choose appropriate interventions, such as a rocker bottom shoe to substitute for the midfoot rocker in the first case or an orthosis to aid in dorsiflexion in the second case. Chapter 5 provides an in-depth review of the gait assessment.
Many of the deformities that occur as a result of motor neuropathy are more subtle than the examples above. As neuropathy advances, the intrinsic muscles atrophy and become weaker, leading to muscle imbalances and changes in joint alignment.13,14 When tissues over these joints are then loaded, they are unable to withstand the same amount of pressure and begin to break down. As extensor muscles on the dorsum of the foot overpower flexor muscles of the plantar aspect, the net result is extension at the metatarsophalangeal joint, which increases pressure at the plantar aspect of the metatarsal head (MTH). This occurs with both claw, and hammer toe deformities; the difference being that claw toes are characterized by flexion of both interphalangeal (IP) joints, whereas hammer toes have flexion at the proximal IP and extension at the distal IP joint. Care must also be taken to protect the distal tips of the toes as well as the dorsum of the IP joints, as these areas are easily injured from rubbing on shoes. Persons with diabetes who have motor neuropathy may develop a high-risk foot, commonly referred to as an “intrinsic minus” foot because of the impairment in function of the small muscles of the foot. The intrinsic minus foot presents as a pes cavus (high arch) deformity with prominent MTHs. Compounding matters is the distal migration of the metatarsal fat pad into the toe sulcus as a result of muscle imbalance. Now the metatarsal region has increased pressure because of the foot shape, as well as the loss of fat pad over the MTH that would normally increase the total surface area being loaded.15
Partial foot amputation is another deformity that alters plantar pressure distribution. Because the surface area to carry the force of body weight is smaller, pressure on the remaining structures increases. Studies that have looked at great toe amputation in patients with diabetes have found an increase in plantar pressure and the development of new deformities and ulcerations after amputation.16,17 As loss of parts of the foot occurs, the mechanics of the foot change, transferring stresses to new areas with the potential for ulceration.
Plantar ulceration has been associated with lower extremity peripheral neuropathy and excessive plantar pressures.18–21 Pressure on the soft tissues of the foot is related to three variables: the magnitude of the force applied to the foot, the amount of surface over which the force is applied, and the length of time over which the force is sustained.22 Because much of the focus in treating and preventing foot ulcers is on reducing pressure, one must understand the relationship of pressure to these three variables. The following formula should be considered:

As indicated, anything that increases the magnitude of the force applied to the foot or decreases the area over which the force is applied increases pressure and makes tissue damage more likely. Immediate injury can occur from extremely high force applied over a small area, as when a patient steps on a tack or piece of glass. Injury occurs because tremendously high pressure exceeds the tensile strength of the skin. Pressure on the foot can also become excessive when a moderate amount of force is repeatedly applied over a small surface area—when bony deformities cause small localized areas of weight bearing or when partial foot amputations decrease the patient’s weight-bearing surface. The force applied to the foot (body weight) remains essentially the same, but the actual pressure on the tissues is greater because of reduction of the surface area. In patients with diabetes, factors such as limited joint mobility,23–27 structural abnormalities,28–30 and previous amputation16,17 can lead to increased force or decreased surface area. All of these are associated with increased plantar pressures and ulceration.
Further complicating this picture is the time factor. In looking at tissue ischemia and resultant ulceration, Kosiak found an inverse relationship between the amount of pressure applied to tissues and length of time that the pressure was sustained.31 Low pressures sustained over long periods of time caused tissue necrosis. This is the mechanism of tissue injury when decubitus ulceration occurs in bedridden, poorly mobile patients. Tissue necrosis also occurs along the medial or lateral borders of the feet or tops of hammer toes when patients wear shoes that are too tight. Kosiak found that as the magnitude of pressure increased, fewer hours were necessary to induce injury.
The most common cause of skin breakdown in the neuropathic foot is repeated bouts of moderate pressure during every-day walking.32 Dr. Brand demonstrated this fact by applying repeated bouts of moderate pressure to the anesthetized foot pads of rats. Repeated bouts of moderate pressure caused inflammatory changes, and with continued repetition, this inflammation progressed to ulceration.22 For health professionals who care for patients with diabetic foot problems, two facts from this research hold particular significance. First, when the inflammatory changes (heat and swelling) began to persist from one day to the next, breakdown of the tissue was prevented by discontinuing the repeated stress. Second, breakdown was prevented by either decreasing the amount of pressure per repetition or by reducing the number of repetitions. The findings of Brand and Kosiak suggest that the variables of force, area, and time and repetition contribute to tissue breakdown and that changing one or more of these variables must be considered in the treatment plan for patients with a high-risk foot.
Autonomic Assessment
Autonomic changes represent the third category of changes associated with polyneuropathy. With roles including the regulation of moisture and blood flow, as well as controlling hair and nail growth and overall skin integrity, the autonomic system is crucial to healthy feet. Cracks and fissures in the foot, as well as nail pathologies, can predispose people to ulceration or infection. As these are all end products of autonomic dysfunction, patients need to be educated on how to prevent them from occurring. Patients with autonomic dysfunction, most commonly from diabetes, should be educated to moisturize their feet often so as to avoid drying and cracking of the skin. Creams or non–alcohol-based lotions should be applied liberally to the feet and legs, but the areas between the toes should be avoided as the excess moisture can lead to fungal infections. Not only is moisturized skin more comfortable, it is also stronger and less likely to develop cracks and fissures, which are easy entries for infections. If nails are too thick to be trimmed safely at home with regular nail clippers, the patient should be encouraged to seek professional help for nail care.
One of the most damaging outcomes related to dysfunction of the autonomic system is diabetic neuropathic osteoarthropathy, also known as Charcot foot. This destructive process can significantly alter the bony architecture of the foot, and can lead to excessive plantar pressures33 and subsequent ulceration if left unchecked (Figure 18-7). This process was first recognized in patients with syphilis during the nineteenth century by Jean-Martin Charcot. Although several neuropathic diseases, including syphilis and Hansen’s disease, can cause a Charcot arthropathy, it is most commonly seen in persons with diabetes.34 Charcot foot is a progressive disorder that leads to joint dislocation, fractures, and deformity of the foot.35
Charcot surmised that when the proper functioning of the autonomic system was impaired by disease, it led to an increase in blood flow to the bones, which then led to bone resorption. Over time, this became known as the neurovascular theory.36 A second theory states that development of a Charcot foot is related to trauma in an insensate foot. Because of the lack of sensation, there is no perception of the trauma, and thus no adjustments to compensate for it. If the joint continues to be loaded, it will stay inflamed and eventually break down. This became the neurotraumatic theory.36 In most experts’ opinions, the cause of Charcot foot is likely to be some combination of the two theories.35,37 A commonality of the two theories is that Charcot foot starts with an insensate foot.36,38,39 As a result, the Charcot foot is most likely to occur in someone with sensory neuropathy, adequate blood flow, and a history of trauma, whether they were aware of it or not. Upon clinical examination, the foot is erythematous, edematous, has an elevated skin temperature, and a bounding pulse indicative of excessive blood flow.39,40
Charcot foot can become debilitating if not recognized early enough to arrest the development of the rocker bottom deformity that is characteristic of the disease. It is often misdiagnosed because no single diagnostic test can confirm its presence. Medical history, clinical manifestations, and radiographic findings all must be considered. Unfortunately, the clinical presentation of a red, hot, swollen foot often leads to the diagnosis of cellulitis, which is treated with antibiotics. During the time the patient is being treated with antibiotics for an infection that does not exist, they are continuing to damage the foot by walking on it. Radiographs taken in the acute phase are not sensitive to the development of neuropathic fractures and bone scans do not differentiate Charcot foot from osteomyelitis. MRI, on the other hand, is capable of identifying bone injury prior to complete fracture.37,40 MRI may be cost-prohibitive, making the medical history and physical examination that much more important.
Charcot foot should be suspected if a patient with neuropathy presents with sudden onset of localized swelling, warmth, and erythema in the absence of an open wound. Appropriate treatment for Charcot foot should be initiated until this condition is ruled out on further testing. During acute Charcot arthropathy, joint destruction can be minimized by immobilization in a total-contact cast and avoidance of weight bearing until signs of healing become apparent (decreased temperature, decreased swelling, and improved radiographic findings). Both lack of compliance with non–weight bearing and use of orthotic devices in place of cast immobilization have shown prolonged healing times.41,42 When cast immobilization is discontinued, the use of an orthotic device for continued protection of the joints during the initial return to weight bearing should be considered.33,42
The architectural changes that occur in the foot secondary to neuropathic osteoarthropathy result in high-pressure areas.33 Because of this, following the period of immobilization and limited weight bearing, patients with a history of Charcot foot must be provided with appropriate footwear to stabilize the foot and reduce plantar pressure. Surgical intervention may be indicated for unstable or severely malaligned fractures or dislocations, which create problems with recurrent ulceration, fitting of shoes, ability to ambulate,43,44 as well as recalcitrant ulcers.45 Some of these procedures require months of immobilization and avoidance of weight bearing, which can be difficult for many patients with diabetes and neuropathy. Such surgery is usually advocated only if nonsurgical management fails.
Footwear Assessment
The analysis of the high-risk foot truly begins before the patient sits on the examination table. The type and appearance of the footwear they are wearing can give insight as to the cause of their pathology. Shoes that either do not fit properly or are excessively worn can cause problems including blisters, calluses, and wounds. On the other hand, shoes that someone refuses to wear are not useful as they will just sit in the closet.
Characteristics of the proper shoe for the high-risk foot include:
• Snug fit at the heel to prevent pistoning (moving up and down) of the heel
• Wide toe box to accommodate for deformities such as bunions and hallux valgus
• Deep toe box to accommodate claw/hammer toes and molded inserts
It is recommended that people shop for new shoes in the mid to late afternoon to ensure the best fit. Because foot size changes throughout the day, a shoe purchased to fit the foot early in the morning may be too small by late evening, and conversely a shoe bought at night may be too large for the foot in the morning.
Gait and Balance
Motor neuropathy causes weakness of foot and ankle musculature that may result in gait deviations that change plantar pressure patterns or contribute to instability. Gait and balance are also affected by damage to sensory nerves, which leads to an inability to sense where the foot is in space. The use of ankle-foot orthoses or shoe modifications may help restore a more normal gait, stabilize joints, or improve balance. Studies have found that patients with peripheral neuropathy secondary to diabetes have problems with gait and postural stability.46–50 In examining a patient with a high-risk foot, physical therapists must include not only the patients’ foot problems but also their overall functional status. To reduce the morbidity associated with falls, recommendations that address safety and function should be included in the treatment plan.
Wound assessment
Although it is clear that the most effective way to prevent amputations is to avoid getting wounds in the first place, that is not always possible. When a wound does develop, regardless of the etiology, a thorough wound assessment becomes a necessity. The comprehensive wound assessment begins with a thorough patient history, which helps the clinician not only gain a better understanding of the cause of the wound, but also forecast healing rates of the wound more accurately. Refer to the previous section on risk factor assessment for more information pertaining to patient history. It is often helpful to take the entire patient history prior to undressing the wound, as there is a tendency to focus solely on the wound once it is visible and forget about other factors that may be important.
Once the patient history is reviewed, the wound can be carefully undressed. In addition to the components already discussed for the evaluation of the high-risk foot, the assessment also includes an examination of the immediate wound and periwound area. The wound should be assessed for location, color, odor, size/depth, and drainage type and amount, and the periwound tissues should be assessed for any abnormalities (Figure 18-8).
Location
If a thorough medical history has been taken, the examiner may have a good hypothesis as to the cause of a wound before even seeing it. The objective examination can either confirm or refute this hypothesis. One of the first objective findings that should be documented is wound location. Although traumatic wounds can occur in any anatomic location, many of the common wound etiologies tend to occur most frequently in certain areas. Diabetic foot (neuropathic) ulcers are most common on the plantar aspect of the digits and MTHs, more specifically, the great toe and first MTH, but they can occur in any area of high stress.51 Ulceration secondary to neuropathy is also common on the dorsum of the toes, as well as bony prominences, such as the lateral aspect of the first and fifth MTHs and the base of the fifth metatarsal, and anywhere a shoe or brace may be rubbing. Wounds secondary to vascular insufficiency can occur in any location that has impaired blood flow, but are most frequently found on the toes, dorsum and lateral aspects of the foot, as well as the lateral leg. In contrast, wounds of venous origin tend to be in what is often referred to as the “gaiter” area, just proximal to the medial malleolus. It should be noted that these are general guidelines, and an accurate diagnosis cannot be made based solely on location. When describing wound location, the clinician should be as precise as possible, often using bony landmarks as descriptors. This becomes increasingly important when multiple wounds are present.
Wound Color
A simple designation for wound color is to use the red-yellow-black staging system, which was first published in the United States in 1988 and had been used in Europe prior to that.52 Red wounds are generally healthy, well vascularized, and are progressing through the normal stages of healing. The red appearance is attributed to the deposition of highly vascularized collagen, known as granulation tissue. This tissue is fragile, and may bleed with excessive force or friction. Granulation tissue that bleeds with minimal pressure or has a dusky appearance is called friable and should be investigated further as it is typically a sign of increased bacteria present in the wound. Yellow wounds indicate fibrinous slough or infection is present. Slough has a stringy, adherent characteristic and can be removed by a variety of methods, which are discussed later in this chapter (Preparing the Wound Bed by Eliminating the Source of Inflammation or Infection). Wounds also may have a black appearance, which signifies the presence of eschar. Eschar is often hard to the touch, but can be soft or boggy if there is a lot of fluid present. In most cases, it is beneficial to remove the eschar because the necrotic tissue promotes the proliferation of bacteria. Several instances when this is not advised are intact eschar on heels and vascular wounds that would not be able to heal following debridement. In addition to the red-yellow-black system that is focused on the dermis, the clinician must also be aware of deeper structures that may be apparent in the wound bed. The first tissue encountered beneath the dermis is known as subcutaneous tissue, fat, or adipose. This should have a pale yellow, moist appearance when healthy, but dries out and darkens when it is nonviable. Healthy, muscle has a bright red color, and the striations are often visible in the tissue. Damaged muscle takes on a dusky gray appearance with a much-less-pliable texture. The remaining structures that will be encountered in a deep wound bed—ligaments, tendons, bone—all should be white if well vascularized. If these tissues are compromised, they will take on a dusky yellow appearance, and continue to darken as damage proceeds.
For documentation purposes, the use of percentages is helpful in describing the wound color. For example, a wound could be 80% red, with 20% firmly adhered yellow fibrin. It is also suggested that the percentage should be documented before and after treatment if there is any significant change in the wound appearance.
Odor
One of the most troubling aspects of a wound from a patient’s perspective is odor. Most significant wounds will have some odor when dressings are removed. As a clinician, it is important to know whether or not the odor is caused by infection, or simply from the dressing having been in place for an extended period. Before making this determination, dressings should be removed and the wound should be rinsed with sterile water or saline. Odors that are eradicated are likely caused by drainage on the dressings. This is especially true of occlusive dressings, such as hydrocolloids. If cleansing the wound does not eliminate the odor, it is more likely caused by necrotic or infected tissue. Wounds with a strong odor often contain anaerobic and aerobic bacteria, and are referred to as polymicrobial53; anaerobic bacteria create odor by releasing compounds including putrescine and cadaverine. These odors can be extremely strong, and are often described as acrid smelling. Aerobic bacteria also are capable of producing foul odors. Because the strength of an odor is subjective, it is recommended that descriptions such as sweet, fishy, necrotic, putrid, and the like also be included in the assessment of the odor. Infection should be considered when previously odor-free wounds develop an odor, but it should also be pointed out that some infections do not produce any odor at all.
Size
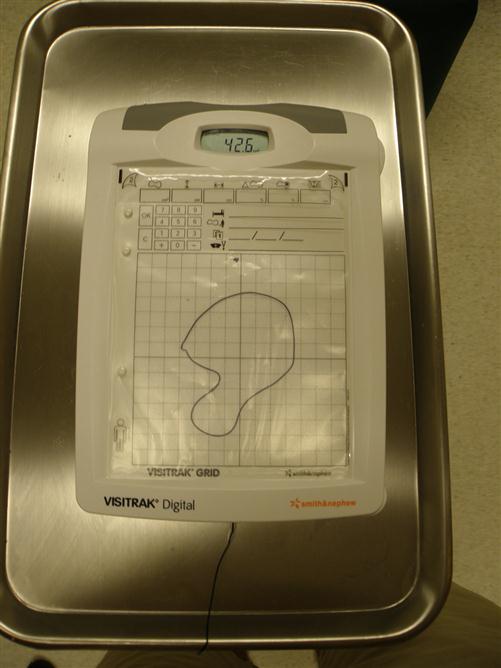
Wound size should be documented on a routine basis as it is an easy way to monitor progress in wound healing. For most wounds, unless they are perfectly symmetrical, a diameter or even length and width may not give an accurate representation as to the true size of the wound. When length and width are used, the largest length is recorded, and the width is recorded perpendicular to the length. Although improvements can be seen as these numbers decrease, it is difficult to accurately calculate a total surface area for the wound or a percent area reduction because wounds are irregularly shaped. Alternative methods include photography with a transparent film over the wound, wound tracings with transparent film, and digital cameras that can calculate the surface area of the wound. All of these options enable the clinician to calculate surface area, and percent reduction in size (Figures 18-9 and 18-10).

Regardless of the method used to calculate wound size, the orientation of the wound should be standardized to ensure that subsequent measurements are assessing the same dimension. Bony landmarks can be used for this purpose, but it is most common to describe length in a cephalocaudal (head-to-toe) fashion and width perpendicular to that. Unfortunately, the largest dimensions of most wounds will not line up perfectly with axes along the cephalocaudal and perpendicular plane. For this reason many clinicians describe wound orientation using a clock face, with 12 o’clock being at the head and 6 o’clock at the feet. Using this system, a wound could be described as 6 cm in length from 10 o’clock to 4 o’clock and 3 cm in width from 1 o’clock to 7 o’clock. Undermining, tunneling, or any other abnormality in the wound can also be described using the clock face, which will help with consistency in measurement, especially if another clinician is measuring the wound.
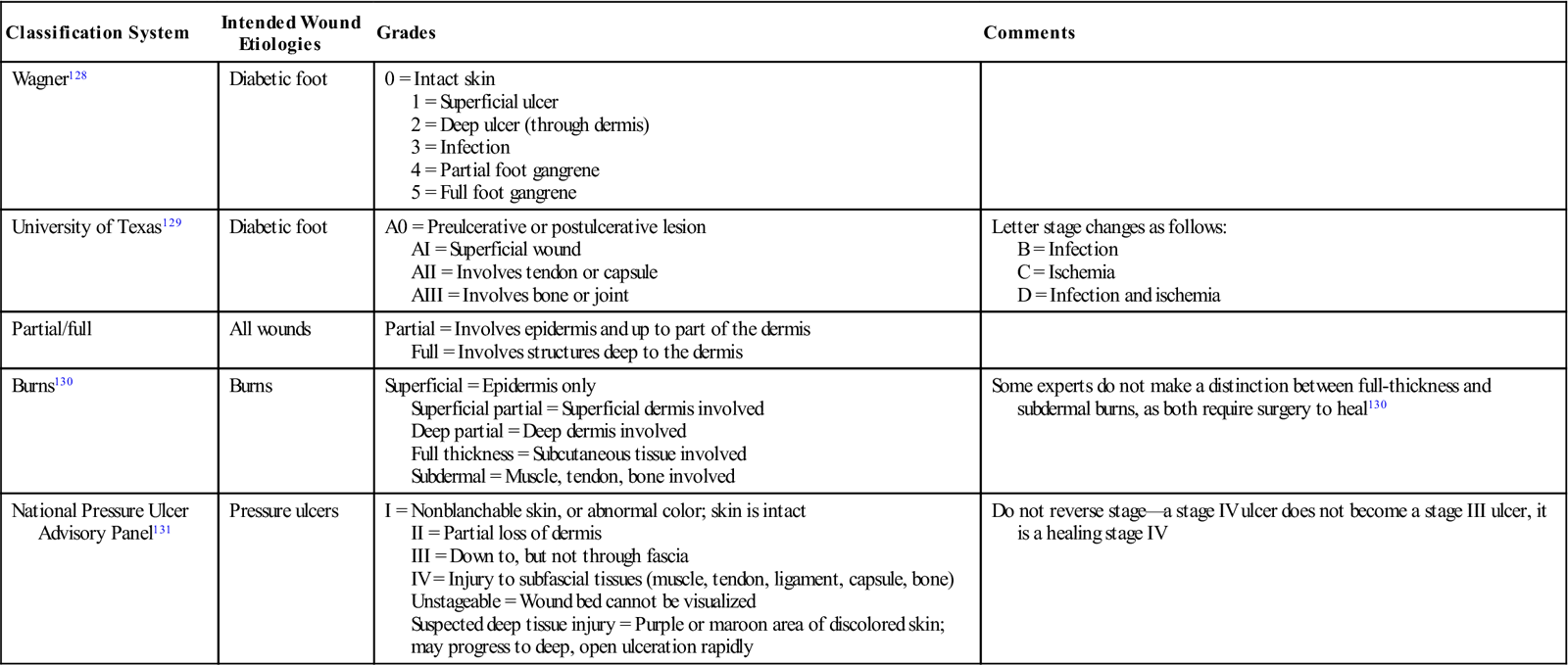
Depth
A thorough understanding of anatomy is necessary for an accurate staging of wounds. In turn, an accurate staging of wounds relies on being able to assess wound depth properly. Before depth can be measured, the wound must be free of nonviable tissue so the wound base can be visualized or probed. The wound can then be probed with a sterile probe held perpendicular to the skin surface. As wounds do not all have a uniform depth throughout, the deepest point should be measured and the location where the measurement was taken should be documented. After the depth measurement is obtained, wounds can be classified in several ways, depending on the etiology. Table 18-1 reviews different wound classification systems that rely on wound depth as a part of the staging criteria.
Table 18-1
| Classification System | Intended Wound Etiologies | Grades | Comments |
| Wagner128 | Diabetic foot | 0 = Intact skin 1 = Superficial ulcer 2 = Deep ulcer (through dermis) 3 = Infection 4 = Partial foot gangrene 5 = Full foot gangrene | |
| University of Texas129 | Diabetic foot | A0 = Preulcerative or postulcerative lesion AI = Superficial wound AII = Involves tendon or capsule AIII = Involves bone or joint | Letter stage changes as follows: B = Infection C = Ischemia D = Infection and ischemia |
| Partial/full | All wounds | Partial = Involves epidermis and up to part of the dermis Full = Involves structures deep to the dermis | |
| Burns130 | Burns | Superficial = Epidermis only Superficial partial = Superficial dermis involved Deep partial = Deep dermis involved Full thickness = Subcutaneous tissue involved Subdermal = Muscle, tendon, bone involved | Some experts do not make a distinction between full-thickness and subdermal burns, as both require surgery to heal130 |
| National Pressure Ulcer Advisory Panel131 | Pressure ulcers | I = Nonblanchable skin, or abnormal color; skin is intact II = Partial loss of dermis III = Down to, but not through fascia IV = Injury to subfascial tissues (muscle, tendon, ligament, capsule, bone) Unstageable = Wound bed cannot be visualized Suspected deep tissue injury = Purple or maroon area of discolored skin; may progress to deep, open ulceration rapidly | Do not reverse stage—a stage IV ulcer does not become a stage III ulcer, it is a healing stage IV |
Drainage
The ideal wound will have enough moisture to prevent desiccation of the wound bed, but not so much that it causes breakdown of periwound tissues. The characteristics of wound drainage will vary depending on multiple factors, including wound location, vascular status, and presence of infection. Drainage should be classified by amount and type to accurately describe what is occurring in the wound. Assessing the amount of drainage is somewhat subjective in that it is not practical, or even possible in many cases, to weigh the amount of exudate from the wound. Instead, the clinician describes the amount of exudate along a continuum, such as the one below:
This can be difficult to quantify, especially for the inexperienced clinician, as different dressings will absorb vastly different amounts of fluid and thus could make a heavily draining wound appear drier, or vice versa. Wounds with underlying arterial insufficiency tend to be drier because less circulation is getting to the wound bed, whereas patients with wounds that are venous in nature often experience heavy drainage because of the edema present. If the amount of exudate increases, and a reason is not clearly related to changes in treatment (i.e. surgical intervention to increase blood flow, discontinuation of compression therapy, or resting in dependent positions), then infection should be considered as a likely cause. The presence of infection causes the wound to remain in the inflammatory phase of wound healing, which results in increased drainage. Infected wounds often exhibit purulent drainage, which can be yellow, green, tan, or even creamy or cloudy. These wounds often require a combination of local and systemic agents to treat the infection. In addition to purulent drainage, drainage can also be serous (watery), sanguineous (bloody), or serosanguineous (pink or reddish, watery).
Periwound Skin
The area immediately surrounding a wound, known as the periwound skin, should be assessed carefully because it can give clues as to the state of the wound. Evidence of excessive pressure, excess moisture, decreased vascularity, and the presence of infection can all be found in the periwound skin with a quick visual inspection and palpation. Table 18-2 lists periwound findings and their significance.
Table 18-2
| Appearance | Description | Significance |
| Callus | Area of hyperkeratosis, typically in response to high pressures54,132,133 | Frequently associated with neuropathy and/or bony deformity. Indicates area susceptible to breakdown132 |
| Blister | Fluid-filled area causing separation of epidermis from dermis | Shearing forces from rubbing on shoes, brace, bed, etc.; may also be caused by adhesive dressings on skin |
| Erythema | Redness | Indicates inflammation caused by local stress or infection; redness in immediate periwound area is normal in acute wounds, but excessive redness or redness that persists for 30 to 60 minutes after the stress is removed requires intervention; erythema associated with infection is often well demarcated; if red streaks are noted (lymphangitis), consult physician as it is a sign of spreading infection |
| Maceration | Changes in tissue caused by excessive moisture | Can lead to skin breakdown; may be a result of excessive sweating, heavy wound drainage, incontinence, or inappropriate dressings |
| Induration | Hardening of the tissue because of edema | Chronic edema impairs wound healing; induration is often associated with infection or venous disease |
| Hemosiderin | Brownish discoloration of the skin around a wound. Associated with deposition of hemoglobin in extravascular tissues | Often associated with venous disease |
| Excoriation | Wearing away of the skin | Indicates an area of trauma; often preceded by maceration and/or blistering |
| Presence of scars | A scar is the final result of a previous injury | May give clues to the chronicity of the problem as well as the extent of damage in the area |
| Temperature | Can be palpated or assessed with infrared thermometer; is typically compared with adjacent areas or to contralateral side | Nonspecific indicator of inflammation; helpful to monitor “hot spots” that may be at risk of breakdown, or for resolution of a Charcot fracture |
| Edema | Swelling in the tissues | Bilateral edema suggests a systemic problem; unilateral edema indicates a localized problem; can occur with infection, inflammation, venous dysfunction, and lymphedema; consider Charcot foot if insensate |
| Other changes | Taut, shiny, hairless, cracked skin | Taut, shiny skin with a loss of hair indicates impaired blood flow; cracked skin is associated with aging, diabetes, or vascular disease. Important to moisturize skin frequently |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree