CHAPTER 32 Burns
1. Identify the three phases of burn care and discuss the goals of each phase.
2. Discuss the causes of burns, including thermal, chemical, and electrical injuries.
3. Identify how the three zones of tissue damage relate to the depth of the burn wound.
4. Compare and contrast the severity of burn trauma using the following terminology: superficial, superficial partial-thickness, deep partial-thickness, and full-thickness burns.
5. Describe three methods commonly used to calculate the total body surface area of a burn.
6. Describe the advantages and disadvantages of at least four topical burn care products or dressings.
7. Describe the indications and techniques for escharotomy, fasciotomy, tangential excision, and skin grafting.
8. Distinguish among indicators for managing the patient with a burn in the outpatient setting, the inpatient setting, and a specialized burn care facility.
9. Identify three principles of managing burn wounds in an outpatient setting.
Beyond the patient’s physical needs, all burn team members must be aware of the psychological impact of acute injury, the phases of recovery from a burn injury, and the long-term rehabilitation needs of the patient. Throughout the United States, a number of specialized burn centers are dedicated to the management of the patient with a burn and other conditions that require care similar to burn care. In a facility that does not provide this type of specialized care, it is crucial that the wound specialist facilitate referral immediately. Box 32-1 lists the criteria for burn center referral.
BOX 32-1 Criteria for Burn Center Referral
• Partial-thickness burns >10% of total body surface area
• Burns that involve the face, hands, feet, genitalia, perineum, major joints
• Electrical burns, including lightning injury
• Presence of preexisting medical disorders that could complicate management, prolong recovery, or affect mortality
• Patients with concomitant trauma in whom the burn poses the greatest risk of morbidity or mortality
• Burned children in hospitals without qualified personnel or equipment to care for children
• Patients who require special social, emotional, or long-term rehabilitative intervention
Adapted from American Burn Association: Guidelines for the operations of burn centers, J Burn Care Rehabil 28(1):134-141, 2007.
Epidemiology
It is estimated that more than one million burn injuries occur each year in the United States, with more than 500,000 annual emergency department visits and more than 50,000 hospital admissions (American Burn Association, 2007). The majority of these injuries involve burns of less than 10% of the total body surface area (TBSA). Flame burns and scalds from hot liquids account for almost 70% of reported cases; almost half of these injuries occur in the home (American Burn Association, 2008). The National Burn Repository 2007 Report (American Burn Association, 2008), which includes data on more than 181,836 burn cases from 73 U.S. burn centers, further identifies characteristics of burn-injured patients. Nearly 70% of all burn victims are male; mean age of all reported cases is 35 years; and 12% of all burn injuries occur in children younger than 5 years and 14% in patients 60 years and older. The mortality rate for these patients is 4% to 5%.
Types of burn injury
Thermal (flame, scald, and contact)
Thermal.
Thermal burns are the most common cause of burn injuries. They result from exposure to flames, scalds from hot liquids, and contact with hot objects. The severity of injury is related to the temperature and duration of contact. Flame burns commonly involve exposure to fire, with ignition of clothing, outdoor trash, and brush fires frequently involving use of an accelerant (Wibbenmeyer et al, 2003).
House fires are another significant cause of flame burn injury and are associated with the additional risk of smoke inhalation injury. Smoke inhalation injury is present in approximately 10% to 20% of patients admitted to burn centers (Palmieri, 2007). In 2006, fire departments in the United States responded to 412,500 home fires, which resulted in 2,580 nonfirefighter deaths and 12,925 injuries. In 2005, residential fires caused nearly $7 billion in property damage (Karter, 2009). Most fatalities at fire scenes are caused by inhalation of smoke with toxic compounds (Palmieri, 2007). The combustion of household items, such as carpeting and furniture, generates a number of gases, including carbon monoxide, hydrogen cyanide, ammonia, aldehydes, sulfur dioxide, and isocyanates (Prien and Traber, 1988). Carboxyhemoglobin levels greater than 50% are often found in patients with such exposure. Administration of 100% oxygen should be initiated as soon as possible (American Burn Association, 2005).
Inhaled hot air (temperatures >150°C) causes heat injury to respiratory epithelia (Palmieri, 2007). Tissue edema can occur very rapidly to the upper airway and may cause airway obstruction. The patient with burns to the face, singed nasal and facial hair, edema of the tongue or pharynx, and increased respiratory rate should be monitored closely for airway obstruction due to edema. Intubation with mechanical ventilation may be necessary to provide adequate oxygenation until the edema resolves.
Scald.
Most scald injuries occur in the kitchen or bathroom of the home and are associated with cooking (food and grease spills) and hot water exposure (Evans et al, 2006; Lowell et al, 2008). Temperatures up to 45°C (113°F) may be tolerated for relatively long periods without injury, but as few as 10 seconds of exposure to water at 70°C can result in full-thickness injury in adults (Carrougher, 1997; Jordan and Harrington, 1997). At the temperature of most home water heaters (60°C [140°F]), tissue destruction in a child can occur in less than 5 seconds; only 1 second in an infant (Helvig, 1993).
Contact.
Contact burns can occur in the home or in the workplace. They frequently occur on the hands, face, and upper body as the object is touched. Common causes of contact burns include oven doors, fireplace screens, space heaters, clothing and curling irons, cookware, and hot machinery and containers (Alden et al, 2006; Hunt et al, 2000; Wibbenmeyer et al, 2003). Children younger than 5 years are at particular risk for scald and contact injuries due to a limited ability to recognize and respond appropriately to danger. The elderly have predisposing factors associated with age that put them at risk for burn injury, including reduced reaction times, decreased dexterity, decreased mobility, inaccurate risk assessment, and impaired senses (Redlick et al, 2002). Working adults are at risk for scald and contact burns; exposure to hot objects or substances are the second leading cause of burn injury in the workplace (Hunt et al, 2000).
Electrical
Electrical injuries account for 4% of burn center admissions (American Burn Association, 2008). It is estimated that as many as 50,000 injuries and 1,000 deaths from electrical causes occur each year in the United States. The American Burn Association (2005) estimates that the risk of being struck by lightning is 1:280,000; lightning injuries kill 80 to 100 people in the United States every year. Tissue injury results when electrical energy is converted into thermal or heat energy. The extent of injury to the body when it becomes part of an electrical current is determined by the (1) strength and type of current, (2) pathway of flow, (3) local tissue resistance, and (4) duration of exposure (American Burn Association, 2005). Various tissues of the body have different resistances to current flow; once electrical contact is made with the skin and resistance is overcome, the body acts as a volume conductor as current flows through the body part (Luce, 2000). Bone has a very high resistance, which allows current to flow along the surface of the bone. Adjacent deep muscle tissue is damaged while superficial muscle and the skin surface remain viable.
Classification of electrical injuries is divided into four categories: high voltage (>1,000 V), low voltage (<1,000 V), lightning strikes, and electric arc without passage of current through the body. The highest incidence of injuries are work related and high voltage, with the primary victims being young men (Arnoldo et al, 2004). Electrical injuries in children are generally low voltage, occur in the home, and involve contact with electrical appliances or frayed cords or placement of objects into electrical outlets. Because of the mechanism of injury, electrically injured patients are at risk for concomitant blunt trauma, soft tissue injuries, and thermal (flame or flash) burns (American Burn Association, 2005). Electrical injuries may also result in potentially fatal cardiac dysrhythmias. Practice guidelines for the management of electrical injuries recommend an electrocardiogram be performed on all patients who sustain either high- or low-voltage electrical injuries (Arnoldo et al, 2006).
Chemical (alkalis, acids, and organic compounds)
Chemical burns account for 3% of burn unit admissions (American Burn Association, 2008), with approximately 60,000 people seeking medical treatment each year. Chemical injuries often are smaller in size than thermal burns but are more likely to be full thickness in depth (Winfree and Barillo, 1997).
The severity of chemical burns is related to the agent of exposure, duration of contact, and agent’s concentration, volume, and mechanism of action. Tissue damage continues after initial exposure until the chemical is removed or inactivated (diluted) with irrigation. In general, neutralization of the agent with another chemical is not recommended unless the exact mechanism is known because the reaction may generate more heat and result in further tissue destruction (American Burn Association, 2005). Health care providers must protect themselves from exposure by using universal precautions and eye protection while caring for the chemical-injured patient. The American Burn Association (2005) identifies the common causes of chemical injury as alkalis, acids, and organic compounds.
Alkalis are commonly found in oven and drain cleaners, fertilizers, industrial cleaners, and cement and concrete. Alkalis damage tissue by liquefaction necrosis and protein denaturation, which allows for deeper spread of the chemical into tissues and a more severe injury. Acids are found in bathroom cleansers, rust removers, acidifiers for home swimming pools, and industrial drain cleaners. Acids damage tissue by coagulation necrosis and protein precipitation, which usually limits the depth and spread of tissue damage (Winfree and Barillo, 1997). Organic compounds, such as phenols and petroleum products (gasoline, diesel fuel, and creosote), can be responsible for systemic toxicity as well as contact chemical burns. Organic compounds cause cutaneous damage as a result of their fat solvent action and, once absorbed, can produce toxic effects on the pulmonary, renal, and hepatic systems (American Burn Association, 2005).
Health care providers must have a high degree of suspicion of lower airway injury related to inhalation of noxious chemicals that are products of combustion (Monafo, 1996). Chemical inhalation may cause sloughing of the airway-lining epithelium, mucus secretion, inflammation, atelectasis, and airway obstruction. Clinical evolution is delayed from 1 to 3 days after exposure (Palmieri, 2007). Treatment requires ventilatory support, meticulous pulmonary toilet, and general critical care management.
Evaluation of burn injury
Zones of tissue damage
Determining burn depth can be difficult for even the most experienced burn care provider. Immediately following injury, burns may appear superficial but declare themselves to be deeper by post-burn day 3 (Gibran and Heimbach, 2000). The phrase zones of tissue damage describes the extent of the injury from the deepest or most severely damaged area to the superficial or outermost area. The three zones of tissue damage are zone of coagulation, zone of stasis, and zone of hyperemia (Jackson, 1953). The zone of coagulation is the area of greatest damage, is closest to the heat source, and is characterized by coagulation of cells. The zone of stasis surrounds the zone of coagulation and involves the vascular system in the area. Thrombosis and vasoconstriction cause transient dermal ischemia. Circulation will return if the area is adequately perfused and protected from further damage from infection, desiccation, and mechanical stress during transfers and repositioning. The zone of hyperemia is the outermost area. Usually no cellular death occurs because this area is only minimally damaged. Cells in this zone recover in 7 to 10 days. The area is reddened because of vasodilation and inflammation. The zone of hyperemia is similar to a superficial partial-thickness burn.
Severity of the burn wound
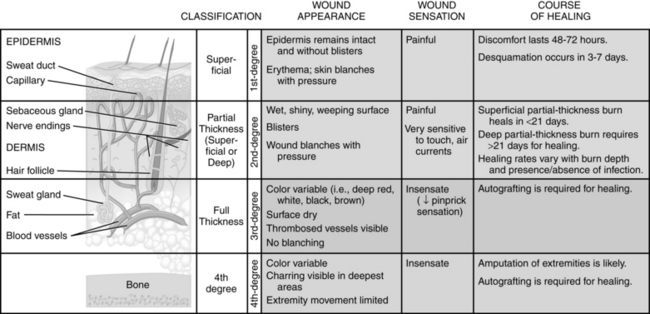
Treatment of the burn wound is based on the depth, extent, and severity of the injury. The depth of the injury is based on the number of cells injured or destroyed. With the exception of the fourth degree, the traditional classification of burns as first, second, and third degree has largely been replaced by the more descriptive designations of superficial, superficial partial-thickness, deep partial-thickness, and full-thickness injury (Figure 32-1). Most burns are not uniform in depth; the edges may be more shallow than the central aspect. The severity of the burn can deteriorate in certain circumstances and become more severe, a process known as wound conversion. Risk factors for wound conversion are similar to factors that impair other acute and chronic wounds (e.g., oxygenation, infection, mechanical trauma, malnutrition).
Calculation of body surface area burned
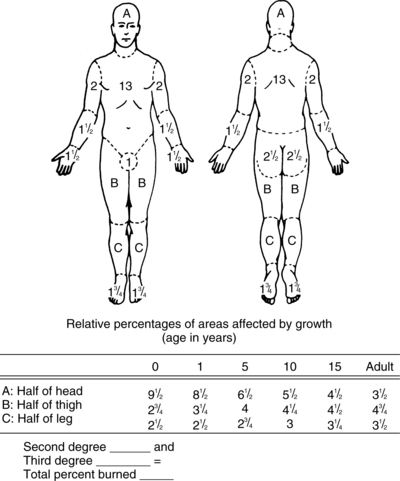
Three methods are used to determine the extent of a burn injury: (1) Lund-Browder chart (Figure 32-2), (2) rule of nines, and (3) hand method. The Lund-Browder chart is the most accurate method for estimating burn extent in patients of all ages (Mertens et al, 1997). The Lund-Browder chart is completed at admission to determine fluid requirements and is repeated after 72 hours to recalculate any areas of burn injury that may have extended. The rule of nines is based on 11 anatomic regions of the body representing 9% (or multiples of 9%) of TBSA. The rule of nines must be modified for use in children because it does not accurately reflect body surface area in children younger than 15 years (Deitch and Rutan, 2000). The hand method of determining the extent of a burn injury is useful for estimating small, scattered burns. The patient’s hand, including the fingers, represents approximately 1% of TBSA (American Burn Association, 2005). The TBSA burned is expressed as a percentage and helps estimate the extent of the injury for diagnosis, treatment, prognosis, and statistical analysis.
Referral criteria
The American Burn Association has categorized burns as minor, moderate, and major (Table 32-1) and has defined the criteria for burn center referral (see Box 32-1). Patients with major burn injuries or those who meet the criteria identified in Box 32-1 require treatment in a specialized center. A burn center is a facility with a burn physician as director and a highly trained, multidisciplinary staff dedicated to caring for the patient with burns (American Burn Association, 2007).
TABLE 32-1 American Burn Association Categories of Burn Injury
| Minor Burns | Moderate Burns | Major Burns |
|---|---|---|
| Adults: 15% TBSA | Adults: 15%–25% TBSA, mixed partial/full thickness | All patients: >25% TBSA |
| Children and elderly: 10% TBSA | Children <10 years or adults >40 years: 10%–20% TBSA | Children <10 years or adults >40 years: 20% TBSA |
| <2% TBSA full-thickness burns not involving cosmetic or functional risk or impairment of face, ears, eyes, feet, hands, perineum | < 10% TBSA full-thickness burns not involving cosmetic or functional risk or impairment of the face, ears, eyes, feet, hands, perineum | >10% TBSA full-thickness burns |
| All burns of face, eyes, ears, hands, or perineum, especially if functional or cosmetic impairment exists | ||
| All high-voltage electrical burns | ||
| All burns with inhalation injury or major trauma | ||
| Poor-risk patients |
TBSA, Total body surface area.
Pathophysiology of burn injury on the body
Inflammatory mediators released from the damaged cells at the site of the burn (e.g., arachidonic acid metabolites, oxidants, histamine, serotonin, kinins, other vasoactive amines) cause increased capillary permeability not only at the site of injury but throughout the body (Ahrns, 2004; Jordan and Harrington, 1997). Although capillary permeability returns to normal roughly 18 to 24 hours after injury, the initial body response is a dramatic outpouring of fluids, electrolytes, and protein into the interstitial space, which creates intravascular volume deficits. The release of fluids through the hyperpermeable capillaries and the increased capillary pressure combine to create local or systemic edema. The body responds with a classic hemodynamic response: an almost immediate fall in cardiac output, metabolic rate, oxygen consumption, and blood pressure, along with ongoing fluid imbalance and cellular shock, for 3 to 7 days. In patients with a burn wound of at least 15% to 20% TBSA, hypovolemic shock develops quickly unless interventions are started (Lim et al, 1998).
The fluid and electrolyte imbalance that immediately results following a burn injury dominates post-burn care priorities and poses potential complications to the pulmonary, cardiovascular, and renal systems. The shift of protein from the intracellular space and vascular compartment into the interstitial space causes numerous potential complications, such as edema, pulmonary edema, blister formation, weeping of fluid, hypovolemia, hypoproteinemia, tachycardia, increased capillary pressure, vasoconstriction of the microcirculation, decreased central venous pressure, and decreased urinary output. Sodium, magnesium, calcium, and phosphorus loss can occur directly through open burn wounds (Supple, 2004). Potassium is released from damaged cells, triggering hyperkalemia and metabolic acidosis.
Loss of skin integrity causes increased fluid and heat loss through the wound. Evaporative fluid loss caused by loss of skin integrity is 4 to 20 times the normal rate, which contributes to hypovolemia; this fluid loss continues until all the wounds are closed. Hypothermia should be prevented rigorously throughout the phases of recovery. The patient with burn injury has an increased thermal neutral point so that exposure to low temperatures results in an increase in the patient’s metabolic rate (Jordan and Harrington, 1997). Restoration and maintenance of intravascular volume with fluid similar to that which is lost in the tissues are essential aspects of burn management.
Patients with burn injuries of 20% or greater TBSA will experience a hypermetabolic response with elevated catecholamine, glucocorticoid, and glucagon levels and decreased insulin level requiring nutritional support for optimal recovery (Mertens et al, 1997). The increase in metabolic rate causes an increase in protein catabolism, gluconeogenesis, and lipolysis. This response is characterized by increased heat loss, negative nitrogen balance, and weight loss (Carrougher, 1997). The severity and duration of hypermetabolic activity are directly proportional to the extent of injury. The peak occurs in the first 2 weeks and slowly returns to normal with closure of the wound. Elevated catecholamines, decreased bowel perfusion, and increased gastric secretions place the burn patient at risk for paralytic ileus, intestinal mucosal atrophy, decreased nutrient absorption, Curling stress ulcer (Supple, 2004), and impaired ability to function as a bacterial barrier (Rutan TC, 1998).
Phases of burn care
Emergent phase
As with any trauma victim, the initial assessment of the patient with a burn injury includes the primary and secondary surveys. The primary survey (conducted out in the field) includes advanced burn life support as outlined by the American College of Surgeons Committee on Trauma (American Burn Association, 2005). The guidelines include the ABCDE assessment: airway, breathing, circulation, disability, and exposure and evaluation.
The secondary survey is initiated after immediate resuscitative measures are established and includes a complete physical assessment and medical history. Because care is based on the mechanism, location, and severity of the injury, as much information as possible regarding the incident should be obtained, such as whether the injury occurred in an enclosed space, chemicals were involved, and the victim lost consciousness. Aspects of the patient’s medical history (e.g., preexisting disease, medications, allergies, alcohol or drug use, immunization status) influence management decisions (American Burn Association, 2005).
Care during the emergent phase centers on emergency management and stabilization and on wound assessment/diagnosis. The first 24 hours is devoted to fluid resuscitation, ventilatory management, and establishing the hemodynamic stability of the patient. During this phase, the depth and extent of the wound are estimated in order to calculate the severity of the injury and fluid resuscitation needs. For a small burn (see Table 32-1), the development of edema is immediate, rapid, limited to the wound site, and peaks within 8 to 12 hours (Ahrns, 1999). Intravascular fluid losses associated with small burns can be managed with oral replacement at 150% of calculated maintenance rate. Intravenous supplementation can be used if the patient has difficulties meeting the oral intake goal.
Large burns reach maximum edema within 12 to 24 hours postinjury. The goal of fluid resuscitation is to maintain adequate tissue and vital organ perfusion while preventing complications associated with inadequate or excessive fluid therapy (American Burn Association, 2005). If fluid resuscitation is inadequate, hypovolemia will progress and acute renal failure will occur. The amount of fluid for replacement depends on the extent and depth of the burn and the patient’s age and medical history. Many fluid resuscitation formulas exist, and most are based on the percent of TBSA burned, body weight, or a combination of both. According to the American Burn Association, fluid resuscitation, regardless of solution type or estimated need, should be titrated to maintain urine output of approximately 0.5 to 1.0 ml/kg/hr in adults and 1.0 to 1.5 ml/kg/hr in children. Increased volume requirements can be anticipated in patients with full-thickness injury, inhalation injury, and delay in resuscitation (Pham et al, 2008). Adequacy of resuscitation is determined by urinary output, mental status, peripheral temperature, systolic blood pressure, heart rate, and base deficit (Sheridan, 2002).
Early initiation of enteral feeding is recommended for nutritional support of the patient with a burn (Gottschlich et al, 2002; McDonald et al, 1991; Raff et al, 1997a and 1997b) to prevent stress ulcers, increase intestinal blood flow, preserve gastrointestinal function, and minimize bacterial translocation from the gut as a result of mucosal atrophy (Andel et al, 2001; Raff et al 1997a and 1997b; Supple, 2004). The parenteral route has no clear advantage and is used only in patients with prolonged ileus or selected patients on mechanical ventilation (Tassiopoulos, 1999).
Nearly all burn centers report supplementing vitamins and/or minerals (Graves et al, 2009). Dosage guidelines established by the National Advisory Group/American Medical Association are appropriate for burn-injured patients unless symptoms of deficiency occur. Because zinc deficiencies are well documented in burn-injured patients, supplemental zinc as well as vitamin C often are required (Sicoutris and Holmes, 2006). Nutrition assessment and support is discussed in great detail in Chapter 27.
Wound stabilization.
Wound intervention during the emergent phase involves cleansing, debridement, and prevention of obstructed blood flow from edema and eschar formation. The usual burn wound care given during this period follows patient stabilization and involves cleansing the areas with a nonirritating detergent and rinsing with warm water. The environment should be warmed to prevent hypothermia. Loose necrotic or devitalized tissue is lightly debrided, and large intact bullae (>2 cm) are opened. Small, frequent doses of intravenous analgesics are provided for pain control. Full-thickness wounds usually are dressed with a topical antimicrobial agent; systemic prophylactic antibiotics are not routinely used unless specific organisms have been identified (Jordan and Harrington, 1997).
Escharotomy.
Deep partial-thickness or full-thickness burns that are circumferential, or nearly circumferential, to an extremity may require an escharotomy to relieve pressure. Edema and eschar formation can obstruct venous return and lead to decreased arterial blood flow. Early identification of extremities at risk and serial examination are essential; monitoring should include temperature, pliability, voluntary motion, pain with passive motion, changes in the quality of pulses, and delayed capillary refill. The escharotomy is a linear incision through the full-thickness wound dividing the eschar. The incision is only as deep as necessary to separate the eschar. Full-thickness eschar lacks nerve endings, so pain is minimal, although small doses of narcotics and anxiolytics are given intravenously to control background pain and anxiety. This procedure can be done at the bedside with a sterile field and scalpel or electrocautery to control the small amount of bleeding that occurs (Jordan and Harrington, 1997). Midmedial and midlateral incisions are designed to completely section the eschar while preventing injury to underlying superficial structures. The structures most at risk during escharotomy are the brachial artery in the upper arm, the ulnar nerve at the elbow, the superficial peroneal nerve at the knee, and the neurovascular bundles and extensors of the digits (Sheridan, 2002). The escharotomy incision wounds are dressed with a topical agent.
Similarly, deep circumferential burns to the chest and/or abdomen may restrict the expansion needed for breathing and adequate ventilation. Frequent assessment of the adequacy of chest expansion, quality of respirations, oxygenation, and mental status of the patient is essential. Circumferential chest burns require an escharotomy placed in the anterior axillary line bilaterally. If there is significant extension of the burn onto the adjacent abdominal wall, the incisions should be extended to this area and connected by a transverse incision along the costal margin (American Burn Association, 2005).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree