CHAPTER 24 Ultraviolet light and ultrasound
Ultraviolet light
UV light is a simple-to-use modality that may be a valuable tool in addressing wound bioburden, especially in this era of resistant organisms. Specialized lamps generate UV light. Hot quartz mercury vapor lamps produce UV-A and UV-B. Cold quartz lamps create UV-C. These lamps are generally easier to use, and treatment may be started immediately, without a warm-up or cool-down period (Figure 24-1).
UV light consists of the portion of the electromagnetic spectrum that is at a higher frequency than visible light. The wavelength ranges from 320 to 400 nm for UV-A, 290 to 320 nm for UV-B, and 185 to 290 nm for UV-C. UV light has long been used for treatment of many skin conditions, including psoriasis (Kirke et al, 2007; Lapidoth et al, 2007) and acne vulgaris. In recent decades, usage for those conditions has declined due to the advent of more topical and systemic treatments and the increased awareness of the potential damage from UV radiation. However, UV-C has seen a resurgence in the care of chronic wounds.
Physiologic effects
UV light does not heat tissue. Instead, it is believed to alter cellular function, increase cell wall permeability through altering the shape of proteins, stimulate production of various chemicals such as prostaglandins and arachidonic acid, and increase the production of adenosine triphosphate (Camp et al, 1978). The erythema that results increases local vasodilation, tissue oxygenation, and histamine release. Earlier studies using high doses of UV report increases in epithelialization and epithelial cell turnover (Freytes et al, 1965; Wills et al, 1983), increased granulation tissue growth and tissue perfusion at lower doses (Ramsay and Challoner, 1976), stimulated growth factor release (James et al, 1991), and increased autolysis (Kloth, 1995). However, these older studies used a different standard of care for comparison than exists today. Therefore, whether UV enhances wound healing in conjunction with advanced wound healing approaches is not known.
Each form of UV has different effects on tissue. UV-A and UV-B are nonionizing. They are both found environmentally, as they pass through the atmosphere. UV-A produces a mild erythema, whereas UV-B elicits a stronger erythematous response while it penetrates the epidermis. The impact of UV-A can be increased with the use of oral psoralens, a photosensitizing agent, before treatment. UV-A penetrates several millimeters into the skin, the deepest of the three forms. UV-B produces hyperplasia of the dermis and stratum corneum 3 days after treatment and has been used to toughen scars (Parrish et al, 1981).
UV-C is mutagenic but is not linked to skin cancers for several reasons: (1) UV-C only penetrates the most superficial layers of the epidermis; (2) the superficial layers of epidermis are sloughed often enough to prevent development of neoplasms; and (3) naturally occurring UV-C is blocked by the atmosphere before it reaches the earth’s surface. However, as wound treatment exposes the more permanent healing tissue, and not the epidermis, to UV-C radiation, the long-term cancer risk is unknown. UV-C is recognized to be germicidal, which has come to be the primary use for UV treatment. Other evidence suggests that UV-C can increase epithelialization, increase epithelial cell turnover (Freytes et al, 1965), increase granulation tissue growth and tissue perfusion at lower doses (Ramsay and Challoner, 1976), stimulate growth factor release (James et al, 1991), and increase autolysis (Kloth, 1995; Spielholz and Kloth, 2000).
The bacteriocidal effects of UV have been recognized for more than a century (Gates, 1928). UV-C has been demonstrated to kill methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant enterococcus (VRE) in vitro in 90 seconds (Conner-Kerr et al, 1999). The mechanism of action is theorized to be inhibition of DNA synthesis (Hall and Mount, 1981). Another in vitro study (Sheldon et al, 2005) found MRSA eradication with use of UV-C, with an even greater impact on Pseudomonas. A case series by Thai et al (2002) demonstrated reduced bacterial counts and more rapid healing with UV-C use, although treatment was not standardized and there was no control, which limit the ability to connect use of UV to the improvements observed. Thai et al (2005) later studied the effect of one 180-second UV-C treatment session on semiquantitative swab culture results of 22 patients whose chronic ulcers contained high levels of bacteria and exhibited signs of infection. Types of wounds included pressure, venous, diabetic, and arterial etiologies. Results showed a statistically significant reduction of the predominant bacteria and significant reductions of MRSA and S. aureus.
Indications and use
Because of its antimicrobial effects, UV-C is sometimes used in operating rooms in place of laminar flow to reduce surgical infections (Ritter et al, 2007). Following a systemic review, Reddy et al (2008) did not recommend UV treatment of pressure ulcers. However, international guidelines for treatment of pressure ulcers (EPUAP-NPUAP, 2009) advocate the consideration of UV-C treatment in the short term for pressure ulcers that do not respond to traditional therapies or as adjunctive therapy to reduce bioburden in clean, critically colonized Stage III and IV pressure ulcers. Pressure ulcer guideline recommendations related to UV are based on expert opinion and small in vitro and in vivo studies (Conner-Kerr et al, 1998, 1999; Thai et al, 2005). The guideline further states that UV should not be used in the absence of additional appropriate therapies due to insufficient evidence to draw definitive conclusions (EPUAP-NPUAP, 2009).
Contraindications and precautions
Safe and effective dosage of UV-C may vary based on the distance from the light source, the intensity of the light source, and the size of the treated area. UV-C has a very low risk of causing burns. Contraindications, precautions, and conditions that can be exacerbated by UV treatment (especially with UV-A or UV-B over large areas of the body) vary according to the source (Box 24-1). Conditions and medications requiring the clinician to use caution when applying UV treatment are listed in Box 24-2 (Cameron, 2008; Michlovitz and Nolan, 2005).
BOX 24-1 Contraindications and Conditions Exacerbated by Ultraviolet (UV) Light Therapy
Ultrasound
Traditional high-frequency ultrasound (1.0–3.3 mhz)
An ultrasound device consists of the control unit and the hand-held sound head, or transducer (Figure 24-2). The user is able to control the intensity (amount of power used), whether the waves are continuous or pulsed, the duration of treatment, and, on some units, the wavelength. The device runs electricity through a crystal in the sound head, causing the crystal to vibrate through a reverse piezoelectric effect. These vibrations create sound waves that pass through the sound head membrane and into the tissue. These waves elicit both thermal and nonthermal effects.
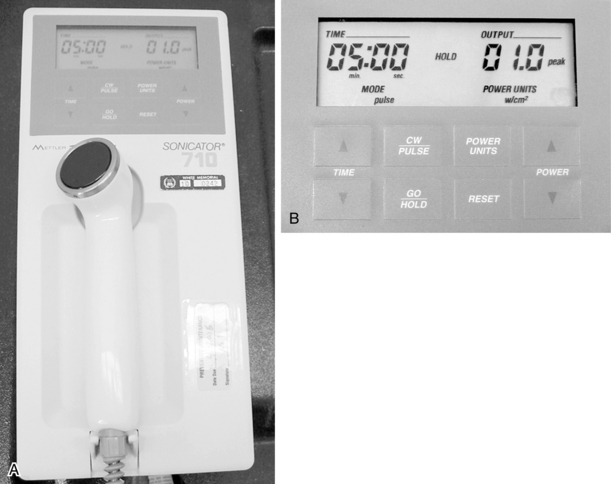
FIGURE 24-2 A, Ultrasound device. B, Close-up of ultrasound parameter settings.
(Courtesy Renee Cordrey.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









