Posterior Cruciate Ligament Reconstruction Using the Tibial Inlay
Hans P. Olsen MD
Mark D. Miller MD
History of the Technique
The posterior cruciate ligament (PCL) is infrequently injured with an estimated incidence of 3 to 16% of all knee injuries.1 There has been less investigation of the mechanics and function of the PCL when compared with the anterior cruciate ligament (ACL). In recent years a better understanding of the short- and long-term consequences of PCL deficiency has spurred research to find the optimal method for reconstructing this ligament. There have been several techniques of PCL reconstruction developed; however, no single operation has emerged as the gold standard to predictably restore posterior stability and PCL function. We believe that, as with other procedures in orthopedic surgery, the best results stem from procedures that re-create normal anatomy.
The PCL originates at the posterolateral aspect of the medial femoral condyle, inserting extra synovially in a central sulcus located 1 cm distal to the posterior edge of the tibial plateau. The ligament consists of a large anterolateral and smaller posteromedial portion, each of which has distinct and consistent insertions, in addition to variable meniscofemoral ligaments. These ligaments originate from the lateral meniscus and insert anterior and posterior to the PCL on the medial femoral condyle. The meniscofemoral ligaments (ligaments of Humphrey and Wrisberg) commonly remain intact following PCL rupture and provide some posterior stability to the knee. The smaller posteromedial portion of the PCL consists of shorter fibers that are taut in knee extension. The anterolateral bundle is the thickest in diameter, contains the longest fibers, and is taut with knee flexion. This is the portion of the PCL that provides the greatest tensile strength and resists posterior tibial translation beginning at 30 degrees of flexion.2,3
Historically, most PCL reconstructions have emphasized an anterior to posterior approach to re-create the anterolateral bundle. This has been performed through a long oblique interosseous tunnel that creates difficulty with graft passage. These reconstructions require the graft to bend around a large angle at the back of the tibia, which has been dubbed the “killer turn,” and has been implicated as a cause of graft failure.4
The tibial inlay technique was originally developed in Europe and introduced to the United States by Berg5 in 1995. This method produces a more anatomic reconstruction of the PCL by placing the distal portion of the graft directly in the PCL sulcus, in the posterior aspect of the tibia. Thus, the tibial inlay method avoids creating the “killer turn” of the graft associated with other reconstruction techniques.
This chapter describes the combined original concept of the tibial inlay with a posterior approach to the tibia as described by Burks and Schaffer.6 Additional refinements have been added, leading to the technique discussed herein.
Indications and Contraindications
Diagnosis
A thorough history of the events of injury is needed to make the diagnosis of a PCL injury. Common mechanisms of PCL injury include “dashboard injuries” during motor vehicle accidents or overloading of the knee and quadriceps in hyperflexion during athletic events. Isolated PCL injuries are more likely to be associated with athletic injury than any other mechanism. Acute, isolated PCL rupture is often associated with a smaller hemarthrosis than with ACL injury. Problems with knee instability with cutting or rapid
deceleration movements are less common than with ACL injured patients, although they may give a history of an instability sensation especially when on uneven ground. Many athletes will continue to play on a PCL injured knee and won’t seek medical attention until they develop a pain or ache in the following days. Patients with PCL injuries may complain that the knee is just “not right” or have other subjective complaints such as a generalized “aching.” Chronic PCL injured patients will report pain (medial and patellofemoral) with ambulation or descending stairs.
deceleration movements are less common than with ACL injured patients, although they may give a history of an instability sensation especially when on uneven ground. Many athletes will continue to play on a PCL injured knee and won’t seek medical attention until they develop a pain or ache in the following days. Patients with PCL injuries may complain that the knee is just “not right” or have other subjective complaints such as a generalized “aching.” Chronic PCL injured patients will report pain (medial and patellofemoral) with ambulation or descending stairs.
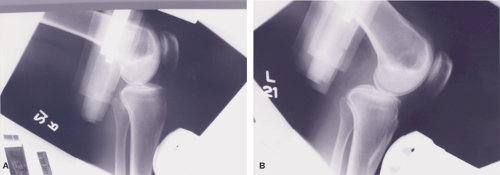
 Fig. 43-1. Posterior drawer test. A: Image shows normal tibio-femoral relationship prior to test. B: Image showing abnormal posterior tibial translation with applied posterior stress force. |
PCL tears frequently occur with concomitant ligamentous, bony, or capsular injuries to the knee. In the trauma setting, these associated injuries can occur up to 60% of the time.7 Following medial or lateral collateral ligament damage, varus or valgus stress to the tibia may result in PCL injury. A hyperextension mechanism of PCL rupture can occur after the ACL is torn and is also associated with a posterior capsular injury. The most common combination is the combined PCL and posterolateral corner injury, which is reported to occur in up to 60% of all combined injuries.7
The physical exam is critical to making the correct diagnosis of PCL injury. The posterior drawer test is 90% sensitive and 99% specific for PCL pathology and should be considered the gold standard for diagnosis8 (Fig. 43-1A,B). The posterior sag test, the Godfrey test, the prone drawer, the quadriceps active test, and the dynamic posterior shift test may all be used to confirm a PCL injury. An isolated grade-III PCL injury is uncommon, thus other ligamentous injuries must be sought when looking for any additional instability. Knee dislocation must be ruled out any time there is the possibility of a multiligament injury. A careful hip and ankle exam as well as a neurovascular exam should be performed, especially if associated with high energy trauma or a potential knee dislocation. Posterolateral instability is commonly associated with PCL injury and may be diagnosed with external rotation asymmetry (Fig. 43-2A,B), the external
rotation recurvatum test, posterolateral and posteromedial drawer test, or the reverse pivot shift test. External rotation asymmetry has been proven to be the most reliable indicator of posterolateral instability.
rotation recurvatum test, posterolateral and posteromedial drawer test, or the reverse pivot shift test. External rotation asymmetry has been proven to be the most reliable indicator of posterolateral instability.
Radiographic studies, including plain films, stress radiography, and magnetic resonance imaging (MRI), are used to confirm clinical suspicion of a PCL injury. Plain films can be used to assess for any bony avulsion, tibial plateau fracture, or fibular head fracture suggesting possible posterolateral corner injury. Stress films are used to quantify posterior instability and can confirm clinical suspicions. It is noninvasive, reproducible, and a reliable method for determining the amount of posterior tibial translation (Fig. 43-3A,B).
Historically, the management of PCL injuries has been nonoperative. Conservative management usually involves early brace treatment with progressive range of motion exercises, followed by a quadriceps strengthening program early in the postinjury period. Protecting the knee from posterior tibial translation is crucial. Patients are typically restricted from athletics until 90% of contralateral quadriceps and hamstring strength is obtained. Recently, the accepted management of complete PCL tears has become more aggressive, with a lower threshold for operative treatment. This is the result of long-term follow-up studies that demonstrate worse results with nonoperative treatment. These studies also show radiographic deterioration with time, especially in the medial and patellofemoral compartments.9 The rate of arthrosis severity and progression depends upon the degree of posterior instability, quadriceps weakness, and the presence of additional ligamentous or meniscal damage. Nonoperative treatment is now reserved for asymptomatic, acute, isolated PCL tears with mild posterior laxity (grades I and II), or chronic isolated PCL injuries that are asymptomatic.
The development of pain and degenerative arthritis is more common in patients with combined PCL injuries. Thus, patients who suffer PCL injuries in combination with bony avulsion injuries, posterolateral corner injuries, or concomitant ligamentous injuries (grade III medial collateral ligament [MCL] or ACL rupture) require operative reconstruction of the PCL. Combined MCL-PCL injuries often need both components fixed. Combined PCL and posterolateral corner injuries are an indication for operative treatment because the posterolateral corner is a secondary stabilizer to posterior displacement. Posterolateral corner injuries should be reconstructed within 2 weeks of injury. Isolated PCL injuries with grade-III posterior laxity/instability are also an indication for operative management. Finally, active, young patients who demonstrate less than 10 mm of posterior laxity on displacement testing (grade II) but with symptomatic complaints of instability or pain should also have the PCL reconstructed.
Another relative indication for the use of the tibial inlay technique involves the revision setting. The tibial inlay technique is useful when a previous nonanatomic reconstruction has been performed. This avoids complications associated with previous tibial tunnels that are too wide in diameter or too proximal on the tibia. Patients with tibial osteopenia, previous fracture, or previous osteotomy may benefit from the tibial inlay technique to prevent proximal graft migration.10
When operative management is indicated the type and site of injury is critical in choosing the correct surgical procedure. Bony avulsion injuries involving the PCL insertion at the posterior tibia are treated with primary repair using lag screws or suture fixation. Midsubstance tears of the PCL require ligament reconstruction, which attempts to reproduce normal anatomy. We believe that the tibial inlay technique produces the most anatomic PCL reconstruction.
The tibial inlay technique is contraindicated in patients who have had prior vascular procedures, especially those who have had remote vascular repairs.
Surgical Technique
Preoperative Planning
Prior to surgery, it is necessary to diagnose concomitant knee pathology and to quantify the degree of posterior instability. With the assistance of stress radiography (Fig. 43-3) or instrumented ligament testing using the KT-1000/2000 (MedMetric, San Diego, CA), PCL instability may be quantified.11,12 Plain radiographs are used to exclude associated bony injury and to assess radiographic signs of arthrosis. Magnetic resonance imaging is also used as an adjunct to diagnosis and development of treatment plan. MRI is nearly 100% sensitive and specific for diagnosing PCL tears.13 In addition, MRI may be used to diagnose meniscal injuries, which should be addressed at the time of surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree