CHAPTER 31 Traumatic wounds: bullets, blasts, and vehicle crashes
Traumatic wounds result from any foreign body impact that results in tissue damage. Their etiology can vary widely: bullet or projectile wounds, blasts, industrial accidents, falls, and car crashes. Modern care for the trauma patient has its origins in military medicine. Practices developed to treat war injuries have been modified and refined to address civilian trauma. War injuries tend to be exaggerations of civilian injuries. For example, an M16 or AK-47 round causes significantly more damage than a 22 and 45 round, even though the mechanism is largely the same. For this reason, this chapter emphasizes treatment of war wounds. Although the severity of injury may be different, the principles guiding wound care remain the same. Box 31-1 lists the components of traumatic wound care.
BOX 31-1 Components of Traumatic Wound Care
• Stabilization of injured patient via acute trauma life support (ATLS) protocol is first step in traumatic wound care.
• Wound treatment is same regardless of etiology, although etiology may help practitioner discover concurrent occult injuries.
• Blood vessels, nerves, and bones must be covered with soft tissue if exposed in a wound to prevent further injury.
• Surgical debridement, low-to-intermediate pressure pulsatile lavage irrigation, and negative pressure therapy using vacuum-assisted closure repeated every 48–72 hours until wound closure or coverage are the hallmarks of traumatic wound care.
• Negative pressure dressings facilitate healing, decrease patient stress, and reduce provider time commitments.
• Optimizing the wound base includes reducing bacterial load and improving blood supply.
• Wound closure may occur through a variety of techniques based on size and location. Techniques for soft tissue wounds include: primary closure, secondary intention, muscle and fasciocutaneous flaps, skin grafting, and skin substitutes.
• Techniques to close open abdominal wounds (used alone or in combination): primary fascial closure, delayed fascial closure, component separation, planned ventral hernia, and serial abdominal closure.
• Systemic disease, the inflammatory response, and poor nutrition adversely affect wound closure; normalization of physiology, provision of adequate nutrition, and treatment of local or systemic infection are integral parts of wound healing.
• Chronic wounds are treated by converting the wound to an acute wound and treating it accordingly.
• Amputation is necessary for limb injuries when limb salvage is impossible, treatment of life-threatening injuries precludes prompt treatment of severe limb injuries, and limb ischemia time exceeds 6 hours.
• Tetanus vaccination should be standard practice for all patients with traumatic wounds.
Etiology of war wounds
Weapon-related injuries are of two basic types: those resulting from small arms fire and those resulting from explosive munitions. Small arms fire includes pistols, rifles, and machine guns. Explosive munitions include mines, grenades, mortars, missiles, bombs, and improvised explosive devices (IEDs). Regardless of the mechanism of injury, extremity wounds have compromised the majority of wounds among U.S. and U.K. soldiers since World War I, followed by head and neck, thoracic, and abdominal injuries (Burris et al, 2004).
Bullet wounds
Upon contact with tissue, a projectile creates two cavities: a permanent cavity and a temporary cavity. The temporary cavity is much larger than the permanent cavity. Elastic tissue such as muscle, fat, and connective tissue will expand and rebound, leaving only the permanent cavity. Nonelastic tissue, such as bone, will fracture secondary to the temporary cavity (Burris et al, 2004).
Further damage is caused by two additional aspects of bullets. When traveling through tissue, bullets fragment after several centimeters. This increases the diameter of the injured tissue beyond the diameter of the bullet. Bullets also yaw, or tumble. When in contact with tissue, bullets rotate 180 degrees. This tumbling greatly increases the damage by a round. Bullets that yaw earlier cause more damage. Higher-velocity bullets cause more damage than lower-velocity rounds, but yaw and fragmentation more heavily influence the amount of damage inflicted (Burris et al, 2004). Common misconceptions regarding bullets are that bullets yaw in flight, that bullets with a full metal jacket do not fragment, and that exit wounds are larger than entrance wounds.
Explosive munitions (ballistic, blast, and thermal)
Explosive munitions come in a large variety and inflict damage in multiple ways. The three types of damage inflicted by most explosive munitions are ballistic, blast, and thermal. Depending on a person’s distance from an explosion, they can be exposed to any or all of these elements.
Blast injuries are caused by the sonic shockwave produced by the explosion. The shockwave typically has a much smaller range than ballistic damage. As with bullets, the shockwave can inflict damage to hollow organs. Explosions produce a much larger shockwave than bullets. Therefore, injuries resulting from a body being thrown against an object are much more common. Thermobaric devices are designed to cause much larger shockwaves. During the initial explosion, these devices disperse a volatile substance such as fuel vapor. The fuel vapor then ignites and produces a longer and more powerful secondary explosion. This technology is frequently used in “bunker-busting” devices (Buchanon, 2006).
Several types of antiarmor devices exist. A shaped charge is designed to direct an explosion at a target. People in an armored vehicle can be injured by two types of fragments: fragments from the charge and spall, which is debris knocked off the armor plating. Some vehicle interiors are coated with Teflon as an antispall liner. Teflon can burn and produce toxic fumes if the thermal damage from the explosion is significant. Rocket-propelled grenades (RPGs) and tube-launched, optically tracked, wire-guided (TOW) missiles are two types of shaped charges. An explosively formed projectile (EFP) is a specialized shaped charge that is commonly used by insurgents in Iraq. Kinetic energy rounds are aerodynamically shaped pieces of metal, usually depleted uranium or tungsten. Depleted uranium has a hypothetical risk of heavy metal toxicity, but the risks surrounding fragment removal exceed the risk of heavy metal toxicity, so removal is not recommended (Buchanon, 2006). Two common types of kinetic energy rounds are armor-piercing, fin-stabilized, discarding sabots (APFSDS) and high-explosive, antitank (HEAT) shells. Antitank mines are similar to land mines except the former are more powerful and are designed to disable vehicles. In Iraq and Afghanistan, the most common antitank mine is the IED or roadside bomb.
Vehicle crashes
Vehicle crashes are yet another type of injury. Although some soft tissue injury may be due to penetrating trauma, much of the damage sustained is due to blunt trauma. Closed head injuries, fractures, cardiac contusions, pneumothoraces, spinal cord injuries, and spleen and liver injuries typically result from blunt trauma. Most of these blunt injuries are deceleration injuries. Organs in hollow cavities (brain, heart, abdominal viscera) are injured by contacting soft tissue or shearing off of ligaments and vessels. Traumatic brain injury and traumatic aortic rupture are two frequently fatal deceleration injuries. Crush injuries may result when a patient is trapped in a vehicle following a crash. The lower extremities and pelvis are particularly vulnerable in car crashes.
Acute management of traumatic wounds
Advanced trauma life support
Control of bleeding.
Tourniquet use comes at a price, however. When applied, hypoperfusion and subsequent ischemia occur to all tissue distal to the point of compression. Prolonged tourniquet use (as short as 90 minutes) can result in ischemia, compartment syndrome, and nerve damage. Use for more than 6 hours can result in limb loss (Beekley et al, 2008; Kam et al, 2001). Therefore, tourniquet use is traditionally not recommended for civilian extremity trauma in the United States. Traumatic hemorrhage typically requires definitive surgical correction.
However, in a combat theater, multiple factors may lead to delayed casualty evacuation. Environmental (e.g., sandstorms), geographic (e.g., mountain ranges), and tactical (e.g., ongoing combat) factors can delay evacuation for hours, if not days. Among combat fatalities, 30% to 40% result from hemorrhage (Perkins et al, 2008). In patients who are not killed immediately, hemorrhage is the most preventable cause of death. ATLS protocol should be followed as strictly as field capabilities allow. Placement of a tourniquet can temporarily halt bleeding, allowing perfusion of crucial organs and survival until an adequate surgical facility can be reached. Recent research derived from U.S. experiences in Iraq and Afghanistan suggests tourniquets are safe and limb loss is low when tourniquets are applied judiciously (Beekley et al, 2008; Kragh et al, 2009).
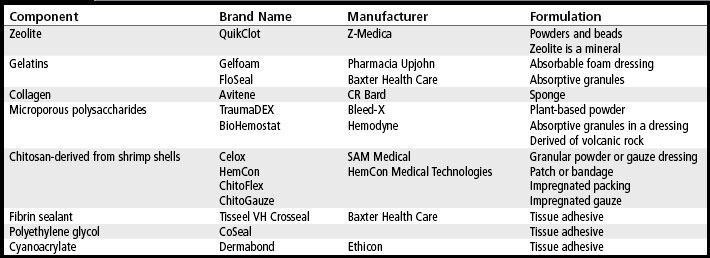
Upon the patient’s arrival to an operating room, tourniquets should be removed and the patient’s wounds explored for sites of bleeding. Blind clamping of vessels can lead to ischemia of healthy tissue and therefore should be avoided. Damaged vessels can be addressed with ligation or graft repair depending on the structure and degree of collateral flow. If external bleeding occurs where a tourniquet cannot be applied (e.g., axial areas) or if a tourniquet inadequately stops hemorrhage, a hemostatic dressing can be applied. Table 31-1 lists examples and descriptions of hemostatic agents and dressings (Kozen et al, 2008; Neuffer et al, 2004; Perkins et al, 2008; Pusateri et al, 2003; Rhee et al, 2008).
Immunization
Once a patient has been stabilized, tetanus prophylaxis should be administered. Tetanus, a disease characterized by intense muscle contractions and autonomic dysfunction, is caused by a toxin produced by the anaerobic bacteria Clostridium tetani. These contractions can be fatal if they affect the diaphragm (Wood, 2004). Wounds necessitating tetanus prophylaxis include wounds older than 6 hours, those with significant contamination or associated necrotic or ischemic tissue, puncture wounds, stab and gunshot wounds, and wounds resulting from burns or frostbite (Wood, 2004). Patients who were immunized within the last 5 years or have received a tetanus booster during this time period may be exempt. Due to the significant contamination of war wounds and the difficulties in verifying medical records in a combat environment, many trauma surgeons recommend immunizing all wounded patients (Anaya and Dellinger, 2007).
Coverage and repair of vital structures
There are three types of nerve injury. Neuropraxia, the most minor nerve injury, is a conduction block of the nerve. These injuries are common in blunt trauma and compartment syndrome. Function lost secondary to neuropraxia usually returns in 3 months. Axonotmesis is an intermediate injury to the nerve that results from damage to the axon. The surrounding endoneurium and perineurium remain intact. The damaged axon will undergo wallerian degeneration (degeneration of axon distal to the injury) but then slowly grow back (about 1 cm/month). Most function will return following this type of injury. Both neuropraxia and axonotmesis will heal without specific intervention. The most severe type of nerve injury is neurotmesis, or complete transaction of the nerve. If the injury is secondary to penetrating trauma, it usually can be repaired. Neurotmesis secondary to gunshot wounds have a less favorable outcome. The gunshot wound results in thermal and shockwave injuries in addition to the penetrating injury, making functional recovery after surgical repair less likely. Optimally, a nerve should be repaired with a tension-free anastomosis. If this cannot be done because of a substantial defect in the nerve, grafting can be attempted. Autologous nerve grafting, usually using a patient’s sural nerve as the donor, is the most common technique. Autologous vein grafts also can be used to guide regenerating nerves over defects. The timing of nerve repair depends on the degree of contamination and the need for subsequent operations to the same wound. Regardless of the degree of injury, an exposed nerve should be covered with soft tissue (Peterson and Lehman, 2008). The exposed nerve is at higher risk for infection and iatrogenic injury during subsequent surgery. A nerve that is allowed to heal without soft tissue coverage becomes highly susceptible to even minor blunt trauma.
Traumatic wounds may contain open fractures that need to be reduced and stabilized. Open fractures are at risk for infection, bleeding, increased soft tissue damage, delayed union, and nonunion. Bone infections (osteomyelitis) are difficult to treat because of the density of the bone and the paucity of adjacent blood vessels supplying the cortical bone. After the wound is irrigated and debrided, open fractures are stabilized, either temporarily or definitively. Depending on the fractured bone, fixation can be achieved by a variety of methods, most commonly screw and/or plate fixation for periarticular fractures and intramedullary nails or external fixators for diaphyseal fractures. After fixation, open fractures require soft tissue coverage with either local tissue or transferred flaps. This typically is performed at a subsequent, definitive operation. Because coverage often cannot be performed at the initial operation due to contamination, infection, or physiologic reasons, a sterile dressing is placed over the bone until a later time when surgery can be performed under more favorable conditions (Smith et al, 2008).
A wound should be explored for exposed traumatized blood vessels. Similar to nerves, exposed vessels are at risk for infection and iatrogenic injury during subsequent operations. Furthermore, any compromise to the blood supply compromises all the tissue it supplies. Medium and large arteries that supply an area of soft tissue without adequate collateral flow require repair around the time of injury. Examples include the superficial femoral, common femoral, and brachial arteries. Due to the presence of collateral veins, most major veins can be ligated following injury. If needed, repair can be performed using a variety of techniques, depending on the vessel and degree of injury. Most exposed vessels in open wounds will occur in the extremities. Repair of these vessels is by autologous or prosthetic graft. In the acute setting, a patient may be too unstable to tolerate a long operation. If this is the case and the patient has a large defect to a vessel supplying a limb, a temporary vascular shunt can be placed to maintain blood flow to the limb until definitive vascular repair can be achieved. Once a patient is able to tolerate a longer operation, the injured vessel should be repaired with an autologous vein graft, typically the saphenous vein, or an artificial conduit such as polytetrafluoroethylene. In most cases an autologous vein graft is preferred over an artificial graft because of superior patency rates. Next, consideration should be given to coverage of the exposed vessel. In addition to the risks of infection and iatrogenic injury, vessel walls will desiccate, erode, and possibly disrupt if wounds are allowed to heal without coverage. Coverage of a blood vessel can be provided by myocutaneous flap or fasciocutaneous flap. When the wound is too large for flap coverage or is too contaminated for a viable flap, an extraanatomic bypass of the injured vessel should be performed, directing a graft to route the blood vessel around the wound in an uninjured tissue plane. When an injured vessel is being repaired, the graft should be similarly routed through uninjured well-perfused tissue planes (Frykberg and Schinco, 2008).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree