Type I
Open fracture, wound <1 cm in length and clean
Type II
Open fracture, wound >1 cm in length without extensive soft tissue damage, flaps, avulsions
Type III
Open segmental fracture; open fracture with extensive soft tissue damage; traumatic amputation (including gunshot injuries, open fractures caused by farm injuries, fractures requiring vascular repair)
A
Adequate periosteal coverage of the fractured bone despite the extensive soft tissue laceration or damage; high-energy trauma regardless of wound size
B
Extensive soft tissue loss with periosteal stripping and bone exposure, usually associated with massive contamination
C
Arterial injury requiring repair, irrespective of degree of soft tissue injury
Initial Workup
Initial evaluation and management of a trauma patient is similar regardless of the mechanism of injury. A detailed history is necessary with special considerations given to various factors such as time elapsed since the injury, mechanism of injury, environment where the injury occurred, and any initial treatments that have been performed. These variables have an impact on treatment decisions and can play a role in the potential for osteomyelitis. Specifically, the type of injury and environmental factors are useful for determining appropriate initial antibiotic coverage (Table 13.2). Tetanus status should be established with puncture wounds and open fractures. Recommended tetanus prophylaxis is dependent upon previous immunization history as described in Table 13.3 [12–14]. A detailed lower extremity physical examination is performed to evaluate soft tissue viability, neurovascular status, tendon function, and extent of open wounds. Radiographs are necessary to evaluate for retained foreign bodies and to identify any fractures. MRI, ultrasound, or CT scans are adjunctive modalities that may be needed to assist in further assessing damage and identifying any foreign objects. Initial laboratory testing for infection is optional depending on the time lapsed since injury which includes complete blood count (CBC) with differential, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP). Inflammatory marker labs are useful to follow the progress of therapy if there is concern for infection.
Table 13.2
Injury presentations and primary bacterial concerns
Injury type | Bacteria concern | Antibiotic options |
|---|---|---|
Lawn mower/chain saw injuries (farm/soil environment) | Pseudomonas spp. | Ciprofloxacin |
Levofloxacin | ||
Aminoglycosides | ||
Anaerobic (Clostridium spp.) | Penicillins | |
Amoxicillin/clavulanic acid | ||
Piperacillin/tazobactam | ||
Boating injuries (water environment) | Vibrio spp., Aeromonas hydrophila, Mycobacterium marinum | Tetracyclines |
Acute presentation puncture wound Consider broad spectrum choices for heavily contaminated wounds and diabetics | Gram positive: Staphylococcus aureus, Alpha hemolytic Streptococcus, Staphylococcus epidermidis | PO Cephalexin Amoxicillin/clavulanic acid Trimethoprim/sulfamethoxazole Clindamycin/ciprofloxacin |
Gram negative: E. coli, Klebsiella spp., Proteus spp. | IV Cefazolin Ampicillin/sulbactam Piperacillin/tazobactam Clindamycin Ciprofloxacin | |
Chronic presentation puncture wound Consider osteomyelitis, especially when through rubber-soled shoe | Pseudomonas spp. | Ciprofloxacin |
Levofloxacin | ||
Aminoglycosides | ||
Piperacillin/tazobactam | ||
Gustilo–Anderson Type I | Gram positive | Cephalosporins |
Piperacillin/tazobactam | ||
Aminoglycosides | ||
Clindamycin (PCN alternative) | ||
Gustilo–Anderson Type II | Gram positive > gram negative | CefazolinPiperacillin/tazobactam |
Gustilo–Anderson Type III | Gram negative > gram positive | Cefazolin or piperacillin/tazobactam, + Gentamicin/tobramycin, + Penicillin with severe contamination |
Initial Irrigation and Debridement for Open Trauma
Prompt and thorough irrigation and debridement of open traumatic injuries is a simple and effective approach for infection prevention. Local, regional, or general anesthesia may be necessary, and early determination should be made in the acute care setting regarding the need for surgical treatment in the operating room (OR). Open fractures are considered a surgical emergency, and the care teams should be mindful to reduce the time elapsed between injury and OR management. Historically, debridement of an open fracture was recommended within 6 h of the injury. Recent literature describes timely management is important; however, a larger emphasis is placed on taking into account the grade of the open fracture [15–19]. A recent study by Hull evaluated a series of 364 patients with open fractures and confirmed that higher grade Gustilo–Anderson fractures (Table 13.1) are more likely to develop a deep infection than lower grade fractures. Furthermore, a delay in treatment has a greater effect on these higher grade fractures and those that are grossly contaminated [18]. Thus, heightened awareness of the time to the OR is necessary in the higher grade and grossly contaminated injuries.
Prompt irrigation and debridement allows initial removal of debris or foreign objects and aids in reduction of the total bacterial load [5]. Secondary and staged irrigation and debridement is often indicated to further remove devitalized soft tissue and residual debris. Devitalized soft tissue reduces the effectiveness of the host immune system, thus attempts are made to remove any necrotic or devitalized tissue from the traumatized wound [4, 20]. The viability of skin and soft tissue is determined by color and bleeding, whereas muscle should be inspected for contractility in addition to color and bleeding. Irrigation solution is frequently based on surgeon preference, but adding povidone-iodine solution or antibiotics to normal saline or lactated ringers solution may not add value and perhaps has undesirable side effects [21, 22]. Detergent solutions have been shown to be effective at removing bacteria and dirt from bone [21, 22]. It is our preference to utilize saline alone, with the principle of copious irrigation for removal of bacteria and organic contaminants. Each traumatic wound or open fracture may require a varying amount of irrigation depending on the extent of injury and degree of contamination. Data is lacking to validate the exact volume of fluid that should be utilized for irrigation. Historically, 3 L is recommended for type I fractures, 6 L for type II, and 9 L for type III fractures [23]. Primary wound closure may be performed under conditions of prompt and appropriate antibiotic treatment, thorough debridement with healthy appearance of local tissues post debridement, and a good host immune system [20, 24–28]. Primary closure may prevent secondary contamination; however, the surgeon should not rush to close a wound if it does not appear ready. Inadequate debridement, inadequate antibiotics, and premature primary closure can increase the risk of complications. Early closure in patients with continued wound contamination with dirt, feces, and nonviable tissue can increase the risk of infection with Clostridium. The second stage procedure is planned 2–3 days later allowing secondary irrigation and debridement with hopeful partial or complete closure. The surgeon should not hesitate to perform staged procedures. Ideally, soft tissue coverage is performed within 3 days as a delay in closure beyond 7–10 days increases the risk of infection [29, 30]. Fracture management may be performed acutely or delayed depending on the fracture pattern and condition of the soft tissues. External fixation is useful for temporary stabilization in an unstable fracture when there is concern regarding the soft tissue envelope. If primary closure cannot be achieved, alternative coverage options such as negative pressure wound therapy (NPWT) may be valuable in patients with extensive loss of soft tissue followed by staged skin grafting at a later date. Case examples with treatment protocols are presented below regarding management of puncture wounds, open fractures, and crush injuries associated with industrial, recreational, and lawn mower injuries with the intent to avoid poor outcomes associated with posttraumatic osteomyelitis.
Puncture Wounds
Puncture wounds represent unique traumatic injuries as the wound is small, but there is potential for heavy contamination, internal injury, and retained foreign bodies. Secondary osteomyelitis can develop acutely due to direct inoculation of bacteria into bone or in a delayed manner due to contiguous spread of infection from local abscess formation. Pedal puncture wounds are common injuries that account for 7 % of lower extremity trauma emergency department visits [31]. The majority of puncture wounds heal without complications, but a delay in medical treatment may lead to problems including cellulitis, abscess formation, septic arthritis, and osteomyelitis. The location of the injury, type of footwear worn at the time of injury, and time elapsed before initial treatment will influence the incidence of infection development and osteomyelitis. The Patzaki classification system for puncture wounds divides the foot into three zones: zone 1 extends from the metatarsal neck to the toes, zone 2 is from the metatarsal neck to the distal calcaneus, and zone 3 includes the calcaneus [1]. The risk of osteomyelitis associated with plantar puncture wounds has been described as 0.1–2 %, with a greater prevalence in forefoot injuries (zone 1) through athletic shoes [8]. The distance between the soft tissue and bone is narrow in this weight bearing portion of the foot, and it is common for puncture wounds in this location to cause direct inoculation to a bone or joint depending on the length, rigidity, and sharpness of the penetrating object. Pedal puncture wounds are particularly concerning in the diabetic population since neuropathic patients frequently have a delay in treatment which commonly results in increased morbidity associated with puncture wounds [32]. Diabetic patients are five times more likely to have multiple operations and 46 times more likely to have lower extremity amputations after puncture wounds [33].
Imaging for Puncture Wounds
Imaging is valuable for foreign body evaluation in the presence of a puncture wound. Standard radiographs are useful for metal objects, large wooden objects that cast a shadow, and glass (Fig. 13.1). Foreign bodies with low radiopacity that are located in muscle tissue, or between bone and muscle tissue, can be difficult to visualize with standard radiographs or CT and are better seen on ultrasound imaging [34]. Thus, ultrasound can be useful to identify radiolucent objects such as plastic or wood and can identify the size and depth of the foreign object as well [35, 36] (Fig. 13.2a). An ultrasound technician can place a skin marker at the approximate location of the object for ease of foreign body removal which is particularly useful in lake presentation injuries when the wound is no longer visible. The amount of information obtained from an ultrasound however remains highly dependent on the skill of the user. An MRI is an alternative imaging option if there is a suspicion for foreign body despite negative radiographs or with late presentation puncture wound injuries with concern for abscess formation or osteomyelitis. It is not uncommon for a chronic and infected plantar puncture wound to develop an abscess that can track dorsally or plantarly along the tendon sheaths, in which case, an MRI is helpful for preoperative planning (Fig. 13.2b).

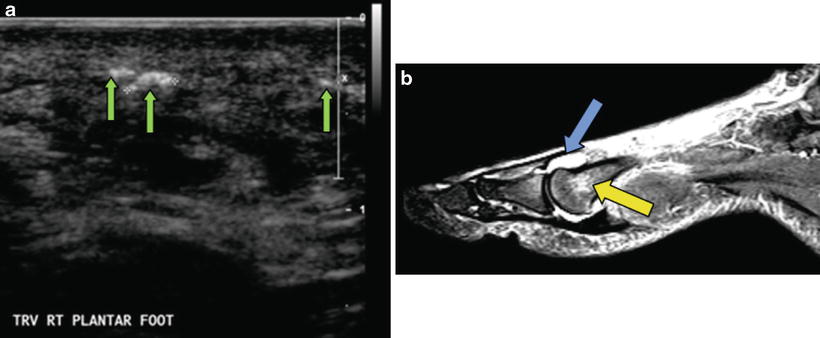

Fig. 13.1
X-ray evaluation for retained foreign body. Standard X-rays are the go-to imaging modality for puncture wounds. (a) Modern digital imaging is effective at identifying most fragments of glass regardless of lead content. (b) Identification of a foreign body on X-ray is the most useful tool for intraoperative guidance since the surgeon is able to directly view the X-ray during attempted removal. X-rays also provide baseline assessment of bone integrity for future comparison should infection develop
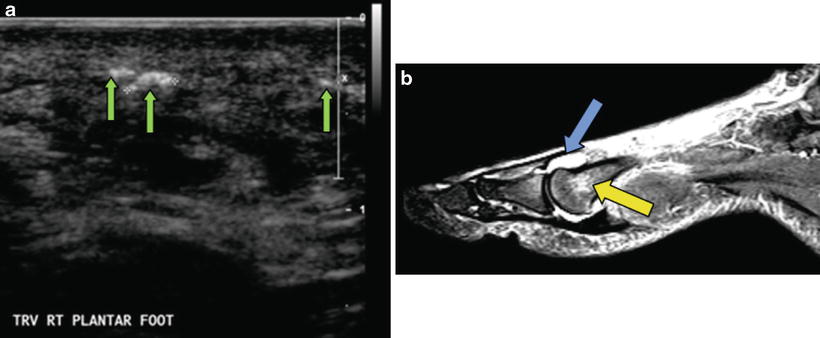
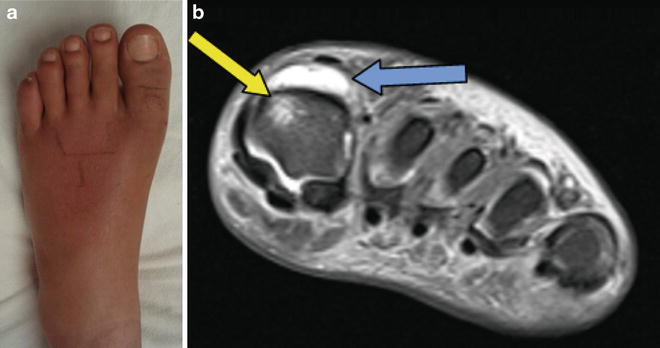
Fig. 13.2
Advanced imaging for puncture wounds and foreign bodies. Diagnostic ultrasound is useful to identify radiolucent foreign bodies or local abscess, although small shards of glass or wood may not be visible. (a) Ultrasound images may not be as useful to the surgeon although skin marking over the identified foreign body is quite beneficial for incision planning. (b) MRI imaging is used in cases of small foreign bodies, potential abscess formation, or joint sepsis associated with puncture wound injuries. Joint effusion is indicated by the blue arrow, and bone marrow edema is identified by the yellow arrow
Antibiotic Considerations for Puncture Wounds
Acute presentation of minor or superficial puncture wounds without clinical signs of contamination may not require antibiotics. However, puncture wounds with a delayed presentation, contamination, necrotic tissue, or known infection require antibiotic therapy. This is initiated after thorough irrigation, debridement, and culture. Staphylococcus aureus is the most common organism involved in soft tissue infections following acute puncture wounds. Empiric treatment with a first-generation cephalosporin is the drug of choice in acute puncture wounds without concern for other environmental factors. Pseudomonas is frequently found in soil, water, skin flora, and rubber-soled shoes. Thus, penetrating injuries that occur through rubber-soled tennis shoes require coverage for Pseudomonas [35]. In wounds that occur in brackish water, consideration for coverage of Aeromonas hydrophila and Mycobacterium marinum should be considered [37, 38] (Table 13.2). In delayed presentation puncture wounds or when there is a concern for development of underlying osteomyelitis, Pseudomonas coverage is important. Pseudomonas is the most common organism associated with puncture wound related osteomyelitis [35, 39]. If osteomyelitis occurs following a puncture wound, management follows basic principles including a combined medical and surgical approach with 4–6 weeks of antibiotics after bone biopsy and adequate debridement.
Initial Debridement of Puncture Wounds and Foreign Body Removal at Acute Presentation
Many acute presentation puncture wounds can be treated in an office setting or emergency department with a minor incision and drainage procedure. An attempt is made to remove any retained foreign body if present since this will act as a nidus for infection and frequently results in pain while walking. Inspection of the wound is needed to determine the depth as a deeper wound is more likely to involve tendon, bone, and joint structures. In younger children that cannot tolerate a local injection, procedural sedation is an option if available otherwise a traditional OR procedure should be considered.
The approach to removal of the foreign body depends on the depth within the soft tissue. A visible splinter or shard of glass can be easily removed in the office with or without a local block. The author’s preferred technique is to use the sharp tip of a 1.5 in. long 18 gauge needle to peel away the skin surrounding the foreign body. The needle acts as a tiny scalpel which minimizes unwanted injury. Loupe magnification is helpful for improved visualization.
Deeper foreign bodies typically require an incision below the dermis which also serves to drain any infection. A small (less than 1 cm) transverse plantar foot incision will typically heal within 7–14 days even without sutures; therefore, sutures are generally not needed. A local infiltrative block is utilized for anesthesia, and standard skin prep is performed. A technique that we have found beneficial is to first utilize a 1–3 mm dermal curette to inspect the deep wound in a methodical manor. The curette acts as a blunt probe and allows for initial inspection with both tactile and audible sensation. One should have a clear understanding of the location of the foreign body as demonstrated by radiographs or ultrasound prior to probing. Care is taken to avoid pushing the object deeper or into a new location. If the foreign body is located with the curette, a small hemostat is placed into the wound for retrieval. If needed and available, a fluoroscan can be useful to assist with location of the foreign object (Fig. 13.3). After removal of the foreign object, the wound is irrigated and culture swabs are obtained from the deep wound if appropriate. Depending on the size, depth, and observed cleanliness of the wound, a decision is made regarding primary closure, packing the wound, or to simply bandage and allow healing by secondary intention. Acute presentation with timely debridement and removal of the foreign body typically allows primary closure without subsequent development of infection.
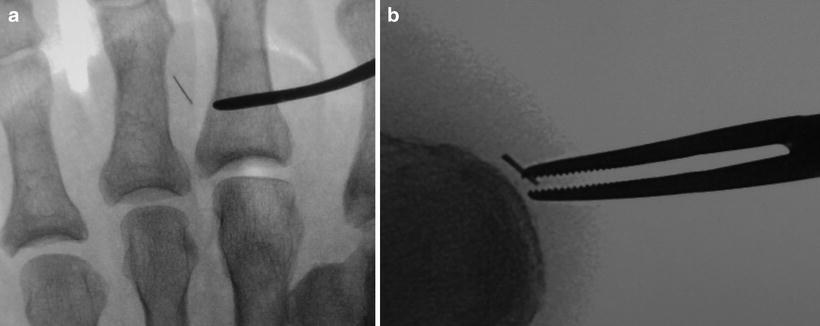
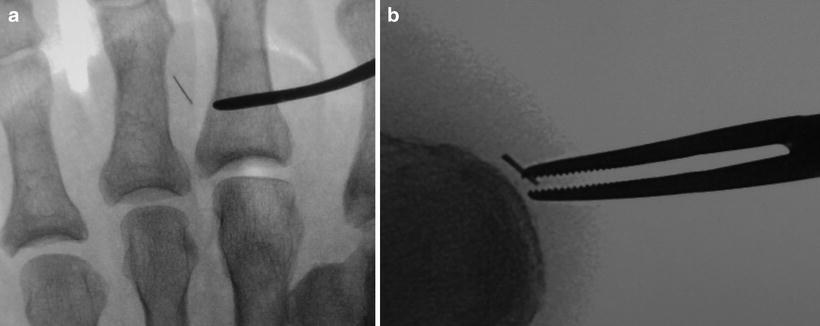
Fig. 13.3
Fluoroscopy-assisted foreign body removal. (a) A curette or freer can be utilized as a blunt probe for foreign body location using fluoroscopy. Care is taken to avoid pushing the object deeper or into a new location. (b) A small hemostat can be placed into the wound for extraction under fluoroscopic guidance
Surgical Treatment of Complex Puncture Wounds
Puncture wounds that require surgical treatment include failed retrieval with initial minor procedure, deep foreign bodies or deep penetrating wounds, foreign bodies near vital structures, delayed presentation puncture wounds, significant contamination, and concern for abscess or infection. Diabetes-related foot infections associated with puncture wounds and foreign bodies can be limb threatening and often present as surgical emergencies. Intraoperative fluoroscopy is typically beneficial to locate the object. Incision considerations involve the desire for adequate exposure and avoidance of incisions on the weight bearing surface, although achieving both goals is frequently not possible. Partial foot amputation may be necessary, and consideration should be given to flap closure options when planning incisions.
Two cases are presented to highlight surgical management protocols for complex puncture wounds. Case 1 is a patient with a retained foreign body and joint sepsis following a dorsal puncture wound from a nail gun (Figs. 13.4 and 13.5). Case 2 involves a delayed presentation puncture wound with abscess formation and significant soft tissue loss (Figs. 13.6, 13.7, 13.8, and 13.9). Removal of the foreign object is performed first if possible although exploration may be required for deep objects. Inspection for abscess, necrotic tissue, and bone exposure assists in determining the extent of surgery, need for staged surgery, closure options, and postoperative antibiotics. If an abscess is tracking in a direction away from the initial incision, one may consider a counter incision to aid in drainage. Intraoperative cultures are obtained after irrigation. The decision to close the wound primarily is based on the intraoperative appearance of the wound. If the nidus of infection is removed, no purulence was encountered, and remaining tissues are healthy in appearance, primary closure can be performed [26]. If an abscess or cellulitis is present, a staged approach to surgery is often best. The surgeon should not hesitate to perform repeat incision and drainage procedures approximately every 3 days until the infection is under control at which point the wound can be closed. If significant tissue debridement was necessary, the surgeon may decide for wound closure by secondary intention. NPWT with delayed skin graft closure is an option under these conditions. Antibiotic management is based on intraoperative appearance of the wound, likelihood of bone involvement, inflammatory marker labs, and culture results.