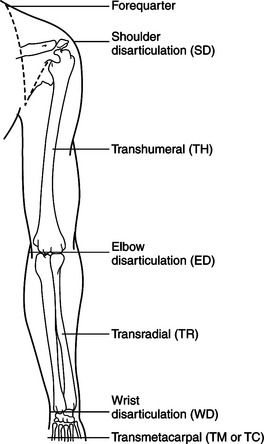
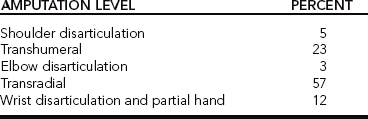
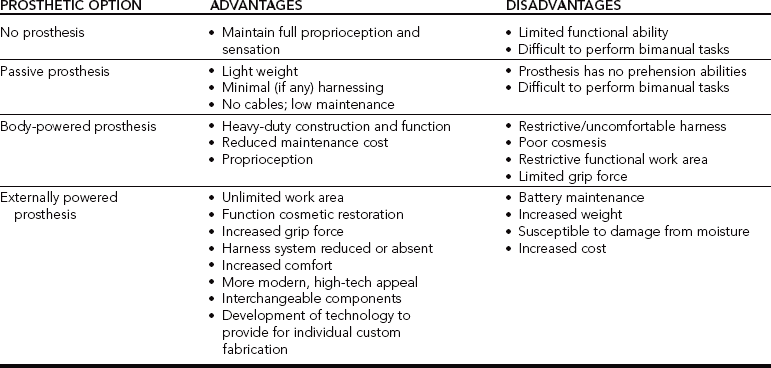
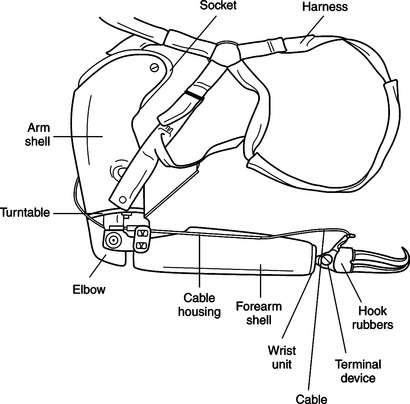
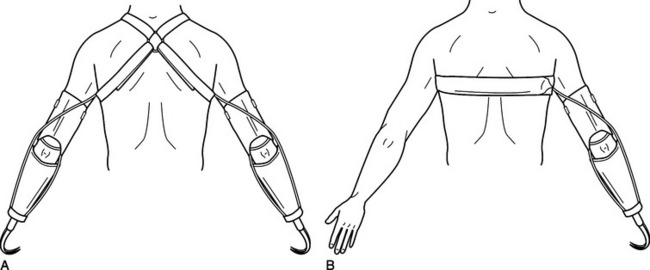
CHAPTER 18 1 Identify the characteristics of various upper extremity prosthetic devices. 2 Define the various causes and levels of amputation. 3 Differentiate between various levels of amputation. 4 Identify advantages and disadvantages of passive (semiactive), body-powered, externally powered, and recreational prostheses. 5 Differentiate the roles of the prosthetic team members. 6 Describe the sequence of training in prosthetic rehabilitation. 7 Explain the unique role of the occupational therapist in upper extremity prosthetic rehabilitation. 8 Identify psychosocial aspects of clients with amputations. 9 Describe upper extremity prosthetic intervention in children. 10 Discuss new updates in prosthetic technology and research. Orthotics and prosthetics are closely interrelated fields. Forty percent of American Board for Certification (ABC) certified practitioners hold credentials in both orthotics and prosthetics. This chapter is designed to serve as a resource for those therapists who serve this historically underserved population. Approximately 40,000 amputations occur each year in the United States. Thirty percent involve the upper extremity [Leonard and Meier 1988, Muilenburg and LeBlanc 1989], and upper extremity amputations represent approximately 10,000 people per year [Malone et al. 1984, Centers for Disease Control and Prevention 1996]. Approximately 50% of individuals are fitted with prostheses [Muilenburg and LeBlanc 1989]. Of the 50% fitted with a prosthesis, only half actually wear the device. Experts cite numerous reasons for this trend [Shurr and Cook 1990]. Fit and prosthetic training appear to be the most salient factors that affect prosthetic wear [Bennett and Alexander 1989]. The role of the prosthetist is to provide a well-fitting prosthetic device. It is the role of the occupational therapist to assist the individual to become an independent user of the device. The prosthesis is often heavy and awkward to use. If the fit is not tolerable, or if the potential wearer has not been properly trained to use the device, the prosthesis may end up on the closet shelf. Figure 18-1 provides an outline of the various amputation levels, along with abbreviations associated with them [Santschi 1958]. The more distal the amputation the greater the degree of natural function retained. Consequently, less is demanded of the prosthesis [Law 1981]. For example, an individual who has an amputation at the midhumeral level may be functionally able to use shoulder internal and external rotation along with other shoulder motions. However, the person lacks elbow flexion and extension and forearm supination and pronation. This is a disadvantage. If an individual with a midhumeral amputation wants to receive money from a cashier, more effort is required. The ability to pronate and supinate serves as a substantial advantage, enabling the person with the amputation to turn the prosthetic hand palm up as if to receive money from a cashier without the substitution movements of shoulder external rotation. Whether or not an individual chooses to wear a prosthesis, the level of amputation directly impacts function. The estimated frequencies of levels of amputation of the 50% who wear a prosthesis are presented inTable 18-1, indicating which level is most common [Muilenburg and LeBlanc 1989]. It is apparent that most amputations occur at the transradial level. The causes of upper extremity amputations differ from the causes of lower extremity amputations. Lower extremity amputations are largely a result of disease. The majority of upper extremity amputations result from trauma [Leonard and Meier 1988]. Other causes include disease, tumors, elective surgery, and genetic anomaly [Bennett and Alexander 1989]. Commonly, therapists work with individuals who before injury used their hands extensively in their daily occupations. Often these persons hope to regain a similar level of independence. A power-line worker describes his experience in the following words. The 7,200-volt power line was approximately five feet from where I came in contact with it. It’s a strange thing, but I don’t remember touching it. According to my co-workers, I started screaming and there was a bright electrical arc between my hands for about 10 seconds. The foreman shut off the power and got the boom truck to get me down…. I noticed there was no flesh on my hands anymore. Both hands were charcoal black! I knew they would have to be amputated, but the only thing I was concerned with was getting to a hospital to relieve some of the unbearable pain…. I’ve had four major operations at St. Elizabeth for amputations. I didn’t know for sure at the time how much they would have to take off. They amputated just above the elbow the first time. And I remember that the stumps looked pretty long the first time, but the second time they got a little shorter, and then the third time they really got short. On the fourth operation they removed an infected area from my right stump and armpit. I was given medication to help build tissue to fill those holes back in [Crane 1979, p. 10]. The team treating a person with an amputation is instrumental in the prosthesis-fitting process. The team consists of the person with the amputation, the prosthetist, and the therapist. The primary goal of therapy is to provide the individual with the proper tools and techniques to regain independence. A team approach combines expertise and experience, creating a synergy of professionalism, with team members working together and promoting the maximal level of independence for the individual with the amputation. The best results in upper extremity rehabilitation include interdisciplinary teamwork [Baumgartner and Bota 1992]. The primary member of this team is the person with the amputation. Individual goals, desires, and needs establish the foundation for which the team develops the action plan. Clients’ priorities for rehabilitation can vary. Common concerns include cosmesis, function, weight, maintenance, and funding for the prosthesis [Atkins et al. 1996]. For example, the needs of an individual with a transradial amputation who works full-time and desires to return to work may vary from those of an individual who is a stay-at-home parent. The type of prosthesis selected would vary, depending on a precise analysis of the client’s work, leisure activities, and ADL. An important aspect to the client is early postoperative prosthetic fitting. The advantages of early fitting are decreased edema, reduced postoperative and phantom pain, accelerated wound healing, improved rehabilitation, and decreased length of hospital stay [Malone et al. 1984]. The prosthetist has knowledge of the technology and componentry available. The prosthetist specializes in componentry, fit, and prosthesis fabrication. It is the responsibility of the prosthetist to understand the client’s primary diagnosis as it relates to the need for prosthetic services [Billock 2003]. The prosthetist must introduce, educate, and orient the client to the controls and functions of the prosthesis. Daily care and maintenance of the prosthesis are taught to the client by the prosthetist and should be reinforced by the therapist. The prosthetist and the therapist may collaborate when exploring the prosthetic options with the client. A well-rounded rehabilitation program is advised because the quality of training will directly determine how the individual uses the prosthesis for the rest of his or her life [Lake 1997]. The therapist has many responsibilities. It is important that therapists know the basic differences in prostheses to make proper recommendations of components to the team. Therapists should also recognize the importance of collaboration with skilled upper extremity prosthetists, with the purpose of maximizing the training process and the degree of independence [Atkins and Alley 2003]. Without proper therapy, the benefits of prosthetic use may be limited. The therapist reinforces and builds on residual movement, developing functional applications of the prosthesis to address the distinct ADL (e.g., brushing teeth) and instrumental ADL (e.g., driving) of each individual [Toren 2002]. The therapist is responsible for ensuring the client knows how to clean and maintain the prosthesis. In addition, the therapist provides opportunities for the client to practice using the prosthesis in specific daily activities. The therapist focuses on bilateral activities. Often, after amputation the individual becomes successful in performing some ADLs unilaterally. Thus, therapy must begin early in the rehabilitation process to facilitate use of the prosthesis in bilateral activities. Initial prosthetic training begins with a reorientation to the prosthesis and basic open-and-close control. Training then includes controlled grasp, such as opening in small increments to grasp small items and then more fully to grasp larger items. Training emphasizes grasping objects of varied texture and density to be handled. Sessions incorporate work on prehension and timing of release. Functional and appropriate tasks are encouraged and require the client to use the prosthesis for gross and fine motor activities. Training also emphasizes tasks to achieve all of these components in a variety of planes [Patterson et al. 1991, Keenan 1995]. With the combined efforts of the team members, the appropriate prosthetic components are chosen so that the individual can achieve goals through therapy, practice, and education. Generally, four categories of prosthetic options are available for the person with an upper extremity amputation. The options include (1) no prosthesis; (2) a passive (semiactive), cosmetic prosthesis; (3) a cable-driven body-powered prosthesis; and (4) an externally powered, electrically controlled prosthesis with either myoelectric sensors or specialized switches.Table 18-2 outlines the pros and cons of each prosthetic option [Law 1981, Muilenburg and LeBlanc 1989]. Wearing no prosthesis is one option, and for some individuals it is the best option. For example, an individual may not be able to tolerate the prosthesis for reasons such as residual limb hypersensitivity, soft tissue adhesions, and excessive scarring [Atkins and Meier 1989]. Individuals who choose not to wear a prosthesis may find advantages and disadvantages with their decision, which are found inTable 18-2. Advantages include increased proprioceptive and sensory input. Disadvantages include limited functional ability, difficulty in completion of bimanual tasks, and possibly the development of overuse syndrome and nerve entrapment in the contralateral limb [Reddy 1984]. Additional reasons an individual may not wear a prosthesis include not knowing the prosthetic options, having a bad first prosthetic experience, lack of funding, or reluctance to undergo revision surgery necessary for prosthetic fit and reduction of hypersensitivity [NovaCare 1991]. A passive (semiactive) prosthesis option is common for individuals who have had amputation distal to the elbow, in that they may maintain elbow flexion and extension and forearm pronation and supination. In this case, the obvious purpose is cosmetic. However, a passive prosthesis provides some degree of function. A passive prosthesis has many benefits, including its light weight, minimal (if any) harnessing, no cables, and low maintenance. Disadvantages include lack of prehensile abilities and difficulty in performing some bimanual tasks. Functionally, the digits of a passive prosthesis can be adjusted to assist with such activities as carrying a purse or a document or operating the gearshift in an automobile [Law 1981]. A body-powered prosthesis is a type of functional prosthesis most commonly used by clients with upper extremity amputations [Law 1981]. The body-powered prosthesis may not be cosmetically pleasing to everyone, but it is sturdy and allows for prehension. Body-powered upper limb prostheses are actuated by body motion, which generates tension in a cable. The cable courses from a shoulder harness through a helical coiled housing to a prosthetic component, such as a hook or elbow [Carlson et al. 1995]. In other words, the active movements of the shoulder and arm cause the tension in the cable to open and close the hand or handlike component (hook). The device is illustrated inFigure 18-2. Benefits of a body-powered prosthesis include its heavy-duty function and construction, decreased maintenance cost, and increased proprioceptive input. Disadvantages may include the restrictive uncomfortable harness, potential for nerve entrapment or compression, decreased cosmetic appearance, restricted functional work area, and limited grip force. Body-powered terminal devices generally weigh less than the externally powered prostheses because they lack the heavy motors and circuitry placed within them to operate the myoelectric signals [Atkins and Meier 1989]. The Harness.: The purpose of the harness is to suspend the prosthesis on the residual limb. It transmits force from the body to the prosthesis for independent operation of the prosthetic components [Muilenburg and LeBlanc 1989]. The body-powered prosthesis always requires harnessing. There are two primary types of harness: a figure-of-eight and a chest strap. The figure-of-eight harness passes over the shoulder, across the back, and under the contralateral axilla. “The ring lies flat in the back, inferior to C-7 and just to the sound side of the center of the spine” [Shurr and Cook 1990]. The standard figure-of-eight shoulder harness (Figure 18-3A) for the upper extremity has an axilla loop on the sound side that is commonly uncomfortable and can cause numbness and nerve damage [Collier and Le Blanc 1996]. The chest strap offers an alternative method of harnessing. It travels across the back, under the contralateral axilla, and across the chest (Figure 18-3B). It is important that the harness, either figure-of-eight or chest strap, be tight enough to activate the terminal device (TD) without excessive effort and loose enough to be comfortable and allow freedom of movement of both arms and shoulders. Long-term wear and inappropriate fit may cause discomfort or physical damage. The harness has been found to limit the functional work envelope, which is the space in front of the person who is able to use the prosthesis successfully for functional tasks. Harness systems limit successful prehension when the TD is outside the functional work area. With the body-powered prosthesis, function is limited above the head, behind the back, and near the ground, primarily because of the restricting harness (Figure 18-4). The prosthesis functions as a result of the ability to move in these planes. Discomfort and neurologic and musculoskeletal disorders can result from inefficient harness design [Carlson et al. 1995] and long-term wear. After years of wearing a harness, the axilla of the sound side experiences increased force and pressure to operate the prosthesis repetitively throughout the day. This can result in neurologic damage. A strong case can be made for providing a myoelectric or externally powered prosthesis that either eliminates or reduces the harnessing. This prevents the risk of long-term nerve damage on the sound side. The prosthetist is responsible for fabrication of the harness, and the therapist occasionally may make minor adjustments to improve function. Sometimes several harness options are attempted to find the type of system that best fits the amputee. It is often a trial-and-error process. Another important factor is the awareness of the increased workload in the remaining arm, which may produce symptoms ranging from minor aches to serious conditions such as nerve entrapment and overuse syndrome [Jones and Davidson 1999]. The Socket.: The socket is the part of the prosthesis that intimately fits over the individual’s residual limb. It is the connection between the prosthesis and the individual’s body. The socket is fabricated from an exact mold of the residual limb, and it is fabricated from various types of laminate or thermoplastic material. Development of high-temperature rigid plastic materials has made it possible to have total contact on the skin and allow decreased weight and increased durability. The use of carbon graphite and the introduction of flexible thermoplastics are more comfortable, lighter, and durable and have made soft sockets with windows possible. The prosthetist makes modifications over bony prominences and areas susceptible to torque and shear forces [Andrews and Bouvette 1996]. Typically, three to four sockets will be fabricated before the final one is delivered. Intimate socket fit provides a stable foundation of support necessary to transfer forces from the TD. It provides evenly distributed pressure on the residual limb, which prevents skin breakdown or pressure sores. In the last decade, a multitude of design innovations have been incorporated, which have resulted in developing better comfort, suspension, stability, and range of motion. The new fitting techniques and socket designs appear to be more efficient for force of transmission and motion capture and more functionally consistent than traditional sockets [Alley 2002]. Occasionally, the prosthetist instructs the individual to wear the socket before all components are attached. This increases wearing tolerance and facilitates reshaping of the residual limb. As the person with the amputation ages, physical and physiologic changes occur. The person may experience weight loss or gain or muscle bulk increase or decrease. These changes have an impact on the size and condition of the residual limb, and the socket may no longer fit as it should. A new socket must be fabricated to fit the exact shape of the residual limb when changes occur. When a new socket is fabricated, it replaces the poorly fitting one in the individual’s current prosthesis. An entirely new prosthesis is not needed because the socket is removable and replaceable. This saves on cost. The wearer of a body-powered prosthesis may benefit from using a second sheath or sock made of either a fabric or a gel-like substance to manage poor skin integrity, prevent breakdown, absorb moisture, or provide padding.
Upper Extremity Prosthetics
Amputation Levels and the Impact on Function
Causes of Upper Extremity Amputations
The Team Members
The Client
The Prosthetist
The Occupational Therapist
Prosthetic Options
No Prosthesis
Passive Prosthesis
Body-powered Prosthesis
Body-powered Prosthetic Components
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Upper Extremity Prosthetics