Chapter 14 Upper Limb Orthotic Devices
This chapter provides a guide for prescribing and the basic principles for using upper limb orthotic devices, commonly known as splints or braces. The word orthosis (derived from the Greek orthos, meaning to correct or make straight) encompasses the full spectrum of devices currently fabricated by therapists and orthotists.16 As defined by the International Standards Organization of the International Society for Prosthetics and Orthotics, an orthosis is any externally applied device used to modify structural and functional characteristics of the neuromuscular skeletal system.30 Orthosis—or alternatively, orthotic device—is the preferred term.21 The terms splint and brace are less preferred because they imply mere immobilization and do not suggest either improved function or restoration of mobility. However, these terms remain common, and in this chapter we use the terms orthotic device and splint interchangeably.
Principles and Indications
Classification
We use many different terms to describe upper limb orthotic devices. We call them by the joint they cover, the function they provide (e.g., immobilization), or the condition they treat. Some are named by their appearance (e.g., banjo or sugar tong), and still others bear the name of the person who designed them (e.g., Kleinert).28
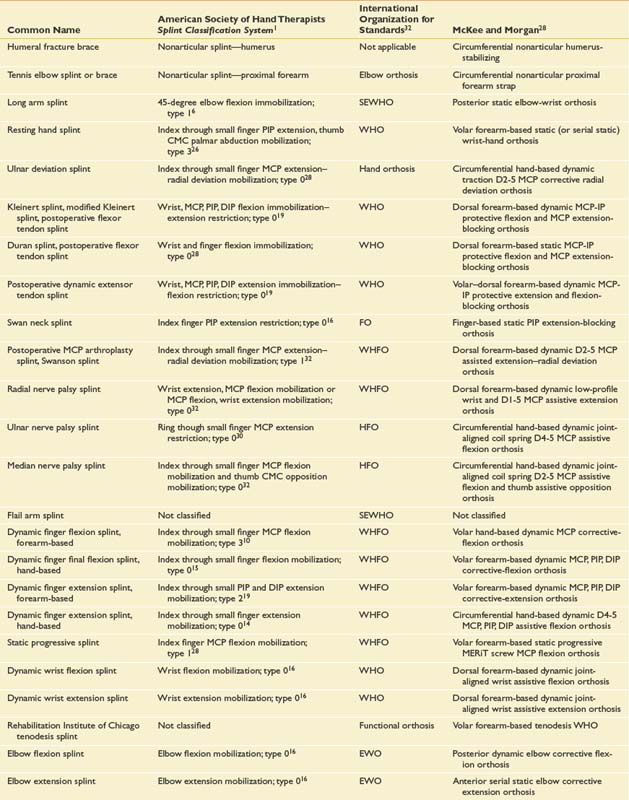
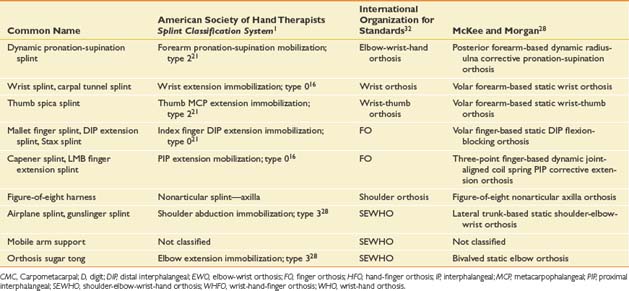
Most splints are known by their common names (Table 14-1)—names that have evolved over time. But such names are not fully informative, are not systematic, and are not even universally accepted. This lack of a universally accepted terminology often presents a communication barrier between the physician and other health professionals. Consequently, more systematic naming systems have been developed that classify orthotic devices according to anatomic region or to purpose and function. Table 14-1 compares the common names of several orthotic devices with those in three other naming systems.
The simplest naming system is that developed by the International Organization for Standards. It reports the anatomic region the orthotic device encompasses. A wrist-hand orthosis, for example, is called a WHO.32 This system, however, fails to define the purpose or function of the orthosis.
In 1991 the American Society of Hand Therapists (ASHT) published the ASHT Splint Classification System.1 This system provides standard nomenclature for splints based on function. It classifies splints by characteristics (e.g., articular or nonarticular) and location of the body part covered. A humeral fracture brace, for example, is identified as a nonarticular splint—humerus. It also identifies the direction of the force applied, and whether the splint is for mobilization, immobilization, or restriction. In this system a long arm splint (Figure 14-1) is characterized as a 45-degree elbow flexion immobilization. The problem with the system is that one splint design can provide many different functions.10
Biomechanical and Anatomic Considerations
Design Categories
Orthotic devices can be classified by the support (or forces provided) to improve motion or function. The categories of splint design are listed below.34
Nonarticular
The nonarticular splint provides support to a body part without crossing any joints, and protects a bone or body part. For example, a humeral fracture splint provides circumferential support to the arm during fracture healing. Other examples are a sugar tong splint to immobilize a proximal radius fracture, or a gel shell splint (Figure 14-3) to exert pressure over a healing scar to prevent hypertrophic scarring.
Static
The static splint provides static support to hold a joint or joints stationary. For example, a volar wrist splint for acute carpal tunnel syndrome reduces motion and rests injured tissues (Figure 14-4). Static splints can be used to protect healing structures (Figure 14-5), to decrease or prevent deformity, and to reduce tone in spastic muscles.
Static Motion-Blocking
The static motion-blocking splint permits motion in one direction but blocks motion in another. For example, a swan neck splint (Figures 14-6 and 14-7) is designed to allow flexion but block hyperextension of the PIP joint. (See the section on rheumatoid arthritis.)
Static Progressive
The static progressive splint is the one most commonly used for regaining joint motion. Unlike the serial static splint, the orthosis is not remolded to increase joint motion. These splints differ from serial splints in that they use nonelastic components such as static lines, hinges, screws, and turnbuckles to place a force on a joint to induce progressive change. The MERiT static progressive component3 (available commercially) decreases the static line length as it is turned, thereby increasing the range of joint motion (Figure 14-8).
Dynamic
The dynamic splint provides an elastic force to help regain joint motion. An example of such an orthosis is a finger extension splint, which uses a spring coil or wire tension assist to increase extension in a PIP joint with a mild contracture (Figure 14-9).
Dynamic Motion-Blocking
The dynamic motion-blocking splint allows certain motions but blocks others. It uses a passive, elastic line of pull in the desired direction, but permits active motion in the opposite direction. An example is a Kleinert postoperative splint for flexor tendon repairs (Figure 14-10). It passively pulls the finger into flexion with an elastic thread or rubber band. It allows active digital extension, while parts of the splint block full extension of the MCP joint and the wrist.
Dynamic Traction
The dynamic traction splint offers traction to a joint while allowing controlled motion. An example is a splint for an intraarticular fracture. This a hand-based PIP extension splint with an outrigger (Figure 14-11), which gives constant longitudinal traction while the joint is gently flexed and extended.
Tenodesis
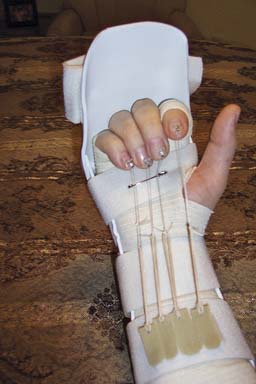
The tenodesis splint facilitates function in a hand that has lost motion because of nervous system injury. An example is the Rehabilitation Institute of Chicago tenodesis splint (Figures 14-12 and 14-13), which assists the patient with a C6 level of spinal cord injury to achieve a functional pinch. Active extension of the wrist produces controlled passive flexion of the fingers against a static thumb post through a tenodesis action.
Continuous Passive Motion Orthoses
Continuous passive motion orthoses are electrically powered devices that mechanically move joints through a desired range of motion. This keeps the joints supple and maintains articular, ligamentous, and tendinous structure mobility during the healing phases after injury or surgery.
Diagnostic Categories and Splint Examples
There are many common clinical conditions for which orthotic intervention is appropriate. This section gives a brief overview of the features of specific diagnoses, followed by the type of splints commonly indicated for each diagnosis. This is not an all-inclusive list, and the reader is referred to comprehensive overviews of upper limb orthotic devices in splinting texts and other references.∗
Musculoskeletal Conditions
Tendonitis, Tenosynovitis, and Enthesopathy
Tendonitis (inflammation of the tendon), tenosynovitis (inflammation of the tendon sheaths), and enthesopathy (inflammation at a muscle or tendon origin or insertion) can all result from excessive repetitive movement or external stressors. The upper limb tendons most commonly involved are the wrist extensors or the abductor pollicis longus and extensor pollicis brevis muscles of the thumb, commonly called de Quervain’s stenosing tenosynovitis. The goal of splints for these conditions is to immobilize the affected structures in order to facilitate healing and decrease inflammation. The thumb spica splint, forearm-based, immobilizes the wrist, the carpometacarpal (CMC) joint, and the MCP joint of the thumb. The IP joint of the thumb does not need fixation because the affected tendons do not move this joint (Figure 14-14).

FIGURE 14-14 Forearm-based thumb spica splint used for de Quervain’s stenosing tenosynovitis.
(Courtesy Jeanne Riggs, OTR/L, CHT.)
Lateral epicondylitis is a more common enthesopathy of the upper limb.34 It can be treated by a tennis elbow orthosis (Figure 14-15). This is a forearm band that changes the lever arm against which the wrist extensors pull. In essence, it puts the origin of the extensor muscles at rest and decreases the microtrauma from overuse. This orthotic device is placed approximately two fingerbreadths distal to the lateral epicondyle, and is a firm strap against which the extensors press against when contracting. A similar brace is used for medial epicondylitis (also known as golfer’s elbow). (See Chapter 38.)
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree