Ulnar Longitudinal Deficiency
CASE PRESENTATION
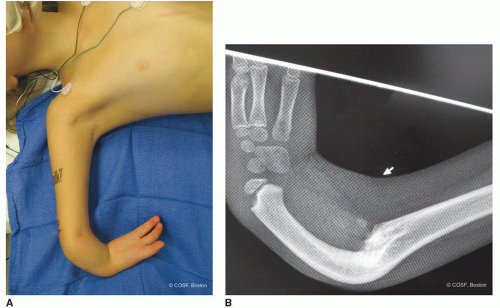
A 12-month-old male child presents with ulnar longitudinal deficiency for second opinion and potential care. He has no associated medical conditions. There is no family history of any congenital differences. He has a three-digit hand. His thumb is in the same plane as the other two digits (Figure 14-1A). His index finger has limited passive and active motion. His long finger has near full active and passive motion. His small and ring finger rays are absent. He has an extreme internal rotation posture to his affected upper limb with no elbow motion (Figure 14-1B). He has moderate wrist motion with a nonprogressive ulnar deviation posture according to his parents and outside records. The issue is whether there is an operation that can improve his function.
CLINICAL QUESTIONS
What are the characteristic anatomic features of ulnar longitudinal deficiency?
What are the associated conditions with ulnar longitudinal deficiency?
How is ulnar longitudinal deficiency classified?
What are the common operative interventions for ulnar club hand?
What are the expected long-term outcomes by natural history and surgery?
What are the present limitations to surgical care for these children?
THE FUNDAMENTALS
From the functional viewpoint, the deformed limb is much more useful than its anatomic condition would have led one to expect.
—A.R. Southwood on ulnar longitudinal deficiency, cited by Adrian Flatt
In the presence of a normal brain and contralateral arm and hand, the functional deficits from a unilateral ulnar longitudinal deficiency are less than those the parents initially expect. The quality of the thumb and remaining digits is critical for functional use. Since the ulna predominately determines anatomic elbow motion and function, children with more involved ulnar deficiencies will be dependent on compensatory motion for placement of the hand in space. The arm is usually foreshortened, which helps hand-to-face activities when elbow motion is absent or limited. The internally rotated arm with ulnar-deviated wrist and bowed forearm can put the hand in a disadvantaged position. Scapulothoracic, glenohumeral, head, and neck motions compensate for these difficult anatomic variations. In the end, the goal of treatment is to improve function because, as of yet, we cannot normalize the situation. In the nearly 100 years since Southwood’s statement, and 30 years since Flatt’s citation, too little unfortunately has changed.
Etiology and Epidemiology
Longitudinal deficiency of the ulna is a very rare upper limb congenital difference, seen in about 1:100,000 live births.1 It is much less common than radial longitudinal deficiency. Ogino’s experimental animal model revealed that lethal cardiac anomalies can occur with embryonic ulnar dysplasia.2 Unlike radial dysplasia, ulnar dysplasia that comes to term in human pregnancies is usually not associated with nonmusculoskeletal organ system anomalies. These children can have proximal femoral focal deficiency, fibular deficiency, phocomelia, and/or scoliosis. They do not require screening for cardiac, renal, gastrointestinal, or hematopoietic malformations the way radial club hand infants do. Some ulnar longitudinal deficiencies can be genetic, such as fibula-ulna or femur-fibulaulna syndromes. These children are a mesomelic dwarfism variation and require combined upper and lower extremity orthopaedic care. Cornelia de Lange syndrome children can also have ulnar longitudinal deficiency.
Unilateral involvement is much more common. The vast majority of ulnar club hands are missing digits on the ulnar side, but most also have thumb malformations. Thus the malformation often extends beyond a strict ulnar longitudinal deficiency. Syndactyly is seen in about one-third
of the cases.3, 4, 5 and 6 Carpal anomalies and fusions are very common with the pisiform almost always absent and the hamate commonly absent. The radius is present but usually foreshortened with a concavity ulnarly.
of the cases.3, 4, 5 and 6 Carpal anomalies and fusions are very common with the pisiform almost always absent and the hamate commonly absent. The radius is present but usually foreshortened with a concavity ulnarly.
There have been many classification systems since Kummel in 1895. The classification systems have variably focused on the forearm, hand, thumb, or some combination thereof.2,3,6, 7, 8, 9 and 10 Bayne’s classification parallels the radial longitudinal classification and makes it easy for most to remember. Type I is a hypoplastic ulna, type II is an absent distal ulna, type III is complete absence of the ulna, and type IV is complete absence of the ulna with radial-humeral fusion. Manske emphasized the status of the thumb in surgical decision making, similar to his classification for cleft hands.
Clinical Evaluation
As with any congenital difference, there is parental and primary care concern about malformations of other organ systems. However, these cases occur almost always in isolation or less commonly, with associated musculoskeletal malformations. Evaluation of the upper limb deficiency is by serial clinical exams and plain radiographs. Deformity is monitored over time to see if there is progressive wrist ulnar deviation, forearm instability, limb foreshortening, or functional deficits. The presence or absence of pain is recorded in older children. Their emotional wellbeing and social status is followed. Anyone who cares for children with congenital differences needs to be a highranking amateur psychologist; but, we also need to know the boundaries of our skills and knowledge.
The spectrum of ulnar longitudinal deficiency is broad. The simplest is absence of ulnar digital ray(s). These children are normal functionally. Since most people do not count fingers, cosmetically their deficiency is often not noted socially. Reassurance and time for the parents to be convinced that all is well is the major form of care for these children.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree