Chapter 136 Vitamin K
Forms, Sources, Absorption, and Metabolism
Physiologic Roles of Vitamin K: Effects of Normal to Supraphysiologic Doses
Interactions with Other Vitamins
Dosing Considerations: Prevention versus Therapy
 Forms, Sources, Absorption, and Metabolism
Forms, Sources, Absorption, and Metabolism
Forms: K1, K2, and K3
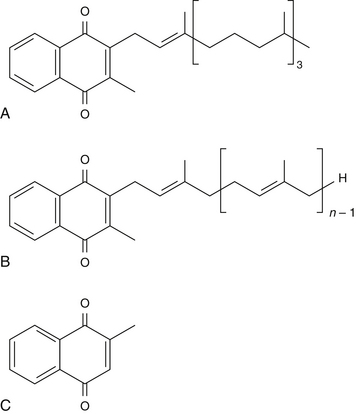
The currently known forms of vitamin K can be grouped in three categories: vitamin K1 (one type), vitamin K2 (14 types), and vitamin K3 (one type) (Figure 136-1). Vitamins K1 and K2 are fat-soluble, whereas vitamin K3 is water-soluble.1 Technically, only vitamin K1 is recognized as a true vitamin, essential for human and animal well-being. Vitamins K2 and K3 can be derived as metabolites of vitamin K1 in various tissues or the gastrointestinal tract in animals or humans. However, there may be many clinical situations that can benefit from supplementation with vitamin K2 (from diet and/or supplements) or from the intravenous administration of vitamin K3. Oral vitamin K3 is used only in animal nutrition; for humans, it is currently allowed only for research purposes.2
The structures of vitamins K1, K2, and K3 are similar in regard to their core molecule, called menadione (or 2-methyl-1,4-naphtoquinone). Vitamin K3 is simply composed of the core molecule menadione (see Figure 136-1, C), whereas vitamins K1 and K2 contain the core molecule menadione plus specific side chains that distinguish them as follows3:
• In addition to the menadione core, vitamin K1 contains a side chain of one unsaturated isopentenyl unit and three saturated isopentyl units (see Figure 136-1, A).
• In addition to the menadione core, each member of the vitamin K2 family contains a side chain of specific length, anywhere from 1 to 14 repeats of unsaturated isopentenyl units (see Figure 136-1, B). The length of the side chain determines the name of each type of vitamin K2 as follows: MK-1(with 1 unit), MK-2 (with 2 units), and so on, through MK-14 (with 14 units). In this review, a K2 designation is added in front of their names, as follows: K2 (MK-1), K2 (MK-2 through MK-14) in order to avoid confusion with vitamins K1 and K3.
On average, it is estimated that 80% to 90% of dietary vitamin K intake is typically derived from vitamin K1, with the rest coming from vitamin K2.4
Main Aspects of Vitamin K1 (Phylloquinone or Phytomenadione)
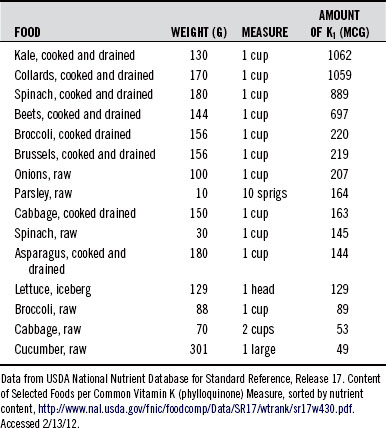
Vitamin K1, also called phylloquinone or phytomenadione, is synthesized only by plants or algae, where it is bound in the thykaloid membranes of chloroplasts and participates in the electron transport chain of photosynthesis. Vitamin K1 occurs in significant amounts (50 to 800 mcg/100 g food) in certain vegetables, vegetable oils, seeds, algae, and in small amounts (<50 mcg/100 mcg food) in the rest of the vegetable and animal foods, as listed in Figure 136-2. See Table 136-1 for the typical yield of vitamin K1 in common measures of select vegetables, which are the most significant sources of vitamin K1 of all vegetable foods.
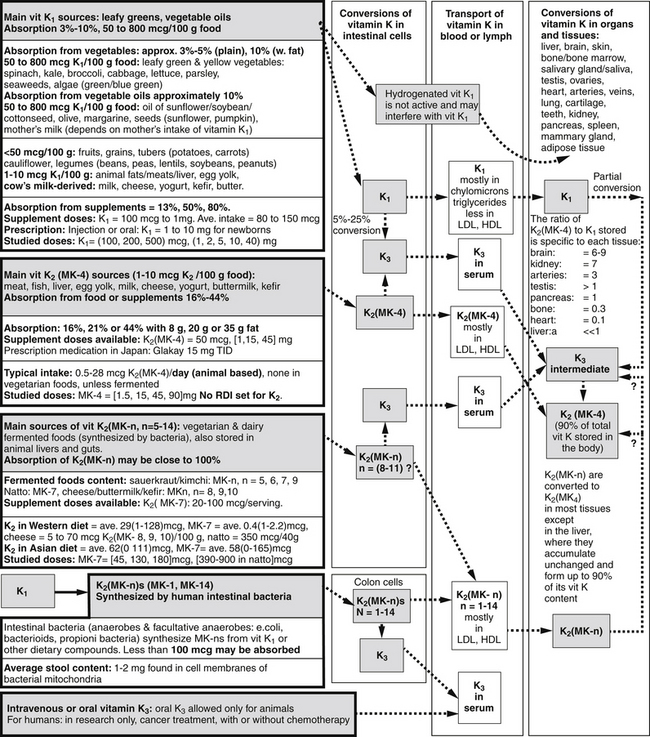
Figure 136-2 Vitamin K forms, sources, absorption, conversions, transport, and distribution in the blood and organs.
Vitamin K1 is also available for oral or intramuscular injection to correct clotting deficiency in newborns or to compensate for anticoagulant overdose in adults. Studies are conflicting in regard to the concern that vitamin K1 injection may increase the risk of various cancers, including leukemia in infants. Recent research seems to have established that the risk was related to the route of administration, specifically to injection and not via the oral route. Also, the safest and most reliable way to increase vitamin K1 in the unborn fetus and reduce the risk of bleeding after birth seems to be by increasing the mother’s vitamin K status, as some studies suggest.5
Absorption
Absorption of vitamin K1 varies considerably depending on its source. When it is delivered in a vegetable, its bioavailability is low (3% to 10%) because it is trapped in the chloroplast.6 Cooking and/or mechanical processing (blending, juicing) of the vegetables or pressing the oil out of the vegetable seeds (such as sunflower seeds) increases the vitamin’s bioavailability and absorption up to as much as 50% as compared with the raw vegetable.7
By adding dietary fat to the vitamin K1-containing food, absorption of the vitamin can be doubled; it may then reach 10% to 15%.8 Following is a summary of estimated vitamin K1 absorption values, obtained by comparing a number of studies9–17:
• Absorption from raw vegetables (such as spinach or broccoli): 3% to 5%; some suggest as high as 10%.
• Absorption from cooked vegetables without fat: some have found no difference compared with raw vegetables.
• Absorption from cooked vegetables with fat: approximately 2.5 times the absorption from raw vegetables.
• Absorption from vitamin K1 dissolved in vegetable oil: approximately 50% to 80%.
• Absorption from a synthetic vitamin K1 supplement: approximately 10% (if mixed in a capsule with 85% cellulose) and approximately 80% (if mixed in an emulsion containing lecithin and a bile acid).
Exposure to ultraviolet (UV) light inactivates vitamin K. When oils containing vitamin K1 are hydrogenated (during industrial processing, cooking, frying, or baking), a big percentage (40% to 50%) of the vitamin K1 content is also hydrogenated. Studies have shown that hydrogenated vitamin K1 has very little biological activity.18 It is important to note that a large section of the population derives a majority of its vitamin K1 from vegetable oils as opposed to vegetables, so the effect of vitamin K inactivation by hydrogenation may have an important impact on common deficiencies of vitamin K, which may be higher than estimated from just vitamin K1 intake surveys.
Transport, Metabolism, and Distribution in Human Tissues
Once ingested, vitamin K1 can be metabolized through various routes in the body (see Figure 136-2).
Vitamin K1 is transported initially in the chylomicrons through lymph and blood to the liver and other tissues. Once taken up by various tissues, vitamin K1 may be stored and utilized unchanged, while part of it may be converted to K2 (MK-4). For unclear reasons, the steady-state ratio of K1/K2 (MK-4) stored in each tissue seems to be specific to each tissue. See Figure 136-2 for a list of these ratios in various tissues and organs.19
One study estimates that 5% to 25% of the absorbed vitamin K1, the same as various K2 forms, is converted to K3 in the intestinal cells.20 Various cells in the body may take up vitamin K3 and convert it to vitamin K2 (MK-4). A portion of vitamin K3 is converted to K2 (MK-4) in each tissue.21
One study looked at the vitamin K stored in the rat brain in response to supplementation with either vitamin K1 or vitamin K2 (MK-4).20 Contrary to what was expected, the results showed that supplementation with vitamin K1 was able to increase the brain content of K2 (MK-4) more than direct supplementation with vitamin K2 (MK-4).
Main Aspects of Vitamin K2
A Family of Menaquinones: K2 (MK-1) through K2 (MK-14)
Significant Menaquinones Available from Foods and Supplements: K2 (MK-4) and K2 (MK-7)
Vitamin K2 is not considered a vitamin in the true sense because theoretically it is not an essential nutrient; it is debatable whether it is needed in addition to vitamin K1 for maintaining normal health. This is because animal and human tissues, as well as their intestinal bacteria, are typically able to synthesize vitamin K2 from the vitamin K1 ingested. It is not clear either whether vitamin K2 can fulfill all the functions that vitamin K1 exerts, since there is no proof that it converts into vitamin K1.
Like the essential role of vitamin K1 in the energy production (photosynthesis) of plants or algae, vitamin K2 is an obligatory component of the electron transfer pathway in the mitochondria of certain bacteria, analogous to the role of the quinone coenzyme Q10 in animal mitochondria.22
Vitamin K1 Conversion to Vitamin K2 (MK-4): Tissue Distribution of Vitamin K1 versus Vitamin K2 (MK-n), n = 1 to 14
Many studies have shown that various long-chain K2 (MK-n)s are converted to K2 (MK-4) in all tissues with the exception of the liver. For example, dietary supplementation with K2 (MK-7) from natto was shown to result in a significant increase of K2 (MK-4) in bone, whereas no MK-7 was detected in the bone.23
Dietary Sources of Various Forms of Vitamin K2
Animal Foods:
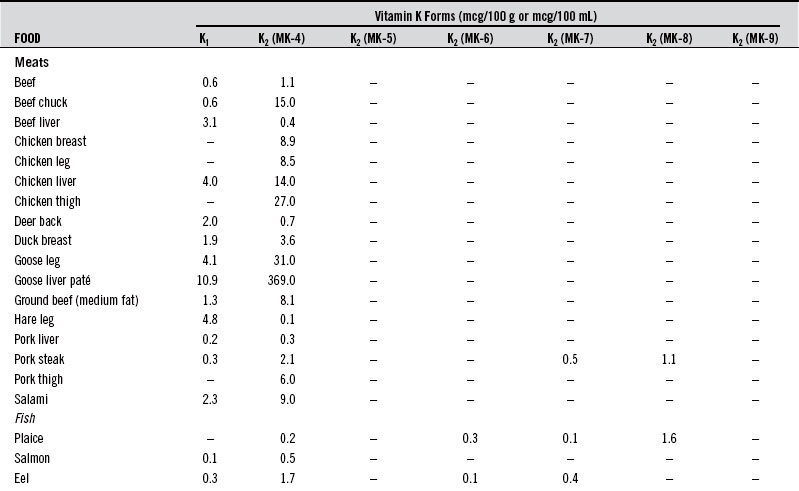
Meats (2 to 3 mcg/100 g), egg yolk (10 mcg/one egg), and milk. These sources preferentially provide the K2 (MK-4) form along with similar amounts of vitamin K1. See Table 136-2 for a listing of the vitamin K2 content of various foods. Table 136-2 lists the vitamin K2 content of select foods from three studies in the United States, Holland, and Japan.24
The content of vitamins K1 and K2 in human milk depends on the mother’s intake of these vitamins.25 The same may be true for cow’s milk and other animal milks. Similarly, the vitamin K content of animal tissues may be lower for animals fed mostly corn versus those that are exclusively grass-fed, although no studies have measured this. The vitamin K2 content of animal-derived food may be higher when they are supplemented with vitamin K3 (a common practice). Since vitamin K3 supplementation has proved detrimental for humans, it may be of questionable safety for animals. Also, continuous antibiotic treatment of the animals (to enhance growth) may impair their intestinal bacterial production of vitamin K2.
Fermented Foods (Animal or Vegetable)
Various forms of vitamin K2 are produced by certain bacteria, ranging from K2 (MK-4) to K2 (MK-12) (see Table 136-2):
1. Animal origin: cheese and other fermented milk products (yogurt, kefir, buttermilk, sour cream) provide vitamin K2 forms mostly as K2 (MK-8) and K2 (MK-9).
2. Vegetable origin: natto, sauerkraut, kimchi. For example, the bacteria specific to natto (a fermented mix of soybeans and rice) will provide vitamin K2 mostly in the K2 (MK-7) form; bacteria in foods like sauerkraut (pickled cabbage) provide vitamin K2 in a wide variety of forms, such as K2 (MK-5) through K2 (MK-9).
Vitamin K2 Produced by Human Intestinal Bacteria
Certain bacteria residing in the human intestinal tract convert the ingested vitamin K1 or other dietary components (such as alpha-ketoglutarate) to various forms of vitamin K2 (MK-n). The types of bacteria that have this property are mostly gram-negative, such as Bacteroides fragilis, Propionibacterium, and particular strains of E. coli (normal gastrointestinal resident strain, not necessarily pathogenic). Certain strains of Lactobacillus were also found to produce vitamin K2, although these are not the commonly known strains of Lactobacillus or probiotics used in supplements or found in yogurt. Vitamin K produced by the gut bacteria may represent a significant portion of the total vitamin K2 acquired by some people if their vitamin K status is marginal.26
Vitamin K2 Absorption and Transport
Very few studies have evaluated the absorption of various forms of vitamin K2.27 There is some consensus among researchers that the longer the vitamin K2 side chain is, the more lipophilic it is, with K2 (MK-4) being less lipophilic than the longer-chain K2.
One study administered K2 (MK-7) from a natto extract and claimed to have obtained “almost complete” absorption.
Vitamin K2 seems to be preferentially transported by the plasma lipoproteins—low-density lipoprotein (LDL) and high-density lipoprotein (HDL)—and have very different plasma half-lives; for example, the half-life of K2 (MK-4) is around 1 to 2 hours, whereas that of K2 (MK-7) is around 2 days. Some hypothesize that K2 (MK-4) is taken up by the tissues a lot faster because it is ready to be stored and utilized as such, whereas K2 (MK-7), for example, tends to be converted slowly to K2 (MK-4), before it is stored in various tissues. K2 (MK-7) can serve as a “time-release” source of K2 (MK-4) (Table 136-2).
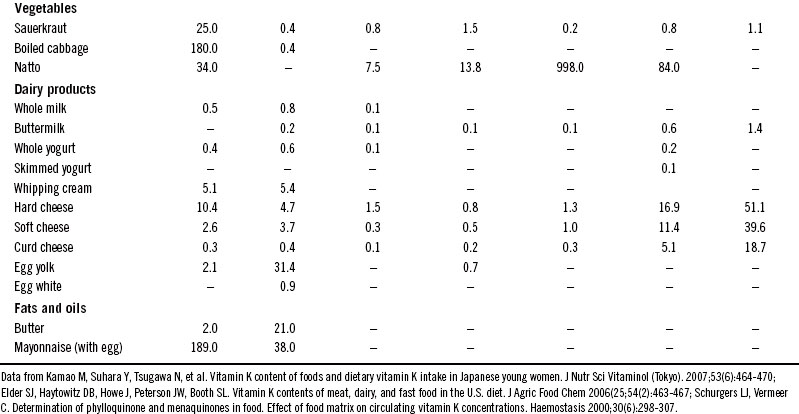
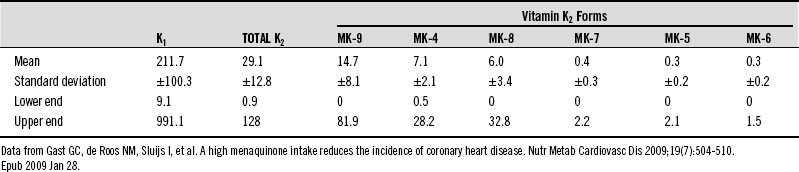
Average Vitamin K2 Intake and Comparative Absorption between Vitamin K2 and Vitamin K1Table 136-3 shows the average intakes of various forms of vitamin K from an epidemiologic study of a Dutch population. The particularly high contribution from MK-9, MK-4, and MK-8 is most likely due to the high cheese consumption in Holland.Even though the actual intake of vitamin K1
Table 136-3 shows the average intakes of various forms of vitamin K from an epidemiologic study of a Dutch population. The particularly high contribution from MK-9, MK-4, and MK-8 is most likely due to the high cheese consumption in Holland.
Table 136-3 Average Intake of Various Forms of Vitamin K in a Dutch Population (all values in µg/day)
Vitamin K2 Supplement Forms and Doses Available
Vitamin K2 is currently available as a supplement in only two forms:
1. Vitamin K2 (MK-4) (menaquinone-4 or menatrenone), which is provided in a synthetic version. It is typically available in doses in the range of 40 to 50 mcg, 1 mg, 15 mg, or 45 mg in stand-alone vitamin K formulas, vitamin D combination with vitamin K formulas, or bone-specific formulas. It is also available as a prescription medication in Japan, called Glakay, in 15-mg doses (with the indication of three times daily).28
2. Vitamin K2 (menaquinone-7, MK-7) is available either in a synthetic version or as a concentrated extract from the Japanese fermented food natto. It can, of course, be ingested with the natto food itself, which provides an average of 350 mcg/50 g in each serving. K2 (MK-7) is also found in much smaller amounts in foods such as fermented cabbage (sauerkraut and kimchi) or cheeses and fermented milks; see Table 136-3. The average vitamin K2 intake found in young Japanese women was 61.7 mcg. From this, K2 (MK-7) typically represents 57.4 mcg owing to the common consumption of natto.
 Physiologic Roles of Vitamin K: Effects of Normal to Supraphysiologic Doses
Physiologic Roles of Vitamin K: Effects of Normal to Supraphysiologic Doses
Mechanisms of Action of Vitamins K1 and K2
Vitamin K’s actions in human physiology are very complex:
1. Posttranslational modification (through carboxylation) of a number of functional proteins, called vitamin K-dependent proteins (VDKs)
2. Modulation of inflammation through downregulation of cytokine IL-6 and prostaglandin E2 (PGE2) (by inhibiting COX-2)
3. Downregulation of cell signaling proteins (produced downstream of mevalonate and 3-hydroxy-3-methylglutaryl-coenzyme A [HMG-CoA]), which affect cell differentiation and apoptosis
4. Neurologic effects through modulation of galactocerebroside sulfotransferase enzyme (GST)
5. Genetic expression modulation
Vitamin K activates a variety of VKDs throughout the body by carboxylating a specific number of the glutamatic acid residues they contain, which become, as a result, gamma-carboxyglutamate residues, also called Gla. One molecule of vitamin K1 or K2 can be recycled many times, so it is used multiple times to produce Gla residues before it is metabolized for elimination (Figure 136-3).
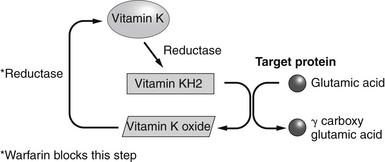
Figure 136-3 Vitamin K recycling and carboxylation reactions.
(From Bowen RA. Vitamin K. http://www.vivo.colostate.edu/hbooks/pathphys/misc_topics/vitamink.html. Accessed 5/29/12.)
Until now, the AI (adequate intake) for vitamin K has been defined as the amount needed to completely carboxylate prothrombin. With the discovery of new roles for various VKDs throughout the body, many researchers are now proposing redefining the AI at a level where all VKDs in the body are 100% carboxylated. A review by McCann and Ames points out that vitamin K affinity varies greatly for each type of VKD, which may influence the order in which VKDs are carboxylated. Most likely, this is done in an order of physiologic priority.29 For example, clotting may have the highest priority in utilizing most of the vitamin K ingested when intake is around or below 100 mcg/day. In this situation, most of the other VKDs in the body will tend to be inadequately carboxylated and so have poor functionality. Unfortunately, there are no tests to verify the carboxylation of all the known VKDs except for the three that will be discussed (PIVKA II, osteocalcin, and MGP). Important cofactors affecting the rate of carboxylation of VKDs are manganese and vitamin B6, specifically P5P (pyridoxal-5-phosphate). Deficiency of these cofactors may downregulate carboxylation, whereas supplementation with P5P was shown in vitro to upregulate it twofold.
Osteocalcin is a protein produced by osteoblasts (bone-building cells) that transports calcium inside the bone for fixating it in the hydroxyappatite structure, thus supporting bone mineralization. Vitamin K has been shown to stimulate osteoblasts to increase their production of osteocalcin and collagen type I, both important components of the bone structure. Increased levels of osteocalcin are able to better support bone remodeling and thus improve bone architecture, which translates into better bone elasticity and reduced risk of fracture.30–32
Osteodentin (tooth dentin) is responsible for tooth mineralization, similar to osteocalcin’s role in the bone.33 Note that the salivary gland concentrates a significant amount of vitamin K, which may have a role in supporting oral health. Vitamin K is known to affect certain bacteria by participating as a cofactor in their energy production (similar to coenzyme Q10 in animal mitochondria). If it is in fact proved that salivary glands secrete vitamin K, this would affect oral bacteria; one researcher has stated that excess vitamin K may exacerbate periodontal disease.34
Matrix Gla protein, or MGP, is found in many soft tissues, where it has at least one identified role, that of rejecting calcium deposition. Specifically, it is found in the skin and in the walls of arteries and veins, where it prevents the calcification of elastin fibers, thus reducing the risk of elasticity loss in these tissues. It is also found incorporated with underlying ground substance of the skin and cartilage (associated with chondrocytes), where it seems to play a role in the synthesis of glycosaminoglycans.35 MGPs have also been identified in testes and sperm; their role there is not clear, but vitamin K deficiency has been shown to reduce testosterone production and sperm motility. One study that looked at primary prostate cancer cells versus metastatic cells found that “loss of MGP expression may be associated with tumor progression and metastasis.”36
Note here the important roles of vitamins D and A in some of these VKDs:
• The active form of vitamin D (1,25[OH]D3) stimulates the synthesis of osteocalcin and MGP.37
• Vitamin A (retinoic acid) stimulates the synthesis of osteocalcin but inhibits that of MGP.38
Consequently vitamins K, D, and A work in concert and have interdependent actions. Thus, in order for vitamin K to perform its functions, the status of vitamins D and A must be optimized, so that VKDs are expressed adequately. It has also been established that the genetic effects of 1,25(OH)D3 are mediated by vitamin A through its nuclear receptor, which exert a permissive activation on the vitamin D nuclear receptor.39
GAS-6 protein (growth arrest-specific gene 6) is believed to play a role in platelet aggregation, cell growth, and apoptosis and has been shown to support the survival of cells in tissues such as arterial muscle, eye lens epithelium, brain, and possibly others. It is also involved in supporting adequate innate immunity (natural killer [NK] cells) and reducing the risk or severity of autoimmune cellular events.40
Modulation of Inflammation by Downregulation of Inflammatory Cytokines
Vitamin K may reduce inflammation by downregulating of IL-6 and PGE2 as follows:
• Metabolites of vitamin K, the 5- and 7-carbon carboxylic acid catabolites of vitamins K1 or K2 (MK-4 or MK-7), inhibit the release of IL-6. This was shown specifically for osteoblasts.41
• Vitamin K2 (MK-4) has been shown to reduce the production of PGE2 by direct inhibition of the COX-2 enzyme.42
These actions of vitamin K may reduce the activity of any inflammatory/autoimmune diseases that are exacerbated by PGE2 and IL-6.43 In osteoporosis, IL-6 and PGE2 have been shown to enhance bone resorption through activation of the RANKL receptor, which in turn upregulates osteoclast differentiation.44 This mechanism is considered essential to the effects observed from treatment with high doses of K2 (MK-4) in reducing and reversing bone loss. Vitamin K2 has also been shown to reduce the activity of rheumatoid arthritis by inhibiting the proliferation of the rheumatoid synovial cells.45 A correlation has been found between vitamin K status (plasma vitamin K1) and osteoarthritic disease activity in the hands and knees.46 In the Framingham study, plasma vitamin K1 was shown to inversely correlate with C-reactive protein (CRP), a marker of inflammation.
An elevated PGE2 should also be corrected by addressing the arachidonic acid/eicosapentaenoic acid (AA/EPA) ratio. This, in effect, modulates the substrates of the COX2 enzyme and would have an additional impact on PGE2 production when added to the effect of vitamin K2 (MK-4) of inhibiting COX2. One study states the effect of the AA/EPA ratio on another inflammatory intermediate as follows: “nuclear factor kB is activated by arachidonic acid but not by eicosapentaenoic acid.”47
Downregulation of Cell-Signaling Proteins (Produced Downstream of Mevalonate and HMG-CoA) Affecting Cell Differentiation and Apoptosis
Vitamin K2 (MK-4) is believed to have an inhibitory effect in pathways downstream of mevalonate, the same pathways where statins and bisphophonates are believed to inhibit key enzymes (HMG-CoA reductase and protein farnesyl transferase, respectively). However, the actions of K2 (MK-4) are not the same as those of pharmaceutical drugs, which have a direct enzyme inhibitory action. Instead, K2 (MK-4) seems to work through a feedback inhibition effect on the mevalonate pathway by “mimicking” one of its downstream metabolites, the molecule geranylgeranyl pyrophosphate.48,49 This mimicry occurs by means of the side chain of vitamin K2 (MK-4), which is the molecule geranylgeranyl. This may be why K2 (MK-4) has distinct effects compared with those of other forms of vitamins K2 or K1.
The inhibition of the mevalonate pathway has multiple effects on human physiology besides cholesterol inhibition since it also downregulates the synthesis of various geranylgeranylated proteins (rho, rab, rac) involved in cell proliferation, cell death, and survival, inflammation, and immune response.50 Consequently when vitamin K2 (MK-4) is supplied orally in large doses (many studies have used 45 mg and even 90 mg,51 which are in the supraphysiological range), it exerts a “mass action” characterized by some researchers as “pharmacologic” in nature.
Roles in Bone Health and Therapeutic Interventions for Osteoporosis
1. Vitamins K1 and K2 are cofactors for the activation (by carboxylation) of osteocalcin, which enables the proper deposition and binding of calcium in the bone matrix.
2. Osteoblasts’ production of osteocalcin and collagen type I is increased by vitamin K2 through modulation of the genetic expression of these proteins.52
3. Vitamin K2 reduces osteoblasts’ apoptosis (cell death)53 and stimulates other bone blastic proteins, such as osteoprotegerin and osteopontin.54
4. Vitamin K2 reduces osteoclasts’ production from bone marrow cells55 and induces osteoclasts’ apoptosis, which in effect reduces the total number of osteoclasts. These metabolic effects are achieved through vitamin K2’s ability to downregulate inflammation (IL-6, PGE2) and cell proliferation while increasing apoptosis (through the geranylated proteins produced on the mevalonate pathway).56 This would be beneficial only if the osteoclastic activity were excessively high.
5. Vitamin K2 may reduce the accelerated bone resorption induced by menopausal hormonal loss57 or corticosteroid treatment.58,59
Vitamin K Doses in the Physiologic Range
Some studies that tested interventions for bone health have used doses of vitamin K that can be considered physiologic—for example, 200, 500, and 1000 mcg of K1.31 The optimal physiologic range has not been completely defined for vitamin K1 and less is known about that of vitamin K2. The dose needed for complete bone osteocalcin activation is believed to be around 1000 mcg of K1, but some individuals may need 2000 mcg.60 This dose is 10 to 20 times higher than that needed for optimal clotting, which is in the range of 90 to 120 mcg.61 In this dosage range, vitamin K exerts its effects in the metabolic pathways, the way the human body evolved to utilize this nutrient. Owing to very low consumption of leafy greens or liver, most people rarely ingest more than 100 to 200 mcg of vitamin K1 and more than 50 mcg of vitamin K2.114 Vitamin K doses in the “normal” physiologic range would most likely be effective, as some studies have shown,62 for the prevention of osteoporosis or osteopenia.
Vitamin K Doses in the Supraphysiologic Range
Most of the studies using a very high daily dose of K2 (MK-4) (e.g., 45 mg) done in Japan with the drug version of K2 (MK-4), Glakay, have shown a significant effect on bone mineral density (BMD). The differences in BMD changes between the treatment and placebo groups for BMD were as follows: +1.1%, +5.2%, and +7.5% after 6, 12, and 24 months, respectively. Some studies also reported a reduced fracture rate (FR) by as much as 80%. Some studies have shown that vitamin K can reduce the FR even when BMD is not affected.63
However, in two recent studies conducted in Holland and the United States, where the investigators used the same K2 (MK-4) material from Japan (Glakay), there was no effect on BMD.64,65 At least the Dutch study found an increase in total bone mineral content as a result of this treatment as well as in bone strength (calculated value). Also puzzling is the fact that a Glakay 1996 postmarketing population survey done in Japan of 4000 people taking the same dosage of 45 mg/day of K2 (MK-4) showed no effect on overall FR (however, a subgroup that had at least five fractures at baseline did show a fracture reduction of about 40%).66 BMD was not assessed in this survey.
Only a few of the studies that used vitamin K1 (in daily doses of 200 and 1000 mcg) have seen a higher BMD in the treatment group over placebo. However, others that used daily doses of 500 mcg, 1 mg, 5 mg, and 10 mg have found no effect on BMD, even though the doses of 5 mg and 10 mg were 5 and 10 times higher than the upper physiologic dose of 1 mg. None of the vitamin K1 studies mentioned previously reported FR except the one using 5 mg, which showed an approximate 50% reduction despite no change in BMD.62
Interestingly, a few of these studies included multiple treatment groups in addition to placebo in an attempt to sort out the effect of vitamin K alone or vitamin D alone versus combination treatments that included vitamin K plus vitamin D or vitamin D plus calcium or all three together.67,68 The results from all these studies clearly showed that combining vitamin K with vitamin D had a stronger effect than either one alone and that combining vitamin K with vitamin D and calcium had even stronger effects. Only one study added magnesium and zinc to the treatment group (taking vitamin K1 = 1 mg, vitamin D = 320 IU, and calcium = 500 mg), and this is one of the only two studies using vitamin K1 that showed a slower age-related decline in BMD in the treatment group.69
1. Incomplete support and insufficient doses of the nutrients essential to the specific actions of vitamin K on bone (such as vitamin D, calcium, vitamin A, and vitamin B6) as well as other aspects of bone metabolism, such as magnesium, zinc, manganese, vitamin B6, and omega-3 fatty acids. These complementary nutrients have synergistic and additive effects to vitamin K’s actions, as discussed earlier under “Mechanisms of Action of Vitamins K1 and K2.”
2. The bioavailability of the supplements given in different studies may vary widely: (e.g., the solubility and absorption of vitamins D and K, and the absorption of minerals, especially calcium, the absorption rates of which vary greatly depending on its form).70
3. The common diagnostic technique to measure BMD used in studies of vitamin K is not as sensitive in detecting the specific actions of vitamin K on bone as are other types of evaluations of bone health and bone quality, such as BU (bone ultrasound test of the heel), BMC (total bone mineral content), BG (bone geometry or size of various bone components, including height changes), or BS (bone strength, calculated from BMD, BG, height, and weight). By the nature of the measurement, BMD is thought to be unable to “give the complete picture” of bone status because it cannot distinguish architectural aspects of the bone quality.71 These aspects of bone health influence its elasticity and resilience and are all important predictors of FR.
Vitamin K supplementation is believed to improve bone quality whether or not it shows effects on BMD.72 Bone quality may be best reflected by assessments of BU, BMC, BG, and BS; this has been done in a few studies in addition to the measurement of lumbar and spinal BMD.73,74 One interventional study with 45 mg of vitamin K2 (MK-4) has shown an increase in both BMC and BG despite no effect on BMD. The treatment group also maintained their bone strength (calculated from BMD and BG) as compared with the placebo group, which showed an expected age-related decline in bone strength. Consequently, this study showed that vitamin K supplementation might reduce FR even though it did not affect BMD.64
Researchers estimate that vitamin K status (as assessed by undercarboxylated Oc [ucOc] in plasma) may correlate better with BU and FR than BMD.63 Bone heel BU was found to have an accuracy and ability to discriminate osteoporotic patients similar to lumbar and spine BMD (by dual-emission x-ray absorptiometry, or DEXA), with potentially better prediction for FR. Consequently it may be useful to do a BU measurement (in addition to or instead of DEXA) in assessing the effects of vitamin K interventions in clinical practice. One study found that “ultrasound parameters were still significant independent predictors of vertebral fracture even after adjusting for BMD.”75 The BU test may give additional information to the BMD test, especially for patients who, for example, have increased their BMD after many years of bisphosphonate therapy (which reduces bone remodeling severely owing to its main mechanism of action of inducing osteoclast apoptosis).
Optimal Doses of Vitamins K1 and K2 for the Complete Activation of Osteocalcin
One study used escalating doses of vitamin K1 (250, 500, 1000, and 2000 mcg) and measured the increase in the percentage of plasma Oc that was completely carboxylated. The results showed that, for that particular population, an intake of about 1000 to 2000 mcg of vitamin K1 was sufficient and necessary to achieve close to complete carboxylation of plasma Oc, which means that it would be completely activated. Another study that used doses of 1mg of vitamin K1 in one group and 45 mg of K2 (MK-4) in another showed that both groups achieved close to complete carboxylation of Oc.65 However, it is not clear whether a dose of K2 (MK-4) lower than 45 mg could have achieved the same degree of carboxylation.
A study published in 2009 looked at the short-term effects (4 weeks) of a dose of 1500 mcg of K2 (MK-4) on the percentage of ucOc in plasma.76 The results showed a decrease in the percentage of ucOc from about 30% to 20%, which is still suboptimal. Another study showed that a dosage of 45 mg/day was sufficient to bring the ucOc down to about 4% (which may be close to the detection limits of current laboratory assessments).65
Effects of Average Levels of Vitamin K1 Derived from the Diet
As discussed, a few studies have observed an inverse correlation between normal vitamin K1 intake derived from the diet and FR and a direct correlation with BMD. The difference between dietary and supplemental vitamin K1 is that the subjects with a high dietary intake of vitamin K1 may have derived it from consuming a lot of green leafy vegetables—which in itself may improve bone health through its magnesium, calcium, potassium, and bicarbonate content—thus improving alkalinity. One important fact to consider is that average dietary vitamin K1 intakes are typically too low (slightly below 100 mcg in the United States and Great Britain to slightly above 200 mcg in Holland) to satisfy the need for completely carboxylating osteocalcin (which is believed to be in the vicinity of 1000 to 2000 mcg of K1) or other VKDs that may be involved in bone metabolism. The average vitamin D status in the general population is deficient, which would further impair bone health.77
The Synergy and Necessity of Combining Vitamins K and D
Vitamin D is known to enhance Oc expression. It was also demonstrated in vitro that the active form of vitamin D (1,25[OH]D3) enhances the effect of vitamin K2 on Oc.78 Vitamin K cannot realize its potential to carboxylate Oc if Oc is not adequately expressed in the first place owing to low vitamin D status.79
None of the studies employing vitamin K1 or K2 supplementation optimized the vitamin D status (as assessed by plasma 25[OH]D3) with sun exposure or vitamin D supplementation. Most studies used insufficient doses of vitamin D in the range of 200 to 1000 IU, whereas some used an analog of an active form of vitamin D: 1-alpha-hydroxycholecalciferol (which has drug status in Japan). Many commercial laboratories have raised the upper limit of the reference range to include the whole “normal physiologic range.” The upper limit of the new reference range of plasma 25(OH)D3 now corresponds to adequately sun-exposed individuals (the so called “lifeguard level”), which has effectively almost doubled the old upper limit of the reference range. The old limit was simply derived from a population that was not adequately exposed to sun.80
The studies that used slightly higher doses of vitamin D, such as 800 or 1000 IU, achieved some of the better results: (1) FR reduction of about 50% (with 5 mg K1 and 800 IU of D3)63 and (2) a BMD increase of 2.3% over baseline and a 7.35% increase over placebo when supplemented with 45 mg of K2 (MK-4), 1454 mg of calcium, and 1000 IU of vitamin D2. They showed that the higher the baseline levels of 25(OH)D3, the higher the rate of BMD increase was in the treatment group. Also, the lower the baseline levels of 25(OH)D3 were, the faster the BMD decline was in the untreated group.
The reason this study used D2 was stated by the authors as lack of availability of vitamin D3 in Japan at that time (2005). Vitamin D2 compared to vitamin D3 is similar but not as effective. In fact, the researchers believed that had they used D3, the results might have been stronger, and a recently published paper shows that vitamin D3 was 87% more effective in raising blood levels of vitamin D and also resulted in a two- to threefold increase in vitamin D storage as compared with D2.81
One animal study, published in 1994 and funded by the drug company producing Glakay (K2[MK-4])155, demonstrated that vitamin K supplementation had no effect on the bone density in the vitamin D deficient rat group, but showed an increase in bone density in the group supplemented with vitamin D, which also ended up with 50% higher plasma levels of 25(OH)D3. However, no study attempted to raise plasma levels of 25(OH)D3 adequately, and it may be possibly because the doses necessary to achieve this, such as 2000 to 5000 IU of vitamin D3 per day, are still considered above the commonly accepted UL (upper tolerable limit).
Two study authors actually state in their papers that they purposely did not design the vitamin K studies with added doses of vitamin D above 400 IU because vitamin D3 supplementation at the level of 800 IU was able to show a reduction in bone fractures on its own and confounded the effects of vitamin K.82 Unfortunately, owing to this reductionist study design, we have few studies investigating the full effects of synergistic combinations of nutrients at levels that occur in a natural and optimal human physiology and in evolutionary adequate diets with added sun exposure.
Why Use 45 mg K2 (MK-4) and Are There Any Potential Side Effects?
1. Oxidative stress, which may be enhanced because of high intermediate K3 metabolites formed from ingesting K2 (MK-4).
2. Coenzyme Q10 production or the immune response may be diminished because K2 (MK-4) inhibits the mevalonate pathway, similar to what was observed with statins, since they downregulate via the same pathway.
3. Unfavorable effects on bone may occur from excessive reduction of osteoclast cell numbers, because this may cause an excessive reduction in bone remodeling. In this respect, vitamin K2 (MK-4) acts like a bisphosphonate (BP), so one cannot rule out that, in the long term, similar side effects may be discovered for vitamin K2 (MK-4), as they have been for BP. However, unlike BP, K2 (MK-4) is likely to have a more positive effect on bone because it stimulates Oc production and its activation, thus enhancing the bone-building process, rather than only reducing the bone-resorbing activity, as BPs do.
How Does K2 (MK-4) Compare with Bisphosphonates and Does It Make Sense to Combine Them?
One Japanese study showed that combining K2 (MK-4) supplementation with BP treatment showed an additive and synergistic effect, probably because of their complementary actions, such as bone building support by vitamin K and not just osteoclast apoptosis by BPs.83,84 Another study showed that vitamin K2 (MK-4) improved the effect of the BP in reducing FR significantly (slightly more than 50%) but had only a modest effect in improving BMD. Overall, BPs seem to have a much stronger effect in increasing BMD than K2 (MK-4). However, BPs seem actually to produce an increase in certain types of FR after long-term use.85 Also, as discussed in Chapter 194, “Osteoporosis,” although bisphosphonates increase BMD, such bones are less remodeled and seem to be less elastic and more brittle and therefore, with time, tend to become more vulnerable to fracture.
What Is the Potential of K2 (MK-7) in Supporting Bone Health?
The amount of total vitamin K2 (mix of various lengths) in a Western diet (from a sample Dutch population) (which may contain fermented cheese, fermented milk, and processed meats) averages 29 mcg/day (in a range from 1 to 128), from which K2 (MK-7) represents an average of 0.4 mcg (in a range from 1 to 2.2) (Table 136-3). Vitamin K2 intake is much higher in the Asian diet owing to its high content of fermented vegetables and soy-based fermented foods; it ranges from 35 to 247 mcg/day, of which K2 (MK-7) can represent 50 to 100 mcg/day in those that consume natto.
K2 (MK-7) is considered a candidate for supplementation to improve bone health because studies have shown a positive correlation between the levels of natto intake (a fermented soy and rice food) and various markers of bone health, such as the degree of carboxylation of OC, BMD, and FR.86 However, the benefits of natto may not be attributable entirely to its vitamin K2 content, as it also contains soy isoflavones, which may have a significant effect on bones in menopausal women that do not take hormonal replacement. Soy foods also contains minerals, and other nutrients.
A study supplementing adolescents with 45 mcg of K2 (MK-7) reported a drop in undercarboxylated Oc from approximately 48% to 38%, clearly showing that the 45-mcg of dose of K2 (MK-7) was not high enough to support the complete carboxylation of Oc.87 Researchers chose this dose because it had enough of a safety profile to be proposed as a supplement for adolescents, as it is within the normal range of total dietary vitamin K2 in Holland. However, dietary K2 is a mix of various forms of vitamin K2, of which K2 (MK-7) may represent only a small percentage, depending on diet (high in Japan; low in Holland and the United States). This level of 45 mcg of a vitamin K2 mix from a Dutch diet was found to best correlate with reduced arterial calcification and reduced risk of cancer in previous epidemiologic studies (discussed under “Role in Cardiovascular Health and Therapeutic Interventions for Reversing Arterial Calcification”). There is an ongoing study using 180 mcg of K2 (MK-7) investigating its effect on bone and arterial health, with results due in 2011.88
A 6-week study showed that a dose of K2 (MK-7)—147 mcg—was able to carboxylate Oc to a larger extent than an equimolar dose of vitamin K1 (100 mcg).89 However, at the end of this study, the percentage of ucOc was 23%, which is still higher than optimal.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree