Unicompartmental Total Knee Arthroplasty With Conventional Instrumentation
Richard D. Scott
INDICATIONS/CONTRAINDICATIONS
Unicompartmental knee arthroplasty (UKA) is an attractive alternative to proximal tibial osteotomy or tricompartmental arthroplasty in selected osteoarthritic patients with unicompartmental involvement. It should yield a higher initial success rate than osteotomy, with fewer early complications. Additionally, it is a conservative alternative to total knee arthroplasty (TKA) by preserving both cruciate ligaments, the opposite compartment, and the patellofemoral articulation.
Before proceeding with the unicompartmental arthroplasty, a decision has to be made at arthrotomy as to whether the patient is an appropriate candidate. Both cruciate ligaments should be intact, although a deficient anterior cruciate ligament (ACL) is occasionally acceptable if certain criteria
are fulfilled. (They include a tibial wear pattern that remains in the anterior two thirds of the tibial plateau. A posterior wear pattern represents an unacceptable ACL deficiency. There should be no evidence of significant medial-lateral tibiofemoral subluxation. Finally, little or no posterior slope should be applied to the tibial resection to discourage a posterior wear pattern from evolving.)
are fulfilled. (They include a tibial wear pattern that remains in the anterior two thirds of the tibial plateau. A posterior wear pattern represents an unacceptable ACL deficiency. There should be no evidence of significant medial-lateral tibiofemoral subluxation. Finally, little or no posterior slope should be applied to the tibial resection to discourage a posterior wear pattern from evolving.)
Changes no greater than grade I should be present in the opposite compartment. The patellofemoral compartment can have up to grade III changes, but the presence of eburnated bone is probably a contraindication to the procedure. A significant inflammatory synovitis is a contraindication as is the presence of crystalline disease in the form of gout or pseudogout.
Poor flexion is not an absolute contraindication to unicompartmental arthroplasty (although we prefer a minimum of 90 degrees of flexion), but poor passive extension is, if not correctable to less than 10 to 15 degrees by the procedure. A lax medial collateral ligament (MCL) is a contraindication in the valgus knee with lateral compartment involvement. If this ligament has developed more than 2 mm of laxity, it can stretch even after adequate passive correction of the deformity, causing late failure of the arthroplasty. Varus deformity greater than 10 degrees or valgus deformity greater than 15 degrees are contraindications for UKA unless passively correctable after excision of osteophytes. Finally, morbid obesity is a contraindication as well.
The technique that follows is as generic as possible regarding the implantation of a UKA. Each individual prosthetic design will have its own unique features regarding alignment, cutting jigs, and modes of prosthetic fixation such as lugs or fins.
PREOPERATIVE PLANNING
Preoperative determination of a patient’s eligibility for unicompartmental arthroplasty requires confirmation that the pain and arthritis are localized to one of the tibiofemoral compartments, based on the history, physical examination, and radiographs. Pain in another compartment of the knee would discourage unicompartmental arthroplasty and favor an alternative intervention, such as TKA. Radiographs include standing anteroposterior, midflexion posteroanterior, lateral, and sunrise radiographs.
To accomplish a conservative tibia-first preparation, the preoperative anteroposterior (AP) x-rays should be used to plan the level of the resection. A conservative resection line is drawn on the x-ray 90 degrees to the long axis of the tibia (Fig. 24-1). The level of this resection is determined on the lateral side 8 to 10 mm below the joint line. The level of the initial tibial resection should be no lower than this line whether it is for a medial or lateral compartment arthroplasty. For medial compartment
replacement, the resection begins where this line intersects with the most peripheral aspect of the plateau. For most knees, this will be somewhere between 0 and 2 mm of resection. This amount of resection makes sense when one considers that for every millimeter of elevation of the joint line from the periphery of the plateau, 1 degree of correction is obtained. Therefore, if the peripheral resection is 0 and a 7-mm tibial component is used, approximately 7 degrees of correction will be achieved. This would take a typical unicompartmental arthroplasty candidate in 3 degrees of anatomic varus back to 4 degrees of anatomic valgus (Fig. 24-2).
replacement, the resection begins where this line intersects with the most peripheral aspect of the plateau. For most knees, this will be somewhere between 0 and 2 mm of resection. This amount of resection makes sense when one considers that for every millimeter of elevation of the joint line from the periphery of the plateau, 1 degree of correction is obtained. Therefore, if the peripheral resection is 0 and a 7-mm tibial component is used, approximately 7 degrees of correction will be achieved. This would take a typical unicompartmental arthroplasty candidate in 3 degrees of anatomic varus back to 4 degrees of anatomic valgus (Fig. 24-2).
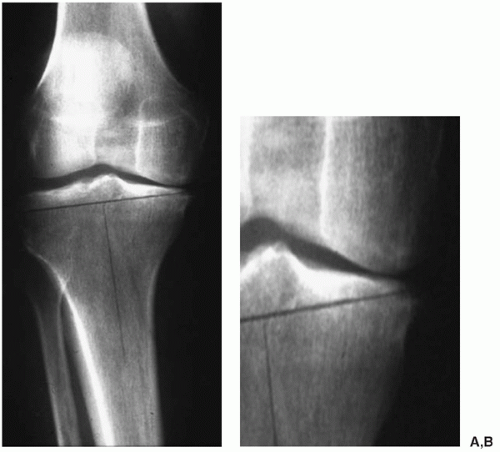 FIGURE 24-1 (A) Preoperative planning involves drawing a conservative resection for a total knee arthroplasty. (B) This represents an initial conservative medial resection. |
SURGICAL TECHNIQUE
If the prosthetic design and surgical technique remain conservative, bone is preserved in the compartment being resurfaced. My goal is to prepare a unicompartmental replacement in such a way that no augmentation methods will be necessary at the time of any future revision. The only possible deficiency would occur in a medial compartment replacement on the tibial side caused by subsidence of the tibial component. Fortunately, osteolysis compromising bone stock is extremely rare in unicompartmental arthroplasty. The following are my basic principles for unicompartmental arthroplasty.
A conservative tibia-first resection
Assessment of the resultant extension and flexion gaps
Equalization of the gaps
Distal femoral resection in the proper alignment and amount
Sizing the femur and aligning it relative to the tibia in 90 degrees of flexion
Completion of the femoral preparation
Sizing, orienting, and completing tibial preparation
Confirmation of limb alignment and component orientation with trial implantation of components
Implantation of real components
OPERATIVE EXPOSURE
Traditionally, unicompartmental arthroplasty of the medial side was carried out by a standard total knee exposure using a median parapatellar arthrotomy with complete eversion of the patella. Care would be taken not to derange the anterior horn of the lateral meniscus. This exposure gave the surgeon the opportunity to completely explore the knee and make an intra-operative decision as to whether the patient qualified for UKA.
Minimally invasive unicompartmental surgery and exposure is now popular (1). These shorter incisions can allow for a shorter hospital stay and faster recovery. They have several disadvantages,
however (2). The limited exposure does not allow a complete assessment of the opposite compartment. It also does not allow a thorough assessment of component orientation, which could lead to malpositioning of components and an increased incidence of both early and late failure of the procedure. There is also concern that the amount of stretching of the skin needed for adequate visualization can lead to an increased incidence of wound healing problems and subsequent infection. I believe that a more rapid recovery associated with minimally invasive unicompartmental arthroplasty is not as much caused by a short incision but rather from the treatment of the quadriceps mechanism. If the patella is subluxed laterally, rather than everted, rapid recovery is possible.
however (2). The limited exposure does not allow a complete assessment of the opposite compartment. It also does not allow a thorough assessment of component orientation, which could lead to malpositioning of components and an increased incidence of both early and late failure of the procedure. There is also concern that the amount of stretching of the skin needed for adequate visualization can lead to an increased incidence of wound healing problems and subsequent infection. I believe that a more rapid recovery associated with minimally invasive unicompartmental arthroplasty is not as much caused by a short incision but rather from the treatment of the quadriceps mechanism. If the patella is subluxed laterally, rather than everted, rapid recovery is possible.
I use a shorter-than-normal skin incision approximately 12 cm in length and begin the arthrotomy approximately 1 cm above the superior pole of the patella. It ends distally at the midportion of the tibial tubercle. Adequate inspection of the joint can usually be accomplished by flexing the knee 30 to 40 degrees and manually subluxing the patella. Digital palpation of the patella allows for the detection of eburnated bone on its surface. A retractor such as a bent Homan is anchored in the intercondylar notch and allows maintenance of the lateral subluxation of the patella during the procedure (Fig. 24-3).
For lateral compartment replacement, many surgeons use a short lateral arthrotomy. My concern with this approach is the fact that a formal lateral parapatellar exposure to the knee would be necessary if the UKA is abandoned for a TKA. My personal preference is to perform a standard median parapatellar approach for a valgus knee requiring lateral compartment replacement. As the arthrotomy approaches the anterior horn of the medial meniscus, the dissection is taken laterally anterior to the coronal ligament to avoid derangement of the medial meniscus (Fig. 24-4). The patella is everted and the knee flexed. Enough fat pad is removed from the anterior aspect of the tibia to expose it for the tibial resection. An incision is made at the midcoronal plane of the lateral plateau just outside the lateral meniscus for placement of a bent Homan retractor. Moist wound towels protect the subcutaneous tissue and the medial compartment throughout the remainder of the procedure.
HELPFUL ELEMENTS OF THE EXPOSURE
Before executing the bony resections, the anatomy should be defined and measures taken to protect the MCL from injury. First, the anterior third of the medial meniscus is removed. This defines an entry point between the deep MCL and the proximal tibial plateau. At this level, the surgeon inserts a curved 1-cm osteotome tangential to the plateau with half of its surface above and the other half below the level of the plateau. It is then tapped with a mallet along the border of the plateau until it reaches the level of the semimembranosus bursa. This creates a pathway for insertion of a retractor that will protect the MCL during tibial preparation.
As noted previously, a bent Homan-type of retractor is placed with its tongue in the intercondylar notch and its blade against the medial border of the patella, subluxing it laterally for adequate
exposure of the entire medial femoral condyle. If this exposure is compromised, the arthrotomy can be extended proximally for about a centimeter. Medial and lateral osteophytes are removed to define the true medial-lateral dimension of the condyle. Removal of intercondylar osteophytes relieves any potential impingement between them and the tibial spine and provides a pathway for the resection that will take place along the spine. Removal of medial osteophytes releases the MCL and allows passive correction of the deformity (3).
exposure of the entire medial femoral condyle. If this exposure is compromised, the arthrotomy can be extended proximally for about a centimeter. Medial and lateral osteophytes are removed to define the true medial-lateral dimension of the condyle. Removal of intercondylar osteophytes relieves any potential impingement between them and the tibial spine and provides a pathway for the resection that will take place along the spine. Removal of medial osteophytes releases the MCL and allows passive correction of the deformity (3).
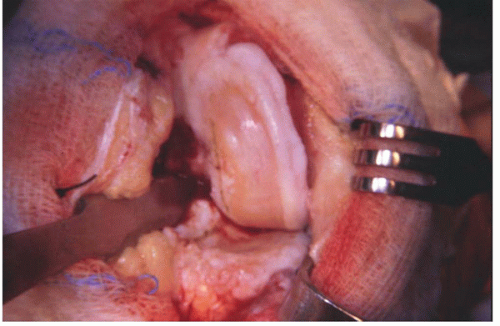 FIGURE 24-3 Excellent exposure is obtained with a short arthrotomy and lateral subluxation of the patella. |
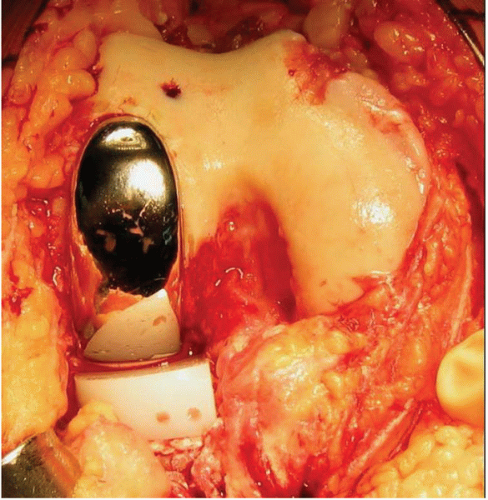 FIGURE 24-4 A medial arthrotomy with preservation of the anterior horn of the medial meniscus provides excellent exposure for a lateral arthroplasty. |
The chondro-osseous wear pattern on both the femur and tibia is defined with a marking pen or electrocautery. This gives an initial guide to the proper rotatory alignment of the femoral and tibial components (Fig. 24-5). Final rotational alignment of each is confirmed as the bone preparation proceeds.
PREPARATION OF THE TIBIA
Here, I describe the technique for an onlay type of tibial component. The same general principles of preparation apply for an inlay technique.
An external tibial alignment jig is applied with the level of resection based on the preoperative templating for conservative cut (Fig. 24-1). The varus-valgus alignment should be more or less perpendicular to the long axis of the tibia and the amount of initial posterior slope applied between 3 and 5 degrees. The exception to this amount of slope is the rare ACL-deficient knee in which posterior slope is limited to between 0 and 3 degrees.
If the alignment jig is to be stabilized by a fixation pin, I recommend that only one inboard pin should be used. Outboard pins that come close to or infract the medial cortex are associated with postoperative stress fractures as are techniques that call for the application of multiple stabilizing pins (Fig. 24-6) (4). It is important to use a narrow oscillating saw blade for this cut to avoid undercutting the tibial spine or injuring medial soft tissues.
Further protection of the medial tissues is afforded by the placement of a 1.5-cm-wide retractor into the tissue plane created by the curved 1-cm osteotome in the initial exposure (Fig. 24-7). After completion of the horizontal bone cut, a vertical cut is made along the tibial spine with a reciprocating saw that is parallel to the tibial chondro-osseous wear pattern. Removal of the medial femoral osteophyte created a pathway for the saw (Fig. 24-8). The lateral placement of this cut is, in general, halfway up the slope of the medial tibial spine. The resected tibial bone is easier to remove with the knee in extension than in flexion because there is usually cartilage remaining posteriorly on both the femur and the tibia. The resected bone can be grasped with a Kocher clamp while the knee is in flexion and then pulled free when the knee is extended. The resected piece will usually show a wear pattern that is anterior and medial (Fig. 24-9).
 FIGURE 24-5 The chondro-osseous wear pattern provides a good start for determining the rotational alignment of the components. |
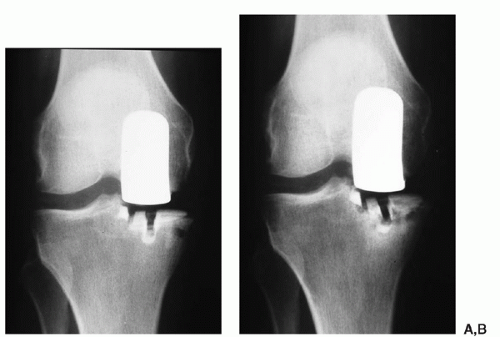 FIGURE 24-6 (A) A peripheral pinhole for an alignment jig creates a stress riser. (B) The result can be a stress fracture through the pinhole. |
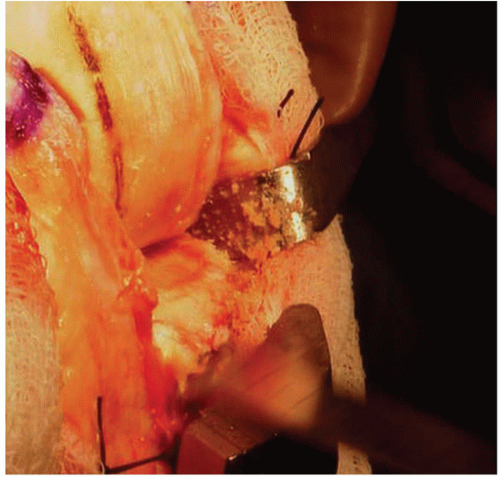 FIGURE 24-7 A well-placed retractor protects the medial collateral ligament from the saw resecting the proximal tibia. |
ASSESSMENT OF THE EXTENSION GAP
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree










