Chapter 13 Unloading the Patellofemoral Joint for Cartilage Lesions
Introduction
Successful outcomes in patellofemoral cartilage restoration procedures rest on the need to unload the patellofemoral joint. Initial patellofemoral cartilaginous procedures were predisposed to failure because of overload of the patellofemoral compartment or failure to address patellar malalignment. Malalignment is defined as abnormal tilt and or subluxation of the patella,1 and distal realignment (i.e., tibial tubercle osteotomy) is the most definitive method of either realigning a subluxated/tilted patella or offloading the patellofemoral compartment.
Anteromedialization of the tibial tubercle addresses patellar malalignment, patellar arthritis, or is used in conjunction with cartilage restoration procedures. The original technique, as described by Dr. Fulkerson in 1983,2 has been shown in long-term studies to provide long-term relief from instability and patellofemoral pain.3 The idea behind the osteotomy is to alleviate stress from the distal and lateral portions of the patella and trochlea to the proximal and medial patellar articular cartilage.2,4–7 By changing the angle of the osteotomy cut, one can customize the procedure to include more medialization for instability cases or more anteriorization for cartilaginous unloading guidelines. Typically, in most procedures done for cartilage restoration, there is some evidence of patellar malalignment, so a combination of both medialization and anteriorization is chosen.
Indications/Contraindications
Indications for anteromedialization of the tibial tubercle include patellofemoral pain with either lateral or distal patellar arthrosis or lateral subluxation/dislocation of the patella. Other indications include a failed lateral release8 and cartilage restoration procedures that need offloading of the newly regenerated or implanted cartilage cells. The ideal candidate is a patient with lateral patellar tilt (or subluxation) with grade III or IV articular cartilage degeneration localized to the lateral patellar or distal medial patellar facets. Not only should the patient be deemed psychologically mature to undergo the surgical procedure, but he or she should also have failed a course nonoperative management consisting of patellar taping, lateral retinacular mobilization, stretching of the extensor mechanism, bracing, and nonsteroidal anti-inflammatory medication.1,2,7
Preoperative Planning
Physical Examination
Specific tests for the evaluation of the patellofemoral joint include noting patellofemoral crepitance, joint effusion, lower extremity Q-angle, patellar J-sign, lateral retinacular tightness, patellar quadrant mobility, patellar apprehension test, patellar grind test, and stability/pain relief with a lateral to medial force on the patella (i.e., you are simulating holding the patella in an unloaded/reduced position).
Imaging Studies
Imaging studies should start with a complete set of knee x-rays consisting of bilateral anterior-posterior (AP) standing views, bilateral posterior-anterior (PA) 45 degrees; flexed views, a lateral view with the knee in 30 degrees; of knee flexion, and a Merchant view.9
The Merchant view is needed rather than the skyline view because as the knee is hyperflexed in the skyline view, the patella is captured by the bony anatomy of the trochlea, and subtle variations of patellar tilt or subluxation are lost at knee angles greater than 30 degrees;.1
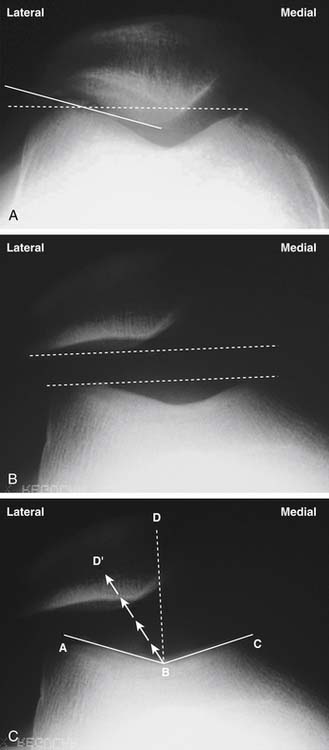
The Merchant view allows the evaluation of patellar tilt (patellofemoral angle of Laurin),10 trochlear dysplasia, and patellar subluxation (congruence angle)9 (Fig. 13-1, A–C). The lateral view allows the evaluation of patellar joint space, trochlear dysplasia, patellar alta/baja, and patellar tilt (Fig. 13-2, A–B). One can also use MRI or CT scans to measure similar angles of patellar subluxation and tilt.3,11–16
Another important measurement for malalignment of the extensor mechanism is the tibial tubercle-trochlear groove (TT-TG) measurement (Fig. 13-3). This relates how far lateral the tibial tubercle is in relation to the central portion of the trochlea.17 Normal TT-TG values are less than 10 mm, and grossly abnormal values are between 18 to 20 mm. The TT-TG can be easily measured on CT or MRI scans and should be thought of as a guide as to how far to move the tubercle during the osteotomy procedure. The final amount of anteromedialization is based on the intraoperative assessment of patellar stability.
Surgical Technique
Holding Area
Any pain blocks can be done at this time by the anesthesia service, although in order to monitor for postoperative function and the possibility of a postoperative compartment syndrome, we do not routinely use nerve blocks for this operation.
Patient Positioning
The patient is brought back to the operating room and placed supine on the operating room table.
For the arthroscopy portion of the procedure, we use a lateral post.
A tourniquet is placed at the upper thigh area, and the lower extremity is prepped and draped in the standard fashion. To avoid capturing the quadriceps with tourniquet inflation and thus altering the normal patellar tracking, the knee is hyperflexed for tourniquet inflation.
Arthroscopy
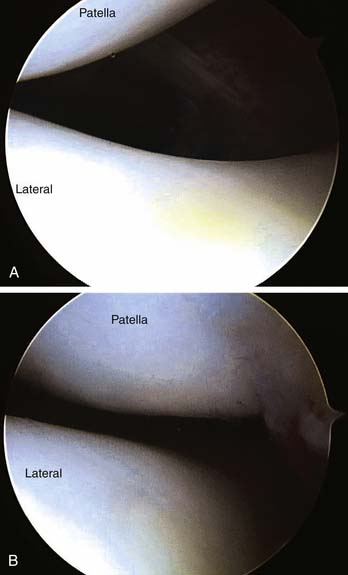
Patellar tilt and subluxation should be documented early in knee flexion (i.e., <15–20 degrees) because at greater knee flexion angles the patella is constrained by the trochlear bony anatomy, thus obscuring the patellar tilt and subluxation (Fig. 13-4, A). The other knee compartments are visualized, and any other concomitant arthroscopic surgery is performed at this time (Fig. 13-4, B).
Incision/Superficial Dissection
The arthroscope is removed but still kept sterile on the field in order to assess the postanteromedialization tibial tracking.
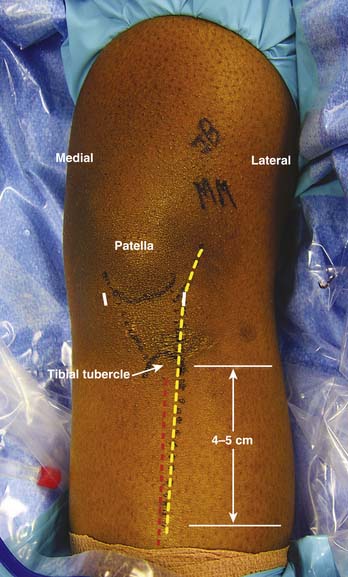
An 8 to 10 cm incision is made incorporating the inferolateral arthroscopy portal proximally and distally extending toward the tibial tubercle. The incision is kept just lateral to the anterior tibial crest to avoid having the incision over the subcutaneous bony skin. In addition, the line of the incision avoids placement of the hardware (tibial fixation screws) directly underneath the skin incision itself (Fig. 13-5). The incision is deepened down to the level of the patellar paratenon and just above the periosteum of the anteromedial tibia.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree