Use of the Laboratory in Diagnosing Rheumatic Disorders
Terry Shaneyfelt
Gustavo R. Heudebert
 |
Patient 1: An 80-year-old retired carpenter presents for evaluation of diffuse joint pain. He reports gradual onset and progression of pain in the right first metacarpophalangeal (MCP) joint and bilateral proximal interphalangeal (PIP) and distal interphalangeal (DIP) joints over the past 5 years. He also has pain in both knees. He has some stiffness in all the affected joints, which lasts approximately 15 to 30 minutes each morning. Pain is worse with activity. He denies any swelling, rashes, fevers, or other joint involvement. Physical examination of the hands reveals hard enlargement of the second through fourth DIP and PIP joints, and painful range of motion of the right first MCP joint. No synovitis is detected. Knee examination reveals crepitance with preserved range of motion and no joint effusion.
Patient 2: A 25-year-old female presents for evaluation of fatigue, myalgias, and intermittent hand pain. She reports that the pain tends to “move around” both the hands and is moderate in severity and can resolve within 24 hours. On further questioning, she reports an erythematous rash on her cheeks after working out in the sun a few weeks earlier, but it resolved and has not recurred. She also reports a short-lived episode of pleuritic chest pain a month earlier. Physical examination reveals mild pain with range of motion in several PIP joints and her left wrist. No effusions or deformities are seen. No pleural or cardiac rubs are heard on auscultation and no rashes are noted on skin examination.
As clinicians, we combine clinical skills with information from diagnostic tests to establish accurate diagnoses so that we may initiate appropriate treatment for our patients. In this chapter, we focus on probabilistic diagnostic reasoning in which pretest probability is informed by diagnostic testing resulting in posttest probabilities. We do not focus on the commonly used diagnostic method of pattern recognition. We recognize that both diagnostic methods are appropriate and complementary. Probabilistic diagnostic reasoning is useful especially for more challenging or less familiar clinical situations where pattern recognition fails.
The generation of a differential diagnosis relies on us, having both general medical knowledge and disease prevalence knowledge. Key features derived from the history, in conjunction with physical examination findings, serve to either increase or decrease the likelihood of each diagnosis under consideration in a process of hypothesis testing. In establishing hypotheses, it is important that we accurately assess the pretest probability of the diagnoses we are considering so that subsequent testing can help us to rule in or rule out those possibilities. Pretest probability is the chance or probability that the patient under consideration has the target disorder before any testing is carried
out. It can be determined in several ways. Validated clinical prediction rules are decision aids that combine elements of history, physical examination, and basic diagnostic or laboratory testing to accurately estimate pretest probability. Disease probability studies, in which representative samples of patients with certain symptoms (e.g., syncope) undergo extensive diagnostic work-ups and report the frequency of the underlying disorders that caused the patients’ illnesses, can provide very accurate estimates of pretest probability but are available for few disorders. Most commonly, and least accurate, clinicians use clinical intuition and experience to guess at the pretest probability. However, there are few well-validated clinical prediction rules in general as well as specifically in the area of rheumatologic disorders; as such it is of crucial importance to understand the interplay between results of diagnostic tests and the clinician intuition of the likelihood of the diagnosis for which the test is being ordered. Since pretest probability informs posttest probability, clinicians must begin with an accurate pretest probability. The consequences of inaccurate pretest probability assessment include poor selection of tests, poor interpretation of results, and ultimately diagnostic error.
out. It can be determined in several ways. Validated clinical prediction rules are decision aids that combine elements of history, physical examination, and basic diagnostic or laboratory testing to accurately estimate pretest probability. Disease probability studies, in which representative samples of patients with certain symptoms (e.g., syncope) undergo extensive diagnostic work-ups and report the frequency of the underlying disorders that caused the patients’ illnesses, can provide very accurate estimates of pretest probability but are available for few disorders. Most commonly, and least accurate, clinicians use clinical intuition and experience to guess at the pretest probability. However, there are few well-validated clinical prediction rules in general as well as specifically in the area of rheumatologic disorders; as such it is of crucial importance to understand the interplay between results of diagnostic tests and the clinician intuition of the likelihood of the diagnosis for which the test is being ordered. Since pretest probability informs posttest probability, clinicians must begin with an accurate pretest probability. The consequences of inaccurate pretest probability assessment include poor selection of tests, poor interpretation of results, and ultimately diagnostic error.
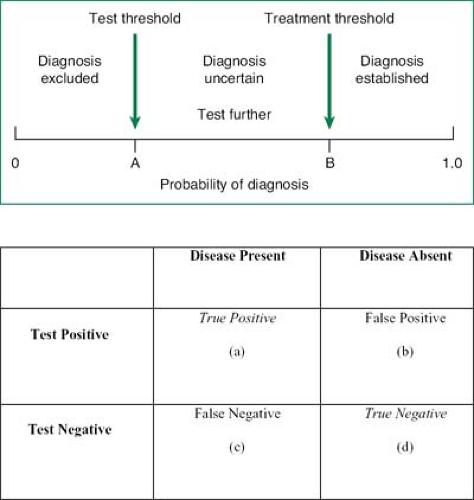
Once pretest probability is determined, clinicians must decide whether to initiate treatment or to perform further diagnostic testing. The treatment threshold is the threshold above which the probability of disease is so high that further testing is unnecessary and treatment can be initiated. The testing threshold is the threshold below which the probability of disease is so low that further testing is unnecessary and the diagnosis is considered excluded (Fig. 26.1). Diagnostic testing is only useful to inform intermediate probabilities between the testing and treatment thresholds. These thresholds vary on the basis of the disease prognosis under consideration, the properties of the diagnostic tests, and the nature of the treatment. The safer the testing strategy, the more serious the condition if left undiagnosed, and the more effective and safe the available treatment, the lower the test threshold. For the treatment threshold, the more benign the prognosis of the illness and the higher the morbidity associated with therapy, the higher we would place the threshold. For example, our testing threshold would be low if a clinician suspects deep venous thrombosis as the duplex ultrasonography is a test that is both safe and easily available; on the other hand, our treatment threshold would be relatively high as anticoagulation, especially when considering short- and long-term courses of therapy, is potentially dangerous for a patient.
The first patient likely has osteoarthritis. No validated clinical prediction rules for the diagnosis of osteoarthritis of the knee or hand exist, nor any disease probability study has been conducted. Clinical intuition would place the pretest probability of osteoarthritis at around 85% to 90%. For most clinicians, the treatment threshold to initiate acetaminophen in this patient is fairly low and could be initiated without further testing (as we are fairly confident he has osteoarthritis and the consequences of moderate doses of acetaminophen are low). The alternative would be to order hand films, which we suspect would be done to rule out other conditions (i.e., rheumatoid arthritis), although the clinical scenario would make this diagnosis highly unlikely (<5%). Of interest, a relatively nondiagnostic radiologic study likely would not stop most clinicians
to initiate acetaminophen therapy; in other words, ordering a hand film had no bearing on our treatment decision but perhaps made us feel better regarding other diagnostic possibilities. The difficult question then becomes if the cost or inconvenience of the hand film is worth excluding highly unlikely diagnoses.
to initiate acetaminophen therapy; in other words, ordering a hand film had no bearing on our treatment decision but perhaps made us feel better regarding other diagnostic possibilities. The difficult question then becomes if the cost or inconvenience of the hand film is worth excluding highly unlikely diagnoses.
Patient 2, on the other hand, likely has systemic lupus erythematosus (SLE). No validated clinical prediction rules to determine the pretest probability of SLE have been published. One population-based screening study (1) of SLE reported a prevalence of 200 cases per 100,000 women (18 to 65 years of age) in England, whereas another review estimated the overall U.S. prevalence of definite SLE plus incomplete SLE (disease meeting only some diagnostic requirements for SLE) to be 40 to 50 cases per 100,000 persons (2). Population prevalence studies such as these two can give misleading estimates of pretest probability because they have the wrong denominator, namely both healthy and diseased persons, both men and women. What we want to know is what is the proportion of all young women presenting with arthritis, malar rash, and possible pleuritis, similar to our second patient, who are ultimately diagnosed with SLE. Again we have to rely on clinical intuition and estimate this patient’s pretest probability to be >50%. The treatment threshold to initiate immunosuppressive therapy in this case would be fairly high (i.e., the clinician would want to be certain of or rule in the diagnosis of SLE). The consequences of undiagnosed SLE are great, making the testing threshold fairly low. Thus further testing for SLE is indicated in patient 2 prior to initiating disease-specific therapy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree