
A Congenital anomalies Limb deficiencies (yellow arrow) and Poland anomaly (absence of the sternal head of the pectoralis – red arrow) are caused by a failure of vascular ingrowth during early development.
The hand forms by about the 8th week [B] and reaches about a third of its adult size at birth [C]. Upper limb growth occurs most rapidly in the proximal humeral and distal forearm epiphyses [D].
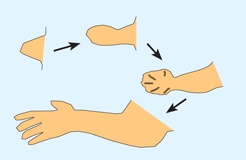
B Hand development The hand first as a bud at 3 weeks with progressive development and finally apoptosis or a dissolution of the interdigital webs to form fingers by about the 8th week.
Redrawn from Arey (1980).

C Hand growth The hand is about 5 mm when completely formed at the 8th fetal week, and about a third of its adult size at birth.
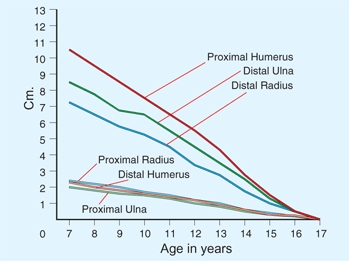
D Growth rates for upper limb The majority of growth of the upper limbs occurs from physes about the wrist and shoulder compared to the elbow. From Pritchett (1988).
During the seventh gestational week, the upper limb flexes at the shoulder and elbow and rotates around a longitudinal axis and accounts for the cutaneous nerve distribution [A]. Cutaneous nerve distribution in the hand arises from C6, C7, and C8.
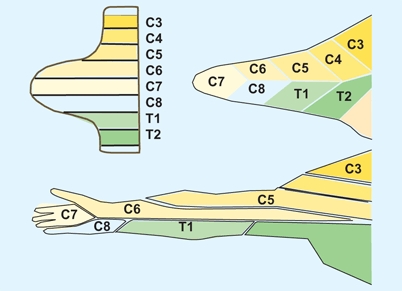
A Cutaneous nerve distribution The upper limb development clarifies the origin of the distribution of the segmental distribution of the upper limb.
Redrawn from Moore (1982).
During infancy, hand function progresses in an orderly fashion [B]. Bimanual function becomes refined during the second year. Both fine and gross motor skills improve with age. The function of each upper limb is more independent than that of the lower limbs. Thus, a short arm causes less functional difficulty than a short leg.
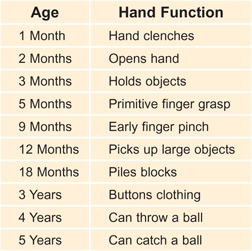
B Hand function by age Hand function becomes progressively more skilled with advancing age.
Optimum hand function is achieved by the dominant hand possessing both strength and the ability to manipulate small objects. The nondominant hand should grasp and release effectively. Function ideally requires intact sensation, tactile surfaces free of scars, motor strength, and a good range of motion of the wrist and fingers.
Evaluation
The physical examination should follow the standard sequence of inspection, palpation, range of motion evaluation, and a careful neurological examination. Imaging should start with conventional radiographs.
Screening Examination
First perform a screening examination of the child, as hand problems are commonly part of a syndrome or association. Examine the whole child [C] to avoid missing other problems that may be important in establishing the diagnosis, as well as other problems that may require treatment. This examination is often best performed with the child on the parent’s lap.
C Screening examination Examine whole child before focusing on the hand problem.
The Infant may be developmentally delayed but without any obvious deformities. Examine the head and trunk and look for associations that might involve the spine, heart, and kidneys. Also screen the lower limbs, as hand and foot problems may occur in the same syndrome or association.
Associations
Certain deformities of the upper extremity are often associated with specific syndromes [D, E, and F]. Examples include nail dysplasia in nail–patella syndrome and the various conditions associated with radial and ulnar deficiencies and syndactyly. Carefully examine the whole child. Look for dysmorphic features, and shortness of stature, and assess the child’s general health. Inquire about medical problems in the family. Certain findings indicate the need for additional studies. For example, the finding of torticollis is an indication for a radiograph of the pelvis to rule out hip dysplasia. The finding of radial dysplasia is an indication for a hematologic, cardiac, renal, and spine evaluation. Check for a sacral dimple.
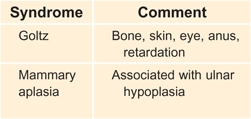
D Syndromes associated with ulnar defects These syndromes should be considered if an ulnar defect is present.
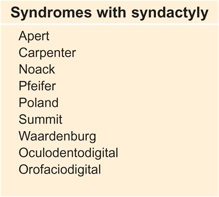
E Syndromes associated with syndactyly
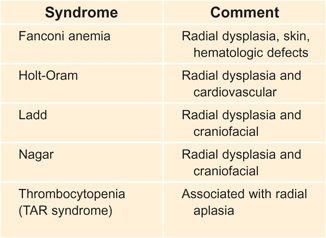
F Syndromes associated with radial defects These syndromes should be considered if radial defects are present.
Upper Limb
Head and neck
Observe the head and neck for abnormalities and asymmetry. The head is normally held in a vertical position by the vestibular and ocular righting mechanisms. Head tilt is common in “wryneck,” or torticollis. Describe the deformity in terms of the three planes, flexion-extension, lateral head tilt, and rotation. Observe the shape of the head. Plagiocephaly is common in torticollis and includes a flattening of the malar prominence and a lowering of the position of the eye and ear on the involved side. The ipsilateral occiput is flattened.
Limbs
Start with observation of the relationship of the neck and limbs. Note any asymmetry [A]. Observe differences in spontaneous movement. Loss of movement may be due to true paralysis from a nerve injury or more likely from pseudoparalysis due to trauma or infection. The infant with a clavicular fracture or septic arthritis of the shoulder or elbow will avoid active arm movement.


A Upper limb length inequality This girl’s right arm is shortened due to a cyst of the proximal humerus. Her function is normal.
Observe the carrying angle, the alignment of the arm and forearm as viewed with the child in the anatomic position. The carrying angle is normally 0°–10° of valgus. A varus carrying angle causes the so-called gun stock deformity, which is usually due to a malunited supracondylar fracture [B]. An increase in carrying angle is seen in Turner syndrome.
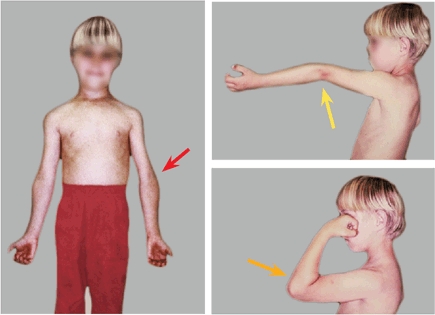
B Cubitus varus This child has a malunion following a supracondylar fracture. In the anatomic position, the child has a cubitus varus deformity (red arrow). Hyperextension deformity (yellow arrow) and limited elbow flexion (orange arrow) are also present.
Look for asymmetry or masses and note any finger or nail abnormalities [C]. Nail dysplasia is seen in the nail–patella syndrome. Other syndromes have characteristic finger deformities such as the “hitchhiker’s” thumb in diastrophic dysplasia.

C Nail-patella syndrome Nail dysplasia is seen in the nail-patella syndrome.
Palpation
Palpation is most important if the child complains of pain. Exact localization of the point of maximum tenderness is very important in establishing the cause of pain. This is most feasible about the elbow, wrist [D], and hand, where the bone and joints are subcutaneous.

D Localize tenderness Correlate tenderness with anatomic structures.
Range of Motion
Describe the motion of the neck in three directions. The normal child is able to flex the chin to the chest. Lateral head tilt should allow the ear to touch the shoulder. Normal head rotation allows about 90° of motion to the right and left. Assess forearm rotation with the elbow flexed to a right angle. Supination and pronation are each about 90° in the normal child.
Joint Laxity
The upper limb is readily examined to assess joint laxity. Assess the elbow, wrist, and fingers for the ability to hyperextend [E].

E Joint laxity Joint laxity is commonly assessed in the upper limb.
Pain
Pain is usually due to trauma , infection, or neoplasm. Pain is often manifest by pseudoparalysis in the infant and young child. Localization of the site of tenderness is very helpful in narrowing the diagnostic possibilities and in deciding what should be studied radiographically. Sometimes a bone scan is necessary to localize the problem.
Hand Examination
Observation
Observe the resting position of the hand as well as how the hand and fingers move. This is often best done from a distance to avoid frightening the child. Observe the position of the fingers. The resting position is altered by tendon lacerations or contractures.
Sensation
Assess sensation by observing the texture for trophic changes, the presence of sweat, and the use of the hand. Ask for the parents’ opinion about hand sensation. Parents usually know. In the older child, differentiating coins by feel alone may be useful.
Motor function
Observe the child playing with a toy to assess the use of the hand. Observe how the dominant and nondominant hands are used. Be aware that bimanual hand function develops after an infant acquires sitting balance.
Pain
A number of conditions that are unique to the hand and wrist may be the source of pain [A]. Among these are nonunion of the radial styloid, unrecognized fractures or idiopathic avascular necrosis of the scaphoid, and overuse syndromes. Most gymnasts experience wrist pain due to overuse. Gymnasts most at risk are older children who are new to the sport and participate many hours per week.
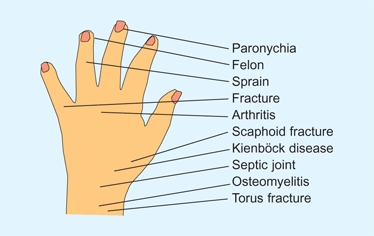
A Hand and wrist pain by location Often the diagnosis is suggested by the location of the tenderness or swelling.
Management Principles
Because the hand is used in expression and is always visible, appearance is an especially important consideration in management.
Descriptions
Describe conditions by using the anatomic terms rather than words such as clubhand or lobster claw deformity.
Parents
Be aware of parents’ feelings, especially if the child has a congenital or traumatic problem. Parents typically go through a series of stages in the grieving process that include first denial, then anger (which may be directed toward managing physicians), and then distress.
Healing
Because the skin of infants is prone to hypertrophic scar formation [B], be very careful about placement of surgical incisions, especially on the palmar aspect of the digits and in the web spaces.

B Hypertrophic scar Friction burns in a toddler. Note the thickness of the scars. Reconstruction will require full-thickness skin grafts.
Surgeon
Hand surgery in the infant or child is difficult due to the small size of the hand, the lack of cooperation of the patient, and the complexity of the problem. Seldom is there a need for the procedure to be done as an emergency, and because the best results are possible with the first attempt at repair, referral to a surgeon with special training and experience in managing hand problems in infants and children is best for the child.
Timing of Management
General guidelines have been established for optimum timing of various treatments.
Operative procedures
are performed in general categories [C]. This timing is a rough guide. Individualize each procedure.
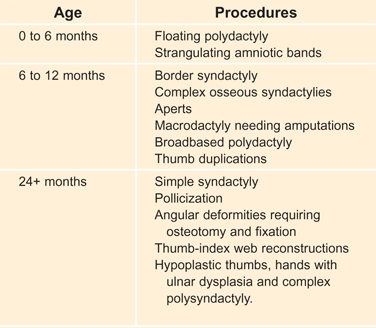
C Timing of procedures This table provides some generalizations for timing of operative procedures. Each indication should be individualized.
Management methods
Apply treatment types to specific age groups. Some general guidelines are useful [A, next page].
Maturity
Consider the capacity of the child to cooperate with treatment and rehabilitation. Surgical dressings should protect the operated area from the child. Delay complex procedures requiring cooperation during rehabilitation until later.
Splinting
Splinting is a primary or adjective treatment method used for hand problems [B]. Many different types of splints have been developed for use on fingers, hands, wrists, and elbows as both static and dynamic splints. Most are made of plastic by therapists with a specific objective in mind.
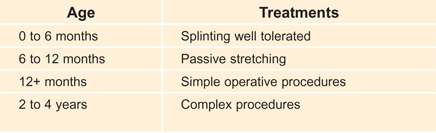
A Timing of management Treatment is best tailored to the age of the infant or child.
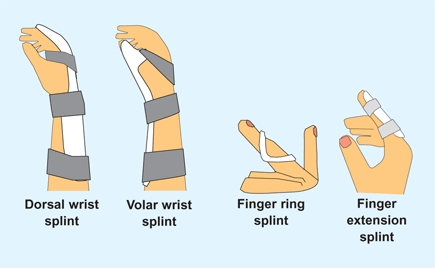
B Splints Many different types of splints are used for the hand. These are some examples.
Dressing
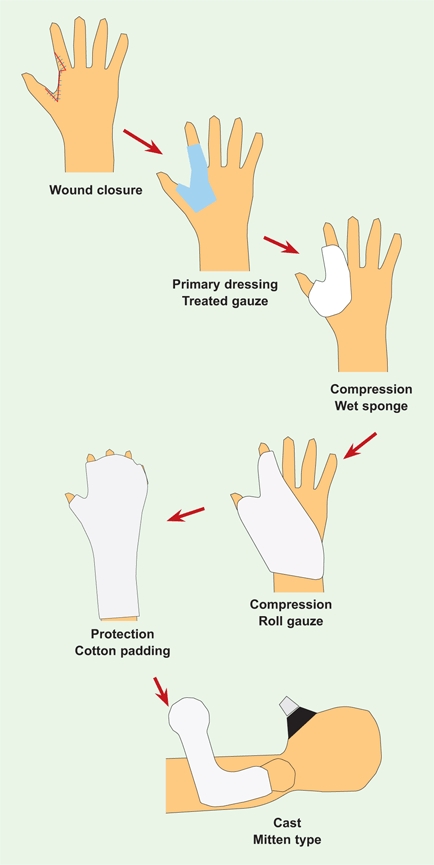
For most wounds, the following plan is appropriate [C]. If a tourniquet has been used, leave it inflated for the initial dressing application.
C Dressing sequence Dressings following surgery or injuries should be carefully applied.
Wound closure
Use 6-0 plain gut dyed blue with a marking pencil to make it visible and to make suture removal unnecessary. Use absorbable sutures.
Primary dressing
Place a single layer of fine mesh gauze treated with petroleum jelly to prevent sticking directly on the wound. Over this, apply a saline-soaked dressing sponge to direct drainage from the wound.
Compression
Apply gentle compressive dressing to secure the primary dressing, contoured and positioned not to restrict circulation. Apply the first layer of fluffed gauze between the digits, being careful to avoid excessive pressure. Then secure the gauze with roller gauze in 2- or 3-inch widths. This provides gentle compression, fits the hand well, and should hold the hand in a position with slight wrist extension and thumb abduction.
Padding
Next, place cotton cast padding to protect the skin and bony prominences and to facilitate cast removal. A skin adhesive will help to maintain the padding in position.
Deflate the tourniquet and assess circulation to each digit. Elevate the hand for a few minutes during the post-tourniquet hyperemia phase before apply the cast.
Rigid outer dressing
Apply a plaster or fiberglass cast that extends above the flexed elbow. This secures the dressing and prevents exploration and intrusion by the child and parents. Start the application with the elbow flexed slightly more than 90°.
In infants and young children, pad the digits and place a cast that becomes a mitten. This mitten prevents toys and food from entering the cast and further protects the wound and secures the dressing.
Sling
Apply a sling made from 2-inch tubular stockinette placed around the neck and chest to hold the arm at the side.
Upper Limb Deficiencies
Upper limb deficiencies may be due to malformations [A] or disruptions, such as amniotic bands, from trauma, or as a result from resections of malignant tumors. Limb deficiencies are most common in the lower limb and in boys [B].

A Complete “phocomelia” This child has bilateral radial dysplasia due to the proximal form of TAR syndrome.
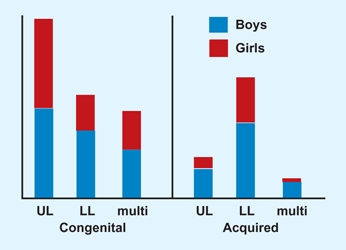
B Distribution of pediatric amputees Distribution for girls (red) and boys (blue) for UL (upper limb), LL (lower limb), or multi (multiple levels) are shown in 1,400 cases. From data of Krebs and Fishman.
Etiology
Vascular ingrowth is needed to supply the progress zone [C]. Failure results in insufficient mesodermal substrate. In the unifying theory of subclavian artery supply disruption sequence, the type of deformity depends upon the timing of the disruption. These defects are referred to as symbrachydactyly.
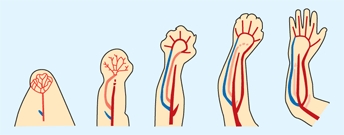
C Stages of vascular ingrowth and limb development Blood vessel ingrowth is essential to normal limb development, as shown in this sequence. Based on Gray’s Anatomy (1973).
Classification
The symbrachydactyly is a spectrum including the most common type of dysplasias [D].
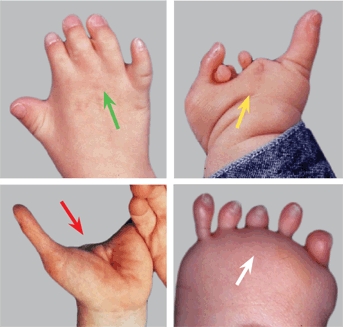
D Symbrachydactyly examples Short finger form (green arrow), cleft form (yellow arrow), monodactylous (red arrow), and peromelic form (white arrow).
Short finger form
may be associated with Poland anomaly.
Cleft form
previously called atypical cleft hand.
Monodactylous (thumb) form
The thumb is the best preserved digit.
Peromelic–transverse arrest form
This may occur at any level from shoulder to wrist. The feature that is always present is the nubbins at the end of the limb.
Evaluation
Although the diagnosis can usually be made by physical examination, obtain radiographs to document and classify the deficiency.
Screening examination
is necessary to identify other abnormalities such as radial head dislocations or radioulnar synostosis.
Family situation
should be evaluated carefully. Make certain that counseling is available for parents who are having difficulty dealing with the grief and guilt common in parents of limb-deficient children. Make a special effort to develop a warm and supportive relationship with the family because management is often difficult. Good rapport improves the child’s compliance with treatment and the parents’ acceptance of recommendations for management.
Management Principles
The following principles may be helpful in planning management.
Early prosthetics fitting is controversial
Some physicians believe that covering the limb with a prosthesis prevents sensory feedback and slows development of bimanual function. Others recommend the fitting of a passive prosthesis between 3 and 6 months of age to promote the development of a more normal self-image by the infant. Most children reject prostheses.
First prosthesis is usually passive
Convert to an active prosthesis based on the infant’s developmental age.
Myoelectric power
is inherently attractive to parents. Because these electrically powered limbs are expensive and difficult to maintain, long-term acceptance is poorer than for the simpler, body-powered prostheses.
Congenital and acquired amputations are different
Congenital amputees have normal sensation at the end of the limb, and are not troubled by overgrowth, scars, or pain, in contrast to those with acquired forms. Congenital amputees also develop better techniques of compensation.
Modify prosthesis
to facilitate activities of daily living. Make available an experienced occupational therapist to access the child’s needs and make recommendations for modifications that enhance self care.
Family support groups
are extremely valuable for both the parents and the child. Most childhood amputee clinics have ready access to these support groups and can help families make the necessary contacts.
Acceptance
is usually less for upper than for lower limb prostheses. The lack of sensibility and fine movement control makes upper limb prostheses less useful than those for the lower limb. Children are most likely to accept an upper limb prosthesis when a specific functional need is recognized. This awareness usually occurs at about 8 years of age.
Bilateral deficiencies
Rarely is prosthetic replacement useful or acceptable [A].

A Bilateral deficiencies Prosthetic replacement is seldom successful. Natural adaptations are more effective.
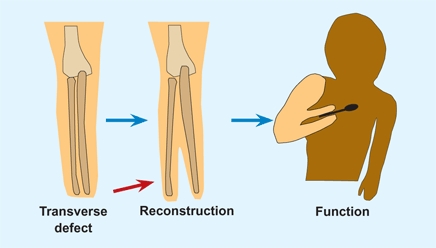
Most successful fittings
are for children with proximal transverse forearm deficiencies [B].

B Transverse forearm deficiencies Usually prosthetic fitting is successful.
Allow child natural adaptations
Such adaptations are usually practical, effective, and energy efficient [C].

C Natural adaptation These children become surprisingly proficient in using the feet to duplicate hand function. The child preferred using the lower limbs rather than the prosthesis.
Replace prosthesis
when destroyed, if it causes discomfort, or if it becomes suboptimal for function.
Discarding
of prosthetics is most common when deficiencies are extensive, prosthetic devices are complex in design, and natural adaptations without a prosthesis are effective.
Operative Procedures
Procedures have limited indications.
Revisions
for overgrowth may be necessary in both congenital and acquired transdiaphyseal amputations [D].

D Diaphyseal overgrowth This is a complication of through-bone amputations.
Krukenberg procedure
This reconstruction separates the radius and ulna to allow grasp with sensibility [E]. The outcome is usually functionally good but cosmetically poor. The procedure is appropriate for blind patients with acquired amputations who cannot visually position items in their prosthetic hands or hooks.
E Krukenberg reconstruction This separation of the distal radius and ulna (red arrow) and repositioning of forearm muscles provides the child with a functional grasp with sensibility.
Prosthetic Options
Terminal devices
Options include several alternatives.
CAPP (child amputee prosthetic project)
includes a closing spring and a frictional resilient covering that enhances control.
Hooks
with elastic closures and plastic covering are durable and can be fitted with body-powered opening mechanisms.
Cosmetic hands
may be passive, body-powered, or myoelectrically controlled.
Powering
devices include several options:
Body power
is commonly used for both opening of a terminal device and elbow flexion [B].
Myoelectric power
may be provided by single or double electrodes placed over flexor or extensor muscles. Single controls are usually applied during the second year with sensors placed over extensor muscles to activate the opening device. The terminal device stays open as long as the muscle is contracted. A second sensor over the flexors may be applied about age 3 for active flexion. These fittings are experimental but children have a lower dropout rate as compared with adults.
Cosmetic passive hand
is a commonly selected option due to its cosmetic advantage and simplicity.
Provide options
Consider providing the child with a variety of prosthetic options to help with normal activities of daily living. About half of children use multiple prostheses based on the situation.
Torticollis
Torticollis, or wryneck, includes a variety of conditions [B] that require different management.
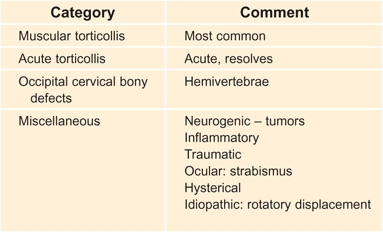
B Causes of torticollis The causes are many, but the vast majority of torticollis cases are due to disorders listed in the top three categories.
Acute Torticollis
Acute torticollis is relatively common. It may occur spontaneously, follow minimal trauma, or occur after an upper respiratory infection [A]. Why the head tilts is uncertain. The tilt may be due to muscle spasm secondary to cervical lymphadenitis or possibly due to a minor subluxation of the cervical vertebrae.

A Acute torticollis This form of torticollis develops suddenly in a previously normal child. Usually the deformity resolves spontaneously in a day or two.
Clinical features
Acute torticollis causes the head to tilt, rotate to one side and become fixed. Radiographs of the cervical spine are difficult to assess because of the lateral flexion and rotation. Laboratory studies are normal.
Manage
by immobilizing the neck with a folded towel and encourage rest. Early management is usually provided by the primary care physician. In most children, acute torticollis resolves within 24 hours. If the deformity persists longer than 24–48 hours, be more concerned and manage as rotatory displacement.
Rotatory Displacement
The more severe form of acute torticollis is called rotatory displacement or rotatory subluxation. This may be associated with severe pharangitis or otitis media, or follow head and neck surgery or trauma; in some cases, it occurs spontaneously. Treat rotatory displacement early to avoid permanent fixation and residual deformity [D].
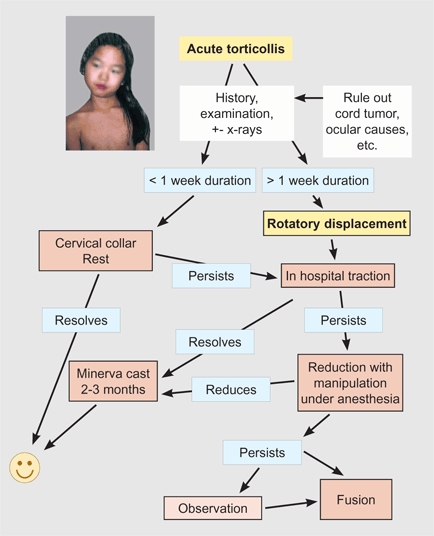
D Management of rotatory subluxation
Evaluate
Determine the duration of the deformity and any associated history such as trauma or infections. Sometimes torticollis follows head or neck surgery. Patients with Marfan syndrome are susceptible. Examine the child for localized tenderness and neck range of motion. Perform a careful neurological examination. Be aware that spinal cord tumors may present with torticollis. Perform appropriate laboratory studies if infection is suspected. The value and reliability of conventional and dynamic CT scans are controversial and probably have little value in planning management.
Manage
First apply traction. If early, head-halter traction is appropriate. In most children, the torticollis resolves with traction. If the deformity has persisted more than a week before resolution, consider extending the period of immobilization for 2 or 3 months using a Minerva cast [C]. For persisting deformity, halo traction or manipulation under anesthesia may be necessary. Should all these measures fail, operative repositioning and C1–C2 fusion may be necessary.
C Minerva cast This form of immobilization may be useful in children with delayed resolution of rotatory subluxation or requiring reduction. This type of cast is sometimes useful to provide immobilization following operative correction. The Minerva cast is better tolerated by the child than the parents. It is most easily applied with the child sitting or standing.
Chronic Nonmuscular Torticollis
In about 20% of children with chronic torticollis, it is due to nonmuscular causes. Radiographs may show conditions such as Klippel-Feil anomaly or hemivertebrae. If radiographs are negative and the sternocleidomastoid muscle is not contracted, consider an ocular etiology. Refer to an ophthalmologist for evaluation. Consider the other conditions that may cause torticollis, such as neonatal brachial plexus palsies and spinal cord tumors, before starting treatment.
Muscular Torticollis
Muscular torticollis is relatively common and presents in two age groups.
Infantile muscular torticollis
The infant [A] is first seen because of a head tilt. Sometimes a history of a breech delivery is given and a firm tumor of the sternocleidomastoid muscle is palpated. Usually only a head tilt and limited neck motion due to a contracture of the muscle are found. Plagiocephaly (asymmetrical head) may be present [B and C].


A Muscular Torticollis This is the most common neck problem in childhood. Torticollis is usually seen first in the infant (left). Some advocate treatment by stretching (right), but its value is uncertain.
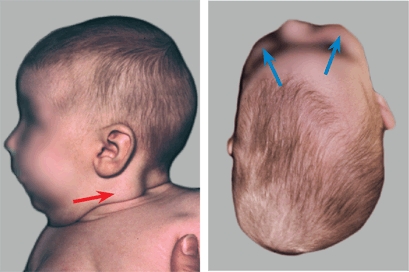
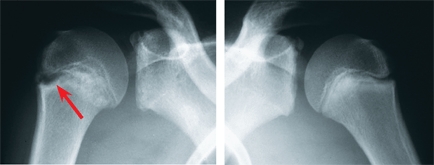
B Muscular torticollis and plagiocephaly The mass (red arrow) develops in early infancy and disappears spontaneously over a period of several months. The plagiocephaly (blue arrows) may persist longer.
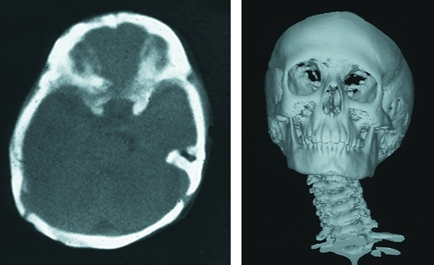
C Plagiocephaly torticollis Cranial deformity is readily shown by CT scans. 3-D reconstructions provide graphic documentation of the extent of the deformity.
Be certain to rule out developmental hip dysplasia. Even if the hip examination is negative, evaluate the hip by either ultrasound if the infant is seen in the neonatal period or by a single AP radiograph of the pelvis if the infant is older than about 10 weeks of age.
Infantile torticollis resolves spontaneously in about 90% of cases. The value of physical therapy by stretching is uncertain [A, right]. Of those that persist, operative correction may be necessary. Delay correction until about 3 years of age. Plagiocephaly rarely persists and is a cosmetic problem.
Juvenile muscular torticollis
Sometimes muscular torticollis appears to develop during childhood [D]. In this juvenile type, usually both heads of the muscles are contracted, causing the head tilt and limiting neck motion. This type of torticollis usually is permanent and often requires operative correction.
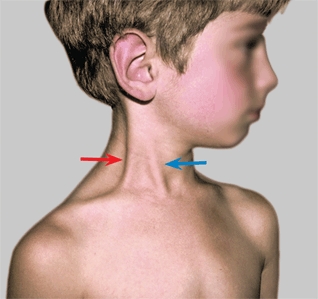
D Sternocleidomastoid contracture Both the clavicular origin (red arrow) and sternal origin (blue arrow) are contracted.
Operative correction
Bipolar release is the most effective procedure for correction of both infantile and juvenile forms of muscular torticollis.
Sprengel Deformity
Sprengel deformity is a congenital elevation of the scapula [A]. The deformity results from a failure of migration of mesenchyme during the second fetal month.

A Sprengel deformity Congenital elevation of the scapula causes a shoulder deformity (red arrows) that cannot be hidden by clothing. Some loss of abduction is a common mild disability (yellow arrow).
Clinical Features
The deformity varies in severity [B], is usually unilateral, and is associated with other abnormalities in 70% of cases. These associated abnormalities include absent or hypoplastic parascapular musculature, abnormalities in the cervicothoracic vertebrae or thoracic rib cage, presence of an omovertebral bone, limited shoulder abduction, and multidirectional shoulder instability. Because of restricted scapulothoracic motion, most shoulder motion occurs through the glenohumeral joint.
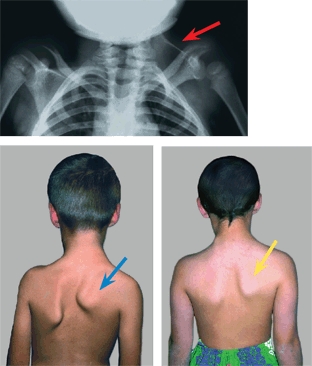
B Spectrum of severity Disability is proportional to the deformity. Shoulder elevation may be severe (red arrow), moderate (blue arrow), or mild (yellow arrow).
Management
When the deformity is mild, correction is not appropriate because the operative scar is often more unsightly than the deformity. For moderate deformity, excise the superior pole of the scapula. For severe deformity repositioning of the scapula is necessary. This repositioning requires an extensive soft tissue release, caudad repositioning of the scapula, and sometimes excision of the superior portion of the scapula. Perform the correction in early childhood when the scapula is most mobile. This mobility allows maximum correction with the least risk of complications. For correction, several procedures have been described. The Woodward procedure is most widely used.
Green procedure
Free all muscular attachments to the scapula, divide the omovertebral band, and rotate the scapula. Move the scapula caudad to a more normal position, and suture it into a pocket of the latissimus dorsi. In the original description of this procedure, traction was applied by a wire attached to the scapula and ilium to hold the scapula in the corrected position.
Klisic procedure
This procedure includes performing an osteotomy of the clavicle, extensive muscle releases, excision of the superior scapular margin, and securing the repositioned scapula with sutures to a vertebral spinous process and rib with absorbable sutures [C].
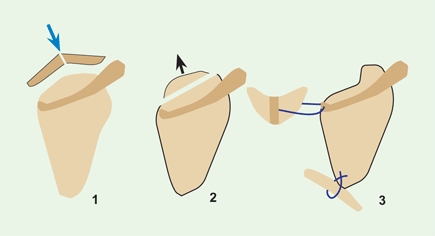
C Klisic procedure 1. The clavicle is divided (blue arrow). 2. The superior pole of the scapula is removed (black arrow) and the muscles are released. 3. The repositioned scapula is sutured to the rib and transverse processes (blue sutures). Based on Klisic (1981).
Woodward procedure
Exposure is made through a midline incision. Release the origins of the trapezius and rhomboid muscles, excise the omovertebral bone, and reposition the scapula [D]. Modifications include excising the superior and medial margins of the scapula.
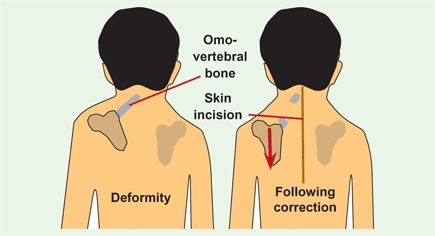
D Woodward procedure Through a midline incision, excise the omovertebral bone, release the soft tissue attachments, and reposition the scapula at a more distal location.
Neonatal Brachial Plexus Palsy
Neonatal palsy [A] is a traction injury to the brachial plexus that usually occurs during delivery. Risk factors include shoulder or fetal dystocia, obesity, and prolonged difficult labor. Despite improvements in obstetrical practices, the incidence of this palsy has not declined because of increases in birth weight and maternal obesity.

A Neonatal palsies These infants show moderate (yellow arrow) and severe (red arrow) palsies.
Natural History
Recovery depends upon severity. Overall, about half spontaneously completely resolve during the first year. Most improvement occurs in the first 3 months. Poor prognostic signs include the presence of a Horner syndrome, total plexus involvement, and a failure of return of function. Failure of recovery of elbow flexion by 3–6 months or, more accurately, failure of recovery of elbow flexion, wrist, and digital extension by 4 months correlates with a poorer prognosis. Common residual disabilities include loss of external rotation and abduction [C] and shoulder subluxation.

C Residual deformities in neonatal palsy Medial rotation (red arrow) and limited abduction (yellow arrow) are typical deformities that limit function.
Evaluation
Note the resting position and spontaneous movement of each joint of the upper limb. Evaluate for Horner syndrome, and assess the range of passive and active joint motion.
Anatomic classification
Severity is determined by the nature and extent of the lesion [B]. Mild lesions are stretch injuries of C5–C6. Severe injuries involve avulsion of nerve roots over multiple levels down to T1.
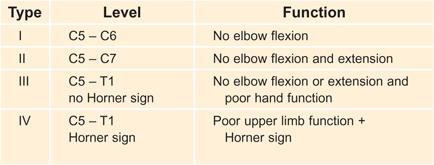
B Classification of brachial palsies Based on Narakas classification (1986).
Residual deformity
Use the modified Mallet classification. Five functions are assessed: hand-to-mouth, hand-to-neck, hand-to-spine, global abduction, and global external rotation. Each is graded from 1 to 4.
Management
Several forms of management may be useful.
Range of motion
Maintain joint mobility with passive rotation of the shoulder (especially external rotation), elbow, and wrist. Instruct parents how to gently range these joints with each diaper change.
Brachial plexus exploration
Evaluate those with severe injuries by CT and MRI studies. Plexus repairs are controversial, as results are unpredictable and should not compromise later reconstructive procedures. Consider early exploration in the first 3 months if Horner sign and a flail limb are present. Repairs of avulsion injuries are most uncertain and require transfers of intercostal or pectoral nerves. Direct nerve repairs are usually impossible, and sural nerve grafts to bridge a defect are needed. Reconstruction may again be considered between 4 and 6 months for less severe but persisting palsies.
Shoulder dysplasia
Children with residual muscle imbalance often develop progressive glenoid hypoplasia and an increasing posterior subluxation of the humeral head. Monitor by sonography. In some, Botox (botulinum toxin) may be helpful in reducing muscle imbalance to protect the joint from increasing dysplasia. Manage by release of the insertions of the pectoralis major, latissimus dorsi, and teres major, followed by a closed reduction of the glenohumeral joint. Transfer the latissimus dorsi and the teres major to the rotator cuff.
Muscle procedures
are indicated for children with disabling adduction and internal rotation contractures. The most common procedure is the Sever-L’Episcopo transfer. This procedure includes release of the pectoralis major, subscapularis, and joint capsule if contracted. The teres major and latissimus dorsi tendons are transferred from the anteromedial to the posterolateral aspect of the humerus. Axillary nerve palsy is a potential complication. This procedure is usually performed in early childhood.
Rotational humeral osteotomy
is indicated for an internal rotation deformity that limits function. Delay the procedure until mid or late childhood. Rotate the humerus to provide about equal internal and external rotation. Results are predictable, correction is usually permanent, and complications are infrequent.
Uncommon Upper Limb Conditions
Overuse Syndrome
Sometimes occurs in the shoulder involving the upper humeral epiphysis. The site is tender and radiographs may show widening of the physis [A].
A Overuse syndrome shoulder Note the widening and sclerosis adjacent to the proximal humeral epiphysis in this baseball pitcher.
Tumors
Lesions such as eosinophilic granuloma may cause shoulder pain [B].
B Eosinophilic granuloma These lesions present in unusual locations such as the scapula (red arrows). They typically cause pain.
Chronic Clavicular Osteomyelitis
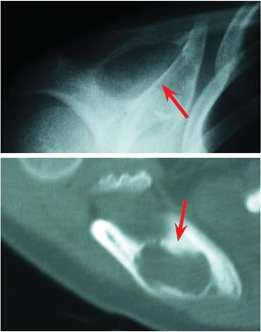
The response of the clavicle to inflammation is unique [C], as the clavicle becomes enlarged, sclerotic, and tender, and may be confused with a malignant etiology. Evaluate with radiographs, a bone scan, biopsy, and culture. MRI and CT studies may be useful in assessing adjacent joints and soft tissue. Often the pathology is that of osteomyelitis but the culture is negative and the cause is chronic recurrent multifocal osteomyelitis (CRMO). The clavicular lesion may be solitary or one of several sites. Manage CRMO with nonsteroidal antiinflammatory drugs. Recurrence is common.

C Chronic osteomyelitis of the clavicle Note the swelling and sclerosis of the clavicle (arrow). A low-grade staphylococcal infection was found.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








