Ulnar Collateral Ligament Reconstruction
Christopher S. Ahmad MD
Raffy Mirzayan MD
Neal S. Elattrache MD
History of the Technique
Injury to the elbow ulnar collateral ligament (UCL) from valgus forces was first described in a javelin thrower in 1946 by Waris.1 The injury then became well recognized in overhead throwing athletes with baseball pitchers at highest risk. Jobe et al.2 developed the original UCL reconstruction and described the technique with initial results in 1986. The technique utilized a tendinous transection and reflection of the flexor-pronator mass, submuscular transposition of the ulnar nerve, and creation of humeral tunnels that penetrated the posterior cortex (Fig. 30-1). This technique offered excellent exposure at the expense of morbidity to the flexor-pronator mass and ulnar nerve. Since that initial report, modifications in the surgical technique have been made to ease technical demands and decrease soft tissue morbidity. A muscle splitting approach has been developed to avoid detachment of the flexor-pronator mass with or without subcutaneous transposition of the ulnar nerve.3 Modifications in bone tunnel creation have also been made, which direct the tunnels anterior on the humeral epicondyle to avoid risk of ulnar nerve injury while the graft remains passed in a figure-eight fashion.3 Further changes in bone tunnel configuration have also been developed to reduce the number of tunnels and facilitate easier graft tensioning.4,5 Results with these modified techniques have proven effective in returning high-level athletes back to throwing.
Indications and Contraindications
Patients with a diagnosis of UCL insufficiency that fail nonoperative treatment are candidates for reconstruction. Accurate diagnosis is based on a history of medial elbow pain during the late cocking/early acceleration phase of throwing. Chronic injuries present gradually, often with painful symptoms occurring only when throwing greater than 50% to 75% of maximal effort, accompanied with inaccurate ball placement. Acute injuries may present suddenly with a pop, sharp pain, and inability to continue throwing. Physical examination features that support the diagnosis include point tenderness elicited directly over the UCL or toward its insertion site at the sublime tubercle. Valgus instability is tested with the patient’s elbow flexed between 20 degrees and 30 degrees to unlock the olecranon from its fossa as valgus stress is applied. The milking maneuver is performed by either the patient or the examiner by pulling on the patient’s thumb to create valgus stress with the patient’s forearm supinated and elbow flexed beyond 90 degrees. The moving valgus stress test is a modification of the milking maneuver where valgus stress is applied while the elbow is moved through an arc of flexion and extension. For both tests, the subjective feeling of apprehension, instability, or localized pain to the UCL indicates UCL injury.
Imaging studies confirm the diagnosis. Valgus stress radiographs may be used to document excessive medial joint line opening, and an opening greater than 3 mm has been considered diagnostic of valgus instability.2,3,6 Conventional magnetic resonance imaging (MRI) delineates the UCL and is capable of identifying thickening within the ligament or more obvious full thickness tears. MR arthrography enhanced with intra-articular gadolinium improves the diagnosis of partial undersurface tears.7
Patients who wish to continue throwing, have failed nonoperative treatment, have an accurate diagnosis, and are willing to participate in the lengthy rehabilitation are indicated for surgical reconstruction. Certain career and timing
situations may favor more immediate reconstruction without demonstrating failed nonoperative treatment. Relative contraindications include an inability to participate in lengthy rehabilitation and poor patient motivation.
situations may favor more immediate reconstruction without demonstrating failed nonoperative treatment. Relative contraindications include an inability to participate in lengthy rehabilitation and poor patient motivation.
Patients who present with valgus extension overload should also be thoroughly evaluated and considered for UCL reconstruction. In a report of professional baseball players who underwent olecranon debridement, 25% developed valgus instability and eventually required UCL reconstruction.8 This important observation suggests that both the olecranon and the UCL contribute to valgus stability. Therefore, olecranon resection may increase the demand placed on the UCL in resisting valgus forces during throwing. A recent biomechanical study demonstrated that increasing amounts of olecranon resection result in increased elbow valgus angulation.9 The authors of that study suggested that these kinematic alterations place the UCL at increased risk for injury. Ahmad et al. have demonstrated that UCL injury results in contact alterations in the posterior compartment that leads to osteophyte formation (Ahmad et al., AOSSM Annual Meeting, Orlando, Fla, 2003). Based on these clinical and basic science studies, we advocate careful evaluation of the UCL in patients presenting with valgus extension overload. Consideration should be given to UCL reconstruction in combination with posterior debridement in these patients who fail nonoperative treatment and have combined posteromedial impingement and UCL injury.
Surgical Techniques
Jobe Technique
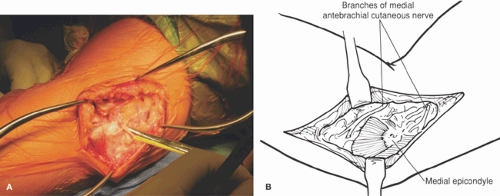
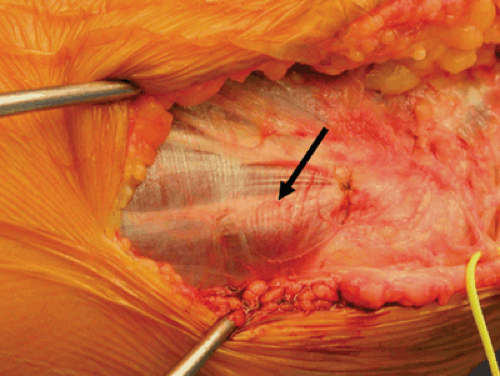
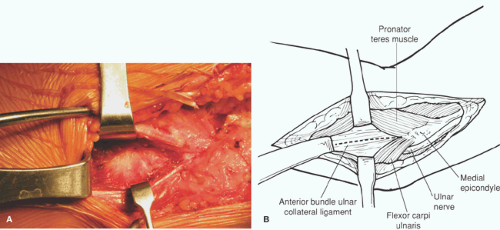
The patient is positioned supine and the arm is placed on an arm board. An examination under anesthesia is performed and a pneumatic tourniquet is placed on the upper arm. After prepping and draping, a consistent valgus stress is applied to the elbow using a small towel placed beneath the extended elbow with the forearm supinated. The arm is exsanguinated and the tourniquet inflated. A skin incision is centered over the medial epicondyle and extended 5 cm both proximally in the direction of the humerus and distally in the direction of the ulna. Dissection is carried down to the muscle fascia while identifying and protecting all sensory branches of the medial antebrachial cutaneous nerve (Fig. 30-2). A longitudinal incision in the common flexor mass is made at its posterior third in line with a tendinous raphe of the flexor carpi ulnaris (Fig. 30-3). A periosteal elevator is used to separate the flexor muscle mass from the UCL-capsular complex. Blunt retractors are placed and the ligament is inspected and palpated under valgus stress (Fig. 30-4).
If a gross ligament tear is not obvious, a longitudinal split is made in the ligament to allow inspection of the joint for loose bodies, degenerative changes, and quality of the length tension of the ligament with valgus force. Valgus stress with the elbow at 30 degrees flexion will reveal any opening of the
ulnohumeral articulation, with greater than 2 mm of gap indicating insufficiency of UCL (Fig. 30-5).
ulnohumeral articulation, with greater than 2 mm of gap indicating insufficiency of UCL (Fig. 30-5).
If necessary, posterior olecranon osteophytes can be removed at this time through a vertically oriented, posterior arthrotomy. Care must be taken to protect the ulnar nerve while an osteotome and a rongeur are used to remove the tip of the olecranon or debride posterior loose bodies. The arthrotomy is closed with absorbable suture. An alternative for patients with posterior olecranon osteophytes or loose bodies is to perform elbow arthroscopy prior to ligament reconstruction.
The ulnar tunnel is created with converging 3.2-mm drill holes made just anterior and posterior to the sublime tubercle of the coronoid process that serves as the anterior bundle’s insertion site. The drill holes are approximately 5 mm distal to the articular surface with at least a 5-mm bridge between the holes (Fig. 30-6). A curette is then used to connect the tunnels at their apex.
The initial humeral tunnel is created with a 4.5-mm drill hole made at the site of anatomic origin of the anterior bundle of UCL on the medial epicondyle directed superiorly. Care is taken to avoid penetration of the posterior cortex and injury to the ulnar nerve (Fig. 30-7). To create the superior humeral tunnels, the medial supracondylar ridge is exposed with a second longitudinal split in the flexor-pronator mass. A 3.2-mm drill hole is placed just anterior to the epicondylar attachment of the medial intermuscular septum and directed to communicate with the 4.5-mm drill hole in the epicondyle. A second 3.2-mm drill hole is made in the anterosuperior surface of the epicondyle approximately 1 cm from the previous 3.2-mm hole and also communicating with the 4.5-mm epicondylar hole.
Attention is then turned to harvesting the palmaris longus tendon graft. With the forearm fully supinated, the tendon is identified just ulnar to the flexor carpi radialis. A 1-cm transverse incision is then made at the level of the distal flexor wrist crease directly over the tendon (Fig. 30-8). A hemostat is used to develop the tendon from surrounding soft tissue. The tendon is palpated proximally and a second transverse incision is made approximately 8 cm from the distal incision. Serial transverse incisions are made more proximally as needed, in a fashion similar to the first and second incisions, until the level of the musculotendinous junction is identified. Usually three incisions are required. The tendon is transected distally and brought out through the proximal incision. The tendon is divided at the musculotendinous junction to give a length of 15 to 20 cm. The incisions are irrigated and closed routinely.
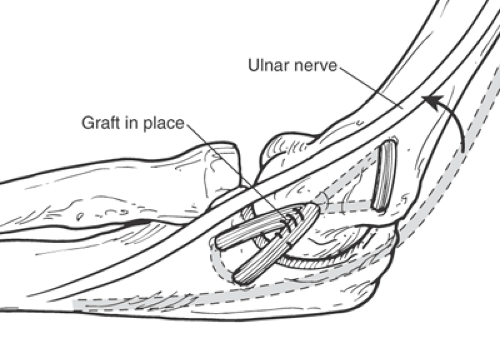
A 1-0 nonabsorbable braided suture is placed in one end of the graft using a locking stitch. The graft is then passed through the ulnar tunnel using a hooked suture passer or a
curved free needle and weaved through the humeral tunnels in a figure-eight fashion across the joint. With a standard-length autogenous graft, an effort is made to pull the excess graft end back into the ulnar tunnel, creating a three-ply reconstruction (Fig. 30-9).
curved free needle and weaved through the humeral tunnels in a figure-eight fashion across the joint. With a standard-length autogenous graft, an effort is made to pull the excess graft end back into the ulnar tunnel, creating a three-ply reconstruction (Fig. 30-9).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree