CHAPTER 31 Vascularized Fibular Grafting for Osteonecrosis of the Femoral Head
Indications
Contraindications
Surgical Technique
Overview
The procedure is performed with the patient under general anesthesia and with the adjunct of an epidural block, which remains in place for 24 to 48 hours postoperatively. The patient is placed in the lateral decubitus position and supported by a pegboard. The entire lower extremity to the level of the iliac crest proximally is prepared and draped. The leg is covered with an impervious stocking up to the mid thigh, over which a sterile tourniquet is placed just proximal to the knee; this is to be used during the fibular graft harvest (Figure 31-1). A Betadine-impregnated occlusive drape is used for both the hip and the leg. The operative procedure on the hip and the harvest of the fibular graft occur contemporaneously and, as such, require cooperation between the surgeons.
Fibular Graft Harvest
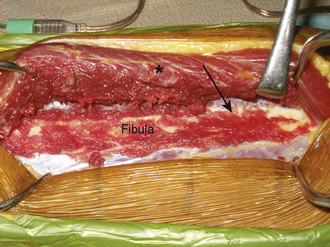
With the use of tourniquet control, a straight, lateral, 15-cm longitudinal incision is made coincident with the natural sulcus between the lateral and posterior compartments of the leg. The incision is begun at least 10 cm distal to the fibular head, and it ends at least 10 cm proximal to the lateral malleolus. The peroneal muscles are reflected in an extraperiosteal fashion off of the lateral aspect of the fibula, working from posterior to anterior and stopping when the anterior intermuscular septum is visualized (Figure 31-2).
Fibular Osteotomy
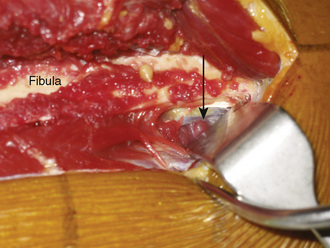
Directly beneath the distal aspect of the flexor hallucis longus muscle, the distal pedicle of the peroneal vessels is identified, and malleable retractors are passed between this pedicle and the fibula. Diligent care is critical during the placement of the retractors to ensure the protection of the pedicle during the osteotomy. After reconfirming that the planned osteotomy is at least 10 cm proximal to the distal tip of the fibula, an oscillating saw is used to cut the fibula. Irrigation during the osteotomy is vital to prevent thermal osteonecrosis. Next, the proximal pedicle is identified deep to the soleus muscle along the posterior aspect of the fibula (Figure 31-3). It is protected, and the proximal fibular osteotomy is performed in a manner similar to that of the distal osteotomy. The fibular cuts are made 15 cm apart to ensure an adequate pedicle length. It is important when performing the proximal osteotomy to identify and protect the superficial peroneal nerve, which is exposed proximally on the deep surface of the peroneus longus muscle.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree