Nicole Sasson Provide patient care that is compassionate, appropriate, and effective for the treatment of the adult with an upper extremity amputation. 1. Describe the key components of the assessment of the adult with an upper extremity (UE) amputation. 2. Describe potential injuries associated with UE amputation. 3. Formulate the key components of a rehabilitation treatment plan for the adult with UE amputation. The evaluation and assessment of the patient with an upper extremity (UE) amputation drives the rehabilitation process. UE amputations can be divided into two categories: congenital and acquired. Most acquired UE amputations are traumatic in nature (1). It is essential to obtain a detailed medical and surgical history including the cause and nature of the amputation and surgical interventions as well as any complications encountered. A patient with an upper limb amputation is unique and no two amputations are the same. A person with an UE amputation is initially devastated and more so if the amputation is bilateral, as we as humans are dependent on the use of our arms and hands. Patients are usually unable to perform a simple task initially. Patients with UE amputations may have suffered concomitant traumatic brain injury and brachial plexus injury, which might impact their rehabilitation program. In cases where resection of a malignancy was the cause of the amputation, it is important to obtain information about the type and stage of the cancer as well as treatments used. The treatments may have included prior surgical resections, chemotherapy, or radiation therapy. The past medical history should document previous hand dominance. There should be a detailed history concerning the existence of comorbid vascular, endocrine, rheumatologic, orthopedic-musculoskeletal, and neurologic diseases. Renal impairment and fluctuations in fluid retention are important issues when prescribing a prosthesis. A complete review of symptoms of overall health and comorbidities, is necessary for the team to consider before pursuing prosthetic options on an individual basis. The presence of phantom limb sensation, phantom limb pain, and presence of neuromas and the need to treat (and with what classes of medications) should be documented. It is also important to ask the patient about musculoskeletal pain in the residual part of the amputated extremity, visual symptoms, and the presence of depression or anxiety—all of which can potentially have an adverse effect on the successful rehabilitation of the patient. The past surgical history should document all interventions including bony fixations, myodesis, myoplasty, cineplasty, and angulation-osteotomy (see Table 9.3). Fracture interventions; revascularization attempts; placement of skin grafts and type, including presence of surgical scars and associated adherence to the underlying residual structures; and presence of neuromas are all very important to record and consider. A functional history should be taken, documenting the performance of activities of daily living including personal hygiene, dressing, feeding, and vocational activities. Vocational and leisure needs provide important information for the team to consider in prescribing an appropriate prosthetic limb and engagement into the rehabilitation process. Physical examination of the UE amputee should document pertinent points in the past medical history and past surgical history already mentioned. Residual limb length and shape should be recorded and assessed with the following points in mind. 1. Transradial—Ideally, the residual limb retains the configuration of an intact UE limb. The longer, the better for the lever arm, with more physiologic pronation and supination. This is ideal for a body-powered UE prosthesis. This can be used to perform manual labor. Presence of the brachioradialis muscle results in improved elbow movement. Residual limbs shorter than the medium length (<55% transradial length) are ideal candidates for externally powered prostheses such as a myoelectric or a hybrid prosthesis. 2. Transhumeral—Ideally, the residual limb should be cylindrical in nature with retention of the tuberosity of the deltoid. The longer the better for the lever arm, where retention of the affected humerus compared with the sound limb is 50% to 90%. Range of motion and presence of contractures of the residual limb should be recorded. Skin integrity is also an important concern since it is needed to suspend the prosthesis and control the terminal device of an UE prosthesis. On inspection, it is important to look for scars, bony or soft-tissue deformities, and burns. On palpation, it is important to feel for skin adhesions and tender areas as well as ascertain for the presence of neuromas, which can be a source of pain for the patient. In UE amputations secondary to trauma, key neurologic or vascular structures in the limb may have been injured; therefore, an assessment is warranted. This should include an evaluation of the muscles and key sensory areas supplied by the brachial plexus and its terminal branches, as well as performing an evaluation of the vascular supply to the limb. Motor strength of key muscle groups in the affected UE as well as in the sound extremity is important to record. Sensory testing should include light touch, pinprick, and proprioception. A brief cognitive evaluation can also be helpful in cases where significant trauma was associated with the limb amputation since the presence of a brain injury can signal challenges in learning how to use the prosthesis safely and may require additional testing. Level of alertness, orientation, attention span, immediate and delayed recall, and judgment are some key areas to focus on. Visual acuity plays an important role while using UE devices and deficits should be recorded. Imaging studies such as x-rays and MRIs of the residual limb can provide significant information regarding the osseous and soft-tissue integrity of that limb. Electrodiagnostic studies can provide information regarding injury to the brachial plexus and its terminal branches. Successful outcomes in rehabilitation for the UE amputee, whether unilateral or bilateral, are dependent on multiple factors including early posttraumatic intervention, an experienced team approach, patient-directed prosthetic training, patient education, and on-going patient evaluation and follow-up (2). The use of rigid dressings and early fitting in patients with transhumeral or more distal amputations encourages the resumption of bimanual activities, promotes wound healing, and decreases edema. This can lead to a greater acceptance and use of the prosthesis. There is a known direct relationship with time of fitting of prosthetic device and long-term prosthetic use. Which usually should happen in the first month following the amputation (3). Earlier application of the UE prostheses also helps to decrease the incidence of phantom limb pain that can disrupt prosthetic training and use. There are multiple steps in the rehabilitation of the UE amputee (Table 9.1). Ideally, the physiatrist should be involved early and in all of the steps. Preamputation counseling involves education on the specific surgical intervention, the subsequent rehabilitation, and basic prosthetic design options as well as peer visitation and psychological counseling. Pain control is tantamount to successful rehabilitation. Once stable surgically, range of motion, strengthening, massage and desensitization, and wound care of the residual limb must be stressed to prepare for successful prosthetic fitting and use. Avoiding contracture development is important in postfracture priority. The transhumeral residual limb’s preferable shape is cylindrical with retention of the deltoid tuberosity. Unilateral UE amputees usually perform all tasks and activities of daily living (ADLs) with their intact side. Commonly, they will experience overuse syndromes and must be educated to avoid this. Overuse injuries are more common, the more proximal the amputation. They can present with decreasing frequency in the elbow, shoulder, and least commonly in the wrist joint. Pain syndromes are common in UE amputees. Phantom sensation is felt by nearly all “acquired amputees,” but is not always troublesome (1). Aggressive preamputation pain management leads to better postsurgical pain states. Use of a patient-controlled analgesia (PCA) system is the standard pre- and postoperatively followed by scheduled parental/oral analgesia. Therapeutic desensitization modalities to assist in pain management are introduced first with edema control, light touch and tapping, and transcutaneous nerve stimulation. Virtual imaging techniques, mirror therapy, and acupuncture (4) have also been found to be quite helpful. Severe cases might necessitate nerve blocks: ganglion, epidural nerve blocks with steroids. Surgical intervention is deemed as a last resort as it is not as successful. TABLE 9.1 Steps in UE Amputee Rehabilitation
![]()
9: Upper Extremity Limb Loss
![]()
PATIENT CARE
GOALS
OBJECTIVES
Ideal residual Limb Length and Shape
Imaging and Other Diagnostic Studies
Rehabilitation of the Upper Extremity Amputee
STAGES OF AMPUTATION REHABILITATION |
Preamputation counseling |
Amputation surgery |
Acute postamputation period |
Preprosthetic training |
Preparatory prosthesis fitting |
Prosthetic fitting and training |
Reintegration into the community/advanced functional skills training |
Long-term follow-up |
STAGES OF REHABILITATION |
Acute care |
Support |
Pain management Wound care |
Preprosthetic training |
Comprehensive evaluation |
Edema control and limb shaping |
Pain control |
Adaptation to body image |
Soft-tissue desensitization/ROM/strength training |
Maximize left/right dominance retraining hand dominance |
Myo-site testing |
Bilateral UE amputees perform ADLs with their feet—especially when congenital in nature; however, as the child ages, he or she should be fit with prostheses. The rule when prescribing prostheses for pediatric patients is “fit to sit (5).” This occurs by 6 months of age with an initial prosthesis that has a passive terminal device. When no “normal limbs” remain for comparative measurement, the normal upper arm length is estimated by multiplying the patient’s height by 0.19 and normal forearm length is estimated by multiplying the patient’s height by 0.21 (6).
The health care certifying organization, Joint Commission (JCAHO), has standards for spiritual care that state that each patient’s “spiritual care be assessed, accommodated, and attended to in ways that are important to them” (7). These standards are typically followed upon admission to the hospital. The admissions personnel ask patients to state their religion and whether or not they would like to see a chaplain. But the chaplain can also serve as a member of the interdisciplinary rehabilitation team and assist the patient in his or her rehabilitation program. JCAHO stresses that the cultural and spiritual beliefs of our patients are met (7), whereas the Commission on Accreditation of Rehabilitation Facilities (CARF) advocates a more holistic approach to the care of the amputee, treating the mind and the body of the patient. CARF emphasizes delivery of exceptional medical care as well as meeting the cultural, spiritual, and educational needs of this population (8).
MEDICAL KNOWLEDGE
GOALS
Demonstrate knowledge of established and evolving biomedical, clinical, and epidemiological sciences pertaining to UE amputees, as well as the application of this knowledge to guide holistic patient care.
OBJECTIVES
1. Describe the epidemiology of upper limb loss.
2. Describe the common anatomical levels of upper limb amputations and their relevance to prosthetic prescription.
3. Review the prosthetic prescription for the individual with upper limb loss.
Each year approximately 185,000 persons undergo an amputation of their limbs (1). There are more than 1.9 million persons living in the United States with limb loss (9). Lower extremity (LE) amputations are most commonly due to dysvascular disease, whereas upper limb amputation is relatively rare and mainly traumatic in origin, affecting 41,000 persons or 3% of the U.S. amputee population (1,9). Major amputations of the upper extremity (UE) (other than digital amputations) account for 3% to 15% and are approximately 20 times less common than LE amputations. UE amputations can be broken down into two groups: congenital and acquired. Reasons for congenital malformations are largely unknown but are thought to be due to exposure to teratogenic agents and/or environmental radiation. Approximately 60% of limb deficiencies in children are congenital and involve the UE compared with the LE in a 2:1 ratio. The most common deletion of the UE is the absence of the left transverse radius (10). Most amputees (68.6%) who have lost limbs to traumatic injuries have lost an upper limb (9,11). Traumatic amputation is the major reason for UE limb loss in the military. This population has grown in particular with the last two military conflicts, Operation Iraqi Freedom and Operation Enduring Freedom in Afghanistan. UE amputations are more common in men than in women: 4 to 6/1 ratio. The majority of these amputations occur in the 20- to 40-year-old age group. Most of the service men and women who undergo amputation will have polytraumatic injuries, including traumatic brain injuries and multiple amputations. OSHA regulations over the past decades have decreased the incidence of occupational workplace incidents. Malignant tumors are the primary reasons for shoulder disarticulation and forequarter amputations (12) (Table 9.2).
Length of the residual limb should be preserved using microvascular anastomosis, distal free flaps, and spare part flaps from the amputated limb, if possible (12), as the level of amputation is the single most important determination of function. However, transcarpal amputation and wrist amputation are seen less frequently because of limited functional outcome (1) with an UE prosthesis (Tables 9.3 and 9.4).
Prosthetic Prescription
Prostheses prescription for the UE amputee has become quite intricate with new technology and componentry being developed since the 1980s. High technology is not required of all users and should be determined by the interdisciplinary team. UE amputees have chore-specific arms fabricated, with body powered being the staple one.
TABLE 9.2 Etiology of Upper Limb Amputations (Decreasing Frequency)
Trauma (80%–90%) |
Congenital (9%) |
Cancer (8%) |
Vascular complications of disease (6%) |
TABLE 9.3 Levels of Amputation (Distal to Proximal) and Lengths of Residual Limbs
Transcarpal |
Below-Elbow Amputation |
Wrist disarticulation |
Transradial |
Long 55%–100% |
Short 35%–55% |
Very short <35% |
Elbow disarticulation |
Above-Elbow Amputation |
Transhumeral |
Standard 50%–90% |
Short 30%–50% or less |
Shoulder disarticulation |
Interscapulothoracic disarticulation “forequarter” |
TABLE 9.4 Surgical Techniques
Myodesis: Direct suturing of residual limb musculature or tendon to the bone/perisoteum. |
Myoplasty: Suturing of agonist–antagonist muscle pairs to each other. |
Cineplasty: Surgical isolation of a loop of muscle (biceps/pectoralis most common) covering it with skin. |
Angulation–Osteotomy: Skeletal alteration of the humerus aiding in suspension of a prosthesis, facilitating rotation. |
Osseointegration (12) |
Targeted muscle reinnervation: Rerouting of nerves to existing unused residual limb musculature. |
Hand transplants (13) |
Terminal Device
The functional activities of the hand are intricate but can be separated into two groups: nonprehensile and prehensile. Voluntary opening terminal devices are normally held closed by a spring or a rubber band and open when the control cable is pulled. It takes the shape of a “c” configuration. Each rubber band produces approximately 0.45 kg (1 lb of prehensile force) between the hook fingers. A version of this type of terminal device is the most commonly prescribed type of terminal device in our country because of its versatility and reliability. The type of metal used depends on the length of the residual limb. A transradial amputee would probably receive a stainless steel hook, whereas a transhumeral amputee would probably receive an aluminum alloy hook to ease the weight and effort needed with elbow flexion.
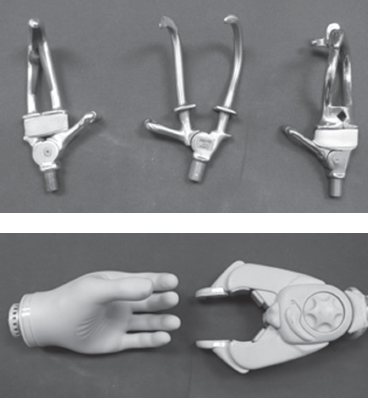
FIGURE 9.1 Prehensile and Nonprehensile Devices
 Transradial amputation (TR) may allow lifting of 20 to 30 lbs
Transradial amputation (TR) may allow lifting of 20 to 30 lbs
 Terminal device (TD) is the most important functional part of the upper extremity prosthesis
Terminal device (TD) is the most important functional part of the upper extremity prosthesis
![]() Passive–cosmetic
Passive–cosmetic
 Flexible passive mitts–sports/task specific
Flexible passive mitts–sports/task specific
 Voluntary–opening (VO) split hook type; usually made of aluminum, more lightweight; most common and practical
Voluntary–opening (VO) split hook type; usually made of aluminum, more lightweight; most common and practical
 Specialized work hook-type (i.e., farmer’s hook); made of stainless steel, heavier in nature
Specialized work hook-type (i.e., farmer’s hook); made of stainless steel, heavier in nature
 CAPP (Child Amputee Prosthetics Project) alligator or helper
CAPP (Child Amputee Prosthetics Project) alligator or helper
 Prehensile forces are determined by the number of rubber bands. Can use up to 10 bands
Prehensile forces are determined by the number of rubber bands. Can use up to 10 bands
 Nonamputee male pinch force is 15 to 20 lbs
Nonamputee male pinch force is 15 to 20 lbs
![]() Voluntary–closing (VC) hook type is not limited by rubber band strength or springs
Voluntary–closing (VC) hook type is not limited by rubber band strength or springs
 Gradient of pinch is dependent on the force exerted
Gradient of pinch is dependent on the force exerted
 Provides better control of closing pressures, but active effort is required to maintain closure or items may be dropped
Provides better control of closing pressures, but active effort is required to maintain closure or items may be dropped
 Myoelectric hands—offer spherical/palmar grasp with grip forces greater than VO/VC TDs. More cosmetically appearing but more fragile
Myoelectric hands—offer spherical/palmar grasp with grip forces greater than VO/VC TDs. More cosmetically appearing but more fragile
 One-site two-function controllers use weak versus strong contractions of the same muscles to operate the TD
One-site two-function controllers use weak versus strong contractions of the same muscles to operate the TD
 Two-site two-function controllers use different muscles to open and close the TD
Two-site two-function controllers use different muscles to open and close the TD
 Wrist unit
Wrist unit
![]() Friction wrist units
Friction wrist units
 Constant—friction wrist units
Constant—friction wrist units
 Allows passive pronation/supination, but rotates when holding heavy objects
Allows passive pronation/supination, but rotates when holding heavy objects
![]() Active pronation/supination
Active pronation/supination
![]() Quick-disconnect wrist unit
Quick-disconnect wrist unit
![]() Wrist flexion units—spring assisted, useful for midline activities: eating, hygiene, toileting, and dressing not usually seen in unilateral but bilateral amputees because of increased weight at the end of the prosthesis
Wrist flexion units—spring assisted, useful for midline activities: eating, hygiene, toileting, and dressing not usually seen in unilateral but bilateral amputees because of increased weight at the end of the prosthesis
![]() Rotational wrists—lock in place
Rotational wrists—lock in place
 Elbow unit
Elbow unit
![]() Attaches to the triceps pad and to the prosthetic forearm
Attaches to the triceps pad and to the prosthetic forearm
![]() Flexible hinges—Dacron webbing; leather or metal cable allowing approximately 50% of residual rotation for amputations through the distal one-third of the forearm
Flexible hinges—Dacron webbing; leather or metal cable allowing approximately 50% of residual rotation for amputations through the distal one-third of the forearm
![]() Rigid hinges—for amputations at or above the mid-forearm level; eliminates rotation
Rigid hinges—for amputations at or above the mid-forearm level; eliminates rotation
![]() Single axis hinges—for shorter residual limb set in pre-flexion to prevent hyperextension of the elbow.
Single axis hinges—for shorter residual limb set in pre-flexion to prevent hyperextension of the elbow.
![]() Polycentric hinges—for short transradial amputees; provides room in the cubital fossa increasing range of motion (ROM)
Polycentric hinges—for short transradial amputees; provides room in the cubital fossa increasing range of motion (ROM)
![]() Step-up hinges—split socket configuration; enhances flexion
Step-up hinges—split socket configuration; enhances flexion
 For a short TR amputation used to provide a 2:1 ratio of flexion to socket motion
For a short TR amputation used to provide a 2:1 ratio of flexion to socket motion
![]() This requires the amputee to use approximately twice as much force to flex the prosthesis
This requires the amputee to use approximately twice as much force to flex the prosthesis
 Sliding action joint
Sliding action joint
 Geared joint
Geared joint
 Socket double walled for optimal fit
Socket double walled for optimal fit
![]() Outer wall is rigid and serves to connect to other components
Outer wall is rigid and serves to connect to other components
![]() Inner wall is fit precisely to the shaped residual limb
Inner wall is fit precisely to the shaped residual limb
![]() Suction socket can provide self-suspension without straps
Suction socket can provide self-suspension without straps
 Munster supracondylar socket can provide suspension to a very short transradial amputee but precludes full elbow extension; can be used for externally powered TD
Munster supracondylar socket can provide suspension to a very short transradial amputee but precludes full elbow extension; can be used for externally powered TD
 Harness
Harness
![]() Figure of 9—for a long transradial amputation or a wrist disarticulation; requires a self-suspending socket, is generally more comfortable than a “figure of 8.”
Figure of 9—for a long transradial amputation or a wrist disarticulation; requires a self-suspending socket, is generally more comfortable than a “figure of 8.”
![]() Figure of 8—short transradial or more proximal amputation
Figure of 8—short transradial or more proximal amputation
![]() Axilla loop—Primary Anchor from which two other straps originate; encircles the shoulder girdle on the nonamputated side.
Axilla loop—Primary Anchor from which two other straps originate; encircles the shoulder girdle on the nonamputated side.
![]() Anterior support strap or the “inverted Y suspensor.”
Anterior support strap or the “inverted Y suspensor.”
![]() Connects to the triceps pad or half arm cuff, usually with an elbow hinge one cable or single control system that attaches proximally to one of the nonelastic straps of the harness and distally at a prehension device or TD
Connects to the triceps pad or half arm cuff, usually with an elbow hinge one cable or single control system that attaches proximally to one of the nonelastic straps of the harness and distally at a prehension device or TD
![]() Bilateral Transradial Harness—omits the axilla loops
Bilateral Transradial Harness—omits the axilla loops
 Transhumeral (TH)amputation may be able to lift 10 to 15 lb
Transhumeral (TH)amputation may be able to lift 10 to 15 lb
 Terminal device—as above
Terminal device—as above
 Wrist unit—as above
Wrist unit—as above
 Elbow unit has an alternator lock that alternately locks and unlocks with the same movement
Elbow unit has an alternator lock that alternately locks and unlocks with the same movement
![]() With the elbow unlocked, body movements will flex or extend the elbow with the cable
With the elbow unlocked, body movements will flex or extend the elbow with the cable
![]() With the elbow locked, the cable will operate the TD
With the elbow locked, the cable will operate the TD
![]() Outside locking hinges—Elbow disarticulation/transcondylar amputation
Outside locking hinges—Elbow disarticulation/transcondylar amputation
![]() Inside Locking Hinges—Transhumeral amputations, if 5 cm proximal to the elbow joint
Inside Locking Hinges—Transhumeral amputations, if 5 cm proximal to the elbow joint
![]() Flail—arm hinges—postbrachial plexus lesions
Flail—arm hinges—postbrachial plexus lesions
![]() Ratchet hinge—postbrachial plexus injury works like a beach chair positioning
Ratchet hinge—postbrachial plexus injury works like a beach chair positioning
![]() Friction units—lightweight, passive positioning
Friction units—lightweight, passive positioning
![]() Flexion assist—counterbalances the weight of the prosthetic forearm
Flexion assist—counterbalances the weight of the prosthetic forearm
![]() Nudge control unit—originally designed to lock and unlock the elbow
Nudge control unit—originally designed to lock and unlock the elbow
 Can also be adapted to operate other components, including flexion and rotation wrist units
Can also be adapted to operate other components, including flexion and rotation wrist units
 Shoulder unit
Shoulder unit
![]() Bulkhead-humeral segment is connected directly to the socket; makes the prosthesis lightweight
Bulkhead-humeral segment is connected directly to the socket; makes the prosthesis lightweight
![]() Friction loaded-passively moveable; provides assistance with dressing and tabletop activities
Friction loaded-passively moveable; provides assistance with dressing and tabletop activities
![]() Single axis—permits abduction
Single axis—permits abduction
![]() Double axis—permits abduction and flexion
Double axis—permits abduction and flexion
![]() Triple axis—permits passive motion
Triple axis—permits passive motion
![]() Ball and socket—permits passive motion
Ball and socket—permits passive motion
![]() Locking shoulder—can stabilize the shoulder in 36 different flexion positions; can be used with an externally powered terminal device (TD); a second friction-controlled hinge provides abduction and adduction stabilization
Locking shoulder—can stabilize the shoulder in 36 different flexion positions; can be used with an externally powered terminal device (TD); a second friction-controlled hinge provides abduction and adduction stabilization
 Socket—double walled for optimal fit
Socket—double walled for optimal fit
![]() Suction socket can provide self-suspension without straps
Suction socket can provide self-suspension without straps
![]() Munster supracondylar socket can provide suspension to an elbow disarticulation by encasing the humeral condyles; can be used for externally powered TDs.
Munster supracondylar socket can provide suspension to an elbow disarticulation by encasing the humeral condyles; can be used for externally powered TDs.
 Harness
Harness
![]() Figure of 8—short transradial or more proximal amputation (see previous)
Figure of 8—short transradial or more proximal amputation (see previous)
![]() Shoulder Saddle with chest straps frees the opposite shoulder
Shoulder Saddle with chest straps frees the opposite shoulder
![]() Relieves the pressure caused by the axillary loop of the “8”
Relieves the pressure caused by the axillary loop of the “8”
![]() Heavy loads are tolerated better
Heavy loads are tolerated better
![]() Poor cosmesis
Poor cosmesis
![]() Donning requires assistance and is more difficult
Donning requires assistance and is more difficult
 Endoskeletal upper limb prostheses vs. exoskeletal upper limb prostheses
Endoskeletal upper limb prostheses vs. exoskeletal upper limb prostheses
![]() Systems with tubular humeral and forearm elements
Systems with tubular humeral and forearm elements
 Encasement in a cosmetic foam cover and components above
Encasement in a cosmetic foam cover and components above
 Lightweight compared to exoskeletal UE prostheses
Lightweight compared to exoskeletal UE prostheses
 Necessary movements for body-powered prosthesis control
Necessary movements for body-powered prosthesis control
 Transradial (TR)Amputations
Transradial (TR)Amputations
 Glenohumeral forward flexion
Glenohumeral forward flexion
![]() Natural movement
Natural movement
![]() Generates good force to reach and activate TD or flex an elbow
Generates good force to reach and activate TD or flex an elbow
![]() Biscapular abduction
Biscapular abduction
![]() Generates weak force that may activate TD while it remains still to perform midline activities
Generates weak force that may activate TD while it remains still to perform midline activities
 Transhumeral (TH)Amputations
Transhumeral (TH)Amputations
 Glenohumeral forward flexion
Glenohumeral forward flexion
 Glenohumeral depression, extension, and abduction
Glenohumeral depression, extension, and abduction
![]() Unnatural and difficult
Unnatural and difficult
![]() Unlocks or locks elbow
Unlocks or locks elbow
 Scapular adduction/chest expansion
Scapular adduction/chest expansion
![]() Unnatural
Unnatural
![]() Unlocks or locks elbow
Unlocks or locks elbow
![]() Allows TD functions
Allows TD functions
 Scapular elevation
Scapular elevation
![]() Requires another strap-waist belt
Requires another strap-waist belt
![]() Unlocks or locks elbow
Unlocks or locks elbow
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






