Chapter 12 Unloading Osteotomies
Effect on Cartilage and Cartilage Repair
Introduction
Good clinical short- and mid-term results have been reported.1–8 However, favorable results seem to be strongly dependent on a precise correction of the loading axis.9 Under-correction with persisting varus usually leads to poor results; overcorrection into large valgus may result in medial joint opening and rapid development of lateral osteoarthritis.10 Various recommendations on the precise amount of the valgus alignment achieved postoperatively have been published. Some authors refer to the anatomical axes of the femur and tibia and recommend a postoperative alignment of 8 to 10 degrees valgus.1–14 Others focus on the mechanical axes of the femur and tibia and suggest a postoperative alignment of 3 to 5 degrees valgus.5,10,15,16 However, these suggestions are based on individual clinical experiences and a few retrospective studies.
Probably the most commonly applied concept in preoperative planning is based on the work of Fujisawa et al.14 In this retrospective clinical study, preoperative and postoperative arthroscopy with a follow-up for 4 months to 6 years was performed on 54 knee joints before closing-wedge HTO, and the tibiofemoral joint cartilage was evaluated. The postoperative weight-bearing axis was correlated with changes in cartilage findings. The correction achieved postoperatively was measured with reference to the intersection of the weight-bearing axis with the tibial plateau. The tibial plateau was divided into four sections and the point of intersection assigned to the corresponding section. Fujisawa et al.14 concluded from their findings that for ideal correction the postoperative axis should lie within the lateral 30% of the tibial plateau as measured from its midpoint. From this study derived the recommendation that the weight-bearing axis should postoperatively pass through the “Fujisawa point” (i.e., it should intersect with the knee joint line at 62% of the tibial plateau width measured from its medial cortex).17–19
Effect of Different Load Axes on Tibiofemoral Cartilage
Literature
Before direct measurement of joint cartilage pressure was technically feasible, indirect methods were employed based on evaluation of radiographs, eventually combined with gait analysis and measurements of ground reaction forces with force plates.20–22
The first direct measurements of transferred joint forces and contact pressures were obtained by application of strain gauges.23,24 Next, pressure-sensitive films (Fuji film) were used that changed color as a result of applied pressure.25,26
The up-to-date techniques use pressure-sensitive film that measures changes in electromechanical resistance (K-Scan System, Tekscan, Inc., Boston, Mass.). These sensors offer the highest accuracy and best reproducibility and have provided the basis for the most recent studies on this subject.27
Most studies are tested under static conditions and rarely under dynamic conditions (i.e., simulation of gait cycle with an increase and decrease in loading). Nevertheless, all the studies were basically able to demonstrate that alterations of the axial alignment led to redistribution of load within the compartments of the tibiofemoral joint. Varus deformity resulted in greater loading of the medial compartment and valgus deformity in greater loading of the lateral compartment. This inequality in the distribution increased with the degree of axis deviation, proximity to the joint line, and amount of applied force.24,25
In addition to those studies describing tibiofemoral pressure distribution under the influence of different load axes in the frontal plane, only two experimental studies have been published that investigated the effect of high-tibial-correction osteotomy on contact pressures distributions within the knee joint. Only one of these studies was concerned with the correction of deformities in the frontal plane (valgus-varus)26; using the closing-wedge technique. The other study, published by the present author, investigated contact pressure changes after correction osteotomy in the sagittal plane.27 Measurements of the contact pressure in the knee joint after correction osteotomy in the varus-valgus plane in open-wedge technique have not been published so far. Furthermore, data correlating the degree of valgus with the desired changes in intraarticular contact pressure distribution are currently not available.
In a biomechanical study with knee joint specimens, Riegger-Krugh et al.25 investigated the effect of HTO in closing-wedge technique on the contact pressure distribution within the tibiofemoral joint. Fuji films were used for pressure measurement (i.e., only measurement under static conditions were possible and there were no repeated measurements). Both varus and valgus malalignments were simulated and a closing-wedge osteotomy of 5 degrees was carried out. The authors found differences in contact pressure distribution as expected, with higher contact pressure in the medial compartment in varus malalignment and higher contact pressure in the lateral compartment in valgus malalignment. Surprisingly, with a neutral loading axis, less contact pressure was recorded in the medial compartments than in the lateral compartments under these test conditions; after valgus HTO, the contact pressure distribution was similar to that with neutral loading axis. The authors concluded that because of those only minimal changes in the contact pressure distribution, an HTO of 5 degrees would represent in most patients an under-correction.
In a biomechanical study conducted by the authors,27 tibiofemoral contact pressure was measured after flexion HTO (i.e., after altering the mechanical axes in the sagittal plane). In a dynamic experimental model involving a knee joint kinemator, contact pressure was measured with the K-Scan System. Flexion osteotomy was performed as a supra tuberositous opening-wedge osteotomy parallel to the tibial slope of the tibial plateau, and then the tibial slope was gradually increased in 5 degrees increments from its original position to 20 degrees. This osteotomy exclusively modified the alignment in the sagittal plane; the alignment in the frontal plane (varus-valgus) was left unchanged.
Experimental Study of the Authors
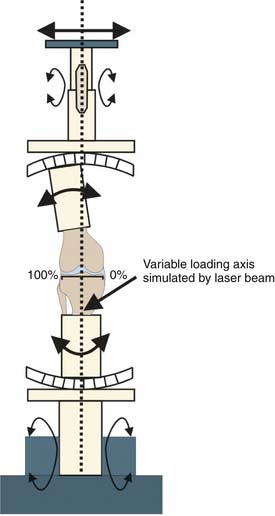
The authors conducted an experimental study to investigate the effect of different loading axes in the frontal plane on the tibiofemoral cartilage pressure.19 Seven knee joints were tested in full extension under axial loading according to a standardized loading protocol (peak load 1000 N) in a materials testing system (MTS 858 Mini Bionix II test system, Eden Prairie, Minn.). Different loading situations of the lower leg were simulated by varying the anatomical alignment angles of the distal femur and the proximal tibia as well as the offset created by the femoral head using a specially designed and constructed fixture. The fixture was allowed to compensate for different preexisting anatomical femoral and tibial angles, and a standardized and reproducible intersection between the mechanical loading axis the knee joint line was set up for each testing. The distal end of the tibia and the proximal end of the femur were potted in cylinders attached to universal joints, which allowed frontal- and sagittal-plane movement but constrained axial rotation.
The knee joint line was measured as the width of the tibial plateau and divided into percentages along its length beginning from the medial margin of the cortex (Fig. 12-1).
Accurate positioning of the load line was determined by a vertical laser beam translating the frontal plane rotation axes of the proximal and distal universal joints (Fig. 12-2). Zero percent varus alignment was defined as an offset of 0% of the width of the tibia plateau from the medial margin. Other axial alignments then tested were at 25%, 50% (neutral axis), 62% (Fujisawa point), and 75%. Subsequently, an intraligamentous opening-wedge HTO was performed in standard technique with medial approach (discussed later). The opening was standardized at 9 mm, the medial collateral ligament initially left intact, and the load axis again adjusted to 62%. Finally, the distal superficial part of the medial collateral ligament bridging the osteotomy was dissected from anterior to posterior in two stages.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree