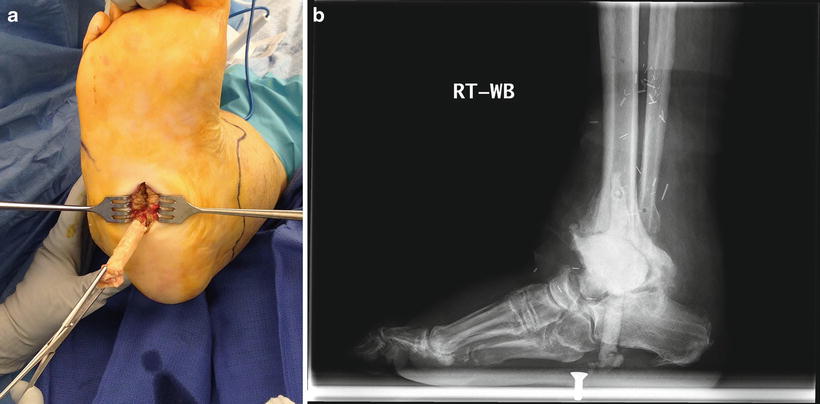
Fig. 11.1
ABLC spacer inserted into deadspace after debridement of diabetic foot osteomyelitis
Several case series have reported success using ABLC as an adjunct to partial foot amputation or as part of a staged limb salvage protocol [43–45]. Krause et al. [43] used absorbable ABLC beads in 46 diabetic patients undergoing a single-staged transmetatarsal amputation and reported a significantly lower complication rate in comparison to 16 transmetatarsal amputation patients that were not treated with ABLC beads.
Schade and Roukis [38] analyzed 29 patients with diabetic foot infections that were treated with parenteral antibiotics, aggressive surgical debridement, and PMMA beads impregnated with 500 mg of gentamicin and 2.4 g of tobramycin. Patients underwent repeat debridement and bead exchange approximately 3 days post implantation as needed before definitive closure. Cultures taken at the time of bead removal revealed positive bacterial growth in only five patients. They theorized that the reason for this persistent infection was inadequate debridement at the index surgery and suggested that the role of ABLC appeared to be maintenance of an aseptic environment instead of complete infection eradication.
Some patients have local and/or systemic factors that make them poor candidates for additional revision surgery [46]. A permanent ABLC spacer (Fig. 11.2) may provide adequate stability for these patients in lieu of amputation or long-term systemic antibiotics. Melamed and Peled [47] reported a 91 % success rate in treating 23 cases of forefoot DFO with debridement and placement of an ABLC spacer as an alternative to toe or partial ray amputation. They hypothesized that the ABLC would resolve the deep infection and temporarily or permanently fill the void, maintaining structural stability at the area created by extensive debridement. The spacer was retained permanently in ten patients and removed with conversion to successful resection arthroplasty/pseudoarthrosis in six patients and fusion in five patients, respectively. The authors concluded that when left as a permanent spacer at the metatarsal head location, the spacer appears to participate in weightbearing and stability and may provide a viable alternative to amputation or additional reconstruction.


Fig. 11.2
(a) Regenerate bone growth surrounding and stabilizing the ABLC spacer, (b) Preservation of the hallux and no re-ulceration in patient with a permanently retained ABLC spacer at the first MTP joint
Trauma
Given the foot and ankle’s thin soft tissue envelope and limited vascular perfusion, lower extremity trauma often results in open wounds. In addition, open fractures may result in segmental bone defects with or without OM. These cases require sequential debridement to eradicate infection before wound closure, fracture repair, or reconstruction. Adjunctively, ABLC has been used for decades to control infection and manage dead space resulting from traumatic injury.
As first described by Masquelet et al. [40], defects requiring delayed bone grafting can be temporarily filled with an ABLC spacer for 4–5 weeks to decrease the risk of infection, allow healing of soft tissues and induce the formation of a vascularized membrane around the ABLC. This induced-membrane optimizes the local environment for delayed bone grafting and prevents fibrous ingrowth and graft reabsorption [48]. While this technique is commonly used for segmental bone loss from high-energy trauma [42], few cases specific to the foot and ankle have been published.
Huffman et al. [49] used the Masquelet technique to treat a patient with complex open fractures and bone loss at the medial column secondary to a gunshot. Two weeks following initial debridement and ORIF, the patient underwent repeat debridement, insertion of an ABLC spacer into the medical column defect and wound closure with a microsurgical free flap. They performed the second stage of the Masquelet technique several months later. This involved removing the ABLC, filling the encapsulated defect (5 cm × 3 cm) with autograft and fixating the fusion site with a locking plate. At the 1-year follow-up, graft incorporation and fusion were noted and the patient was able to ambulate with a custom-molded shoe.
Malizos et al. [50] retrospectively reviewed the outcomes of 84 consecutive patients that were treated for posttraumatic or postoperative OM at the foot or ankle. All patients were treated with a limited course of parenteral antibiotics and a surgical protocol of aggressive debridement and an ABLC spacer or bead pouch (4 g of vancomycin per 40 g of PMMA cement power and 3 g of fucidic acid), which was placed into the open wound and wrapped and sealed with an impermeable adhesive membrane. External fixation was used in cases involving segmental defects at the distal tibia. A “second-look” debridement and ABLC exchange was performed 48–72 h after the initial debridement and repeated until the wound was clean. Once the wound was deemed clean, they performed bony reconstruction using autograft (Ten patients), distraction osteogenesis (Eight patients), or joint fusion (11 patients) and soft tissue closure following the reconstructive ladder.
They achieved limb salvage and infection control without an amputation in 69/84 (82 %) cases. They performed a primary below-knee amputation (five patients) or ray amputation (six patients) for Cierny-Mader type B and C hosts with a non-salvageable infection. A mean of three operative procedures per patient were performed. Host-type B and C patients required significantly more operative procedures than host-type A patients (P = 0.02). Additionally, the risk of complications was significantly greater for type-B and -C hosts versus type-A (p < 0.001). They concluded that a staged surgical management protocol combining radical debridement, local antibiotic delivery, and short-term systemic antibiotics efficiently controlled infection and achieved functional limb salvage in the majority of patients.
Postoperative Infection/Septic Joint
Postoperative bone or joint infection is a challenging and potentially limb-threatening complication of reconstructive surgery. Treatment goals include eradication of the infection and restoration of a painless functional limb through revision of initial surgery or salvage procedure [51]. Treatment options for surgical revision and limb salvage include: debridement with retention of hardware and long-term antibiotic suppression, debridement with removal of all hardware, insertion of a temporary ABLC spacer with a one- or two- stage implant exchange or arthrodesis procedure, or amputation [46, 50–52] (Fig. 11.3).


Fig. 11.3
(a) Postoperative dehiscence and infection of Achilles tendon and calcaneous, (b) Retained suture anchors in posterior calcaneous with osteomyelitis, (c) ABLC spacer used to treat osteomyelitis and fill void after removal of anchors and debridement of infected bone
While the literature and outcomes data specific to the foot and ankle are limited [53], multiple joint replacement centers have reported good clinical and functional results using a two-stage procedure for the treatment of hip and knee infections [54–57]. The preferred, two-stage revision starts with removal of the infected implant, joint debridement, irrigation, and placement of an ABLC in the implant site. The second stage typically follows a few (2–4) months later and consists of ABLC removal and replanting of a revision prosthetic or an arthrodesis-type procedure [2].
Not all patients are good candidates for additional surgical revision.
Ferrao et al. [51] used an ABLC spacer as definitive management for postoperative ankle infections following total ankle replacement (n = 6). They used ankle arthrodesis (n = 3) for patients who, following insertion of the cement spacer, either did not desire further surgery or were medically unfit for further surgery. Two patients eventually underwent BKA for wound complication and pain as a result of the ABLC loosening. All patients with a retained spacer were able to ambulate and perform basic activities with minimal discomfort.
Management Protocol/Surgical Algorithm (Chart 1)
Foot and ankle osteomyelitis is an often complex and limb-threatening condition that requires a team of specialists (infectious disease, vascular surgery, etc.) to optimize healing potential and maximize the patient’s chance of limb salvage. A systematic management protocol is imperative to maximize systemic and local host factors, eradicate infection, manage dead space, and optimize lower extremity mechanics and function.
Debridement
The first and most critical step in our management protocol is aggressive and wide resection of all infected, necrotic, and nonviable bone and soft tissue until only normal, well-perfused tissue remains. Necrotic or dead bone has a discolored, avascular appearance and soft consistency. Bone should be debrided back to a hard consistency with punctate bleeding on the cortex (Haversian) and normal-looking marrow in cancellous (sinusoidal) bone (paprika sign). A sagittal saw is useful for serially sawing off bone slices until exposed surfaces bleed in uniform and the transition from necrotic infected bone to viable bone is observed [46]. Atraumatic surgical technique should be used throughout debridement to avoid damaging adjacent healthy tissues [58].
We prefer to perform debridement without an inflated tourniquet so that the quality of bleeding at the debrided wound edges and bone margins can be continually assessed. When a tourniquet is utilized for hemostasis during debridement, it is important to deflate the tourniquet before performing a final wound assessment [58]. Inadequate debridement can result from concerns about how to close and reconstruct the resultant defect, highlighting the importance of access to a multidisciplinary team of surgeons. The removal of all osteomyelitic bone takes precedence over the preservation of normal, bony architecture [46].
Multiple studies demonstrate that the quality of debridement plays a vital role to eradicate and prevent the recurrence of infection [38, 59]. Simpson et al. [59] found a significantly lower infection recurrence rate in patients with osteomyelitis who underwent wide resection—5 mm beyond the normal margin of infected bone—compared to those that underwent a less aggressive, marginal debridement. After debridement, the wound is irrigated with a pulsed lavage system, using 3–6 L of normal saline, taking care to avoid unwanted irritation to the healthy tissues.
Hardware Removal
Hardware and implants are carefully evaluated during the initial debridement and removed when any suspicion for loosening or deep infection exist. Internal hardware is a nidus for infection and early biofilm formation. The surest way to eliminate biofilms in orthopaedic infection is to remove the affected device that harbors the biofilm completely [60].
Cultures and Biopsy
Multiple, deep soft tissue and bone specimens should be sent for microbiologic culture (aerobic, anaerobic, fungal, acid-fast) to obtain antibiotic sensitivities and confirm findings consistent with osteomyelitis through histologic analysis. These samples should be taken from representative tissue at the zone of infection before and after debridement and irrigation. Additionally, it is important to obtain cultures of both the debrided osteomyelitic bone and the normal bone proximal to the area of debridement. Analysis of this normal bone or “clean margin” and the post-debridement wound cultures are used to guide antibiotic therapy, confirm the irradiation of infection, and determine whether further debridement or wound closure is appropriate [46, 58]. When possible, the initiation of empiric, broad-spectrum antibiotics should be delayed until these deep cultures are obtained [46].
Chart 1 Staged surgical treatment of foot and ankle osteomyelitis with antibiotic-loaded cement
Antibiotic-Loaded Cement Implantation
High-dose ABLC (>1 g antibiotic per batch of cement) is effective and indicated for treating infection, but the only commercially available ABLC products are low dose (≤1 g of antibiotic per batch of cement) and are indicated for prophylactic with revision joint replacements. Because the FDA has not approved a reformulated high-dose ABLC (2–8 g antibiotic per 40 g of bone cement), the formation and use of high-dose ABLC requires hand mixing by surgeons, resulting in a wide variation of dosages and types of antibiotics used to treat infection [13, 61]. Although antibiotics dosage is not yet standardized for high-dose ALBC, at least 3.6 g of tobramycin and 1 g of vancomycin per 40 g package of bone cement has been recommended for effective elution levels [13].
Technique
The ABLC is created using sterile technique on the back table according to the manufacturer’s instructions. Methylmethacrylate can be dry mixed with the appropriate antibiotic powder—we prefer approximately 2 g aminoglycoside and/or 2 g vancomycin per 40 g of cement prepared, depending on the patient’s infection history and risk factors. The liquid monomer is then added and the combination is mixed until the cement is semirigid. Alternatively, Hanssen [13] recommends first mixing the PMMA monomer and powder together to form the liquid cement before adding the antibiotic power, in order to make mixing easier when using high volumes of antibiotic.
Beads vs. Spacer
Once the ABLC is semirigid, it is molded into beads or a spacer. Beads are often used to treat osteomyelitis in small areas or when structural stability is not as important (partial foot amputation). Spacers are custom-molded to fit the size and shape of the defect (block, sphere, intramedullary rod) providing improved stability, maintenance of musculoskeletal alignment, and soft tissue tension, which is important when planning a revision [62] (Fig. 11.4).


Fig. 11.4
Antibiotic-loaded cement spacer inserted into the defect resulting from debridement of osteomyelitis. Note that first MTP joint alignment is maintained
Spacers are inserted into the defect when still slightly moldable. Care is taken to ensure that the defect is not overstuffed and no prominences are felt to prevent excess pressure to the skin and wound-healing problems (Fig. 11.5). Although the majority of the hardening process should take place on the back table, saline irrigation can be used while the cement hardens to prevent exothermic damage at the adjacent skin [38].


Fig. 11.5
Antibiotic-loaded cement spacer at the fifth TMT joint. A larger, more prominent spacer could cause wound-healing problems to the adjacent skin
Beads measuring 5–8 mm in diameter can be formed and strung on a strong monofilament suture or wire when the ABLC is moderately viscous. They should be allowed to cure completely (15–20 min) before insertion into the defect. The bead pouch technique [63] or negative pressure wound therapy can be used to cover the wound when the overlying soft tissue defect is too large for closure.
External Fixation
Temporary external fixation may be applied when additional stability is needed in cases of large segmental defects to maintain anatomic alignment. Monorails (Fig. 11.6) are typically used to span the forefoot and midfoot while static ring fixation is used to stabilize the ankle and hind foot.


Fig. 11.6
Monorail external fixation used to stabilize and maintain position of the first MTP joint and ABLC spacer
Soft Tissue Closure
Wound closure is performed when infection eradication is noted with clinical findings, laboratory data as well as post-debridement culture and biopsy results. When confirmed clean at take-back evaluation and debridement, wound closure is performed following irrigation using a double instrument setup to avoid recontamination [58]. When possible, the soft tissues are closed primarily over the spacer or beads using an interrupted technique with monofilament.
The reconstructive ladder is used to guide wound closure when large- or difficult-to-close defects are present. Although several modifications of the concept have been described, most descriptions start with direct closure, followed by skin graft, local flap, and finally free flap. In addition, negative pressure wound therapy (Fig. 11.7) can be used as an adjunct to any method of reconstruction [64]. Before wound closure, drain insertion should be considered to prevent dehiscence [61].


Fig. 11.7
Negative pressure wound therapy used for wound management in a patient with an ABLC spacer implanted to fill the void left after removal of the infected cuboid
Spacer Removal or Exchange
Patients typically return to surgery 24–72 h after the initial debridement for a repeat debridement and ABLC exchange, or ABLC removal and wound closure based on the clinical response to therapy and surgical goals. Serial debridement and spacer exchange every few days may be repeated until all infection is eradicated [61] (Fig. 11.8).