CHAPTER 9 Supine Approach to Hip Arthroscopy
Surgical technique
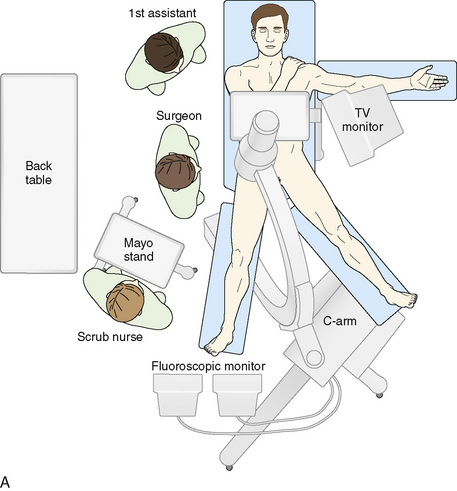
For the supine position technique, the patient is given a general anesthetic that provides muscle relaxation. Paralysis is recommended, because this allows less force to be used to distract the hip, with the purpose of reducing the risk of pudendal nerve injury from pressure between the pelvis and the perineal post of the traction table. The patient is placed supine on the fracture table with both feet secured to traction boots or mobile spars, depending on the specific table used. A well-padded perineal post is placed, and the patient is brought into position so that the post is firmly situated against the perineum and lateralized toward the operative hip, with care taken to protect the genitalia. The operative leg is positioned in 10 degrees of abduction, neutral flexion–extension, and neutral rotation. The nonoperative extremity is positioned in 45 degrees to 60 degrees of abduction, neutral flexion–extension, and neutral rotation to serve as countertraction for lateralization. Gentle traction is applied to the abducted nonoperative leg, which lateralizes the patient’s pelvis and results in the perineal post resting on the inner upper thigh of the operative extremity (Figure 9-1). This allows for the pressure of the perineal post to be diverted away from the perineum itself to minimize the risk of neuropraxia to the pudendal nerve as traction is applied to the operative leg. In addition—and quite important—this also helps to generate the appropriate vector of force for a uniform distraction both laterally and distally (Figure 9-2). Traction to the operative leg straight distally would be met with unnecessary resistance to overcome the inferior transverse acetabular ligament. Lateralization of the hip with the use of the post helps to pull the femoral head laterally and distally from the socket without having to overcome the ligament as a barrier to distal translation.
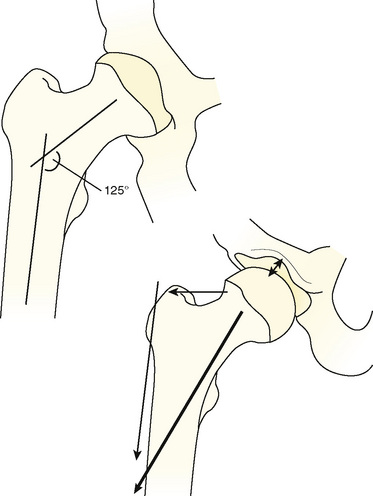
From Byrd JWT. The supine position. In: Byrd JWT ed. Operative hip arthroscopy. New York; Thieme Publishers; 1998: Figure 9.2, page 125.
After the patient has been positioned appropriately and slight traction has been applied to the nonoperative extremity, traction on the operative limb can be applied. This should be incremental, and it can be monitored with serial images from an image intensifier (i.e., C-arm). A tensiometer can also be used; however, the senior author has not found this to be useful. Jim Glick has shown that the risk of nerve injury as assessed by somatosensory evoked potentials is associated with the duration of traction rather than the amount of traction (Glick, personal communication). Thus, the absolute amount of traction is apparently not important. Some surgeons use the tensiometer to evaluate any changes in tension. We use the fluoroscopic image intensifier routinely; we bring the base of the machine in from the foot of the table in between the patient’s abducted legs, and we center the column over the operative hip (see Figure 9-1). Incremental traction is then applied until approximately 8 mm to 10 mm of femoroacetabular joint distraction is generated. The area of the proposed anterolateral portal is identified and marked; the area around this proposed portal site is prepared with Betadine solution; and a spinal needle is then used to enter the hip joint to verify the correct path of the anterolateral portal, to ease joint access, and to perform an air arthrogram to release negative intra-articular pressure. In a cadaver study, Dienst and colleagues demonstrated that positioning the hip in 20 degrees of flexion and performing an air arthrogram (i.e., disrupting the vacuum seal and distending the hip joint) reduced the amount of traction required to distract the joint for safe entry, thereby further reducing the risk of neuropraxia. The needle is placed from the intended anterolateral portal with the guidance of the fluoroscopic image intensifier (Figure 9-3). The needle needs to enter the central compartment to effectively reduce the intra-articular pressure. We have shown that placing the needle onto the femoral neck does not release the negative intra-articular pressure within the joint. Care is taken to keep the spinal needle close to the femoral head (to reduce the risk of injury to the labrum) and to keep the longer part of the tip away from the femoral head. When the suction seal is broken, the joint will open more widely. The needle position relative to the femoral head is evaluated before and after the seal is broken. If the needle moves proximally when the negative pressure is released, the labrum may have been violated by the needle. If the needle moves with the femoral head, the labrum has likely not been injured.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree