Anterior Cruciate Ligament Reconstruction Using Nonirradiated Fresh Frozen Patellar Tendon Allograft
Andrew H. Smith MD
Bernard R. Bach Jr MD
History of the Technique
The evolution and refinement of endoscopically assisted anterior cruciate ligament (ACL) reconstruction evolved in the 1990s. With the development of the technique, the search for the ideal ACL graft continues to flux. With slight modifications in the method, different graft types can be accommodated. Hamstring, quadriceps, patellar bone-tendon-bone (BTB), and other autografts have all been used with success. The reproducible favorable results of patellar bone-tendon-bone (BTB) autografts has led to its perception as the “gold standard” for ACL grafts. However, BTB autograft is associated with greater donor site morbidity, longer surgical time for graft harvest, and a longer initial period of protected weight bearing compared to other autograft sources. Allograft usage has evolved from the desire to gain all of the favorable characteristics of BTB graft and eliminate the negative aspects of autograft harvest. BTB allograft allows secure fixation and eliminates donor sire morbidity. The purpose of this chapter is to review our experience with nonirradiated patellar tendon allografts for ACL reconstruction.
Indications and Contraindications
More than 200,000 ACL tears occur in the United States annually. Approximately one half of these injuries undergo surgical reconstruction. The decision to perform an ACL reconstruction should be based on a discussion with the patient to determine his or her desired activity level and willingness to participate in postoperative rehabilitation. Allograft can be recommended in nearly every situation in which autograft is used. Patients over 40 years of age, patients with patellofemoral symptoms, and patients with early degenerative changes are suited for allograft due to the absence of donor site morbidity. Because of insufficient autograft donor tissue, petite females are also particularly good candidates for allograft tissue for reconstruction. Additionally, with no harvest time and no donor site morbidity, allografts are particularly suitable for bilateral reconstructions and multiligament reconstructions.
The contraindications for BTB allograft are the same as with ACL reconstruction using BTB autograft. Interference screw fixation placed across open growth plates in a skeletally immature patient with a significant amount of growth remaining is not recommended. In most situations, allograft and autograft can be used interchangeably. In certain situations, allograft may be more desirable than autograft. In patients with pre-existing patellofemoral degeneration, multiple ligament knee reconstructions, and in revision situations, BTB allograft may be more desirable than autograft tissue. A contraindication to the use of allograft tissue is the desire by the patient not to be subjected to the risk of disease transmission, however small it may be.
Surgical Technique
Preoperative Evaluation
All patients undergoing ACL reconstruction should have a history of symptomatic knee instability. Clinical examination supporting the diagnosis of anterior cruciate knee confirms the diagnosis. A KT-1000 arthrometer (Medmetric, San Diego, CA) is used to document the degree of anterior-posterior translation. Magnetic resonance imaging (MRI) is obtained to evaluate for concomitant pathology, which can be addressed at the time of surgery. Risks, complications, and benefits of surgery are discussed with the patient preoperatively.
Anesthesia
All ACL reconstructions are performed on an outpatient basis under general anesthesia. Our practice has been to routinely administer intra-articular bupivacaine at the end of the case. Some surgeons prefer a femoral nerve block for additional postoperative pain relief, although this is not part of our current outpatient protocol. A spinal anesthetic can be used instead of a general anesthetic according to surgeon preference.
Examination Under Anesthesia
A careful examination of the injured knee under anesthesia and documentation of findings are essential in the operative report. The exam of the injured knee involves a comprehensive evaluation of all knee ligaments and must be accompanied by a comparison examination of the contralateral, normal knee. The examination under anesthesia confirms the diagnosis and may identify associated pathology. With the absence of guarding, exam subtleties may be noted in the anesthetized patient that were not appreciated while awake.
The patient is examined in the supine position after suitable anesthesia. The Lachman and pivot shift tests are performed and graded. Varus and valgus stability is tested at 0 and 30 degrees. The thigh-foot angle is measured at 30 degrees and 90 degrees. Posterior cruciate ligament (PCL) stability and posterolateral corner integrity are checked. Anterior and posterior drawer tests are also performed and graded.
A positive pivot shift test under anesthesia confirms the diagnosis of ACL insufficiency. At this point in the procedure, it is appropriate to begin to thaw the allograft. The allograft will be thawed and ready to work with later in the case when it is time to tailor it to the proper size.
Patient Positioning
The patient is positioned on the table supine. The waist of the table is kept slightly flexed to eliminate lumbar hyperlordosis. The operative leg is placed in a padded thigh tourniquet incorporated into an arthroscopic leg holder, allowing for knee flexion of 110 degrees. In the majority of cases, the tourniquet is not inflated. The nonoperative leg is placed in a padded leg holder which holds the posterior calf and heel with the hip and knee flexed to protect the common peroneal and femoral nerves. The leg is prepped twice with DuraPrep and draped in the usual fashion. A first generation cephalosporin is administered for preoperative antibiotic prophylaxis.
Diagnostic Arthroscopy
Diagnostic arthroscopy is performed first. Bupivacaine 0.25% with epinephrine is injected into the knee joint and surrounding arthroscopic portals. A superomedial portal is used for pump outflow. The improved visualization afforded by creating a separate outflow portal is one of the reasons why tourniquet inflation is rarely required. The arthroscope is inserted through an inferolateral portal created at the level of the distal patella with the knee flexed at 90 degrees. Easy transition is made with placement of the arthroscope into the suprapatellar pouch. The patella and trochlea are then inspected for articular injury and contact. The medial and lateral gutters are then inspected for loose bodies and peripheral osteophytes.
The arthroscope is maneuvered into the medial compartment. A spinal needle is used to triangulate an incision for placement of the inferomedial portal. It is made as close to the patella tendon as possible to facilitate subsequent intercondylar notch work. A probe is inserted via the inferomedial portal, and medial meniscal integrity and stability are tested. While in the medial compartment, any articular damage of the medial femoral condyle and medial tibial plateau is graded and documented.
The lateral compartment is then inspected initially in 30 degrees of flexion with varus, and then in the figure-four position. The lateral meniscus is probed, checking for meniscal injury. Any articular damage to the lateral femoral condyle or lateral tibial plateau is graded and documented. The popliteus tendon and popliteal hiatus are inspected for injury; they are visualized from both the lateral compartment and from the lateral gutter. The scope is then transitioned into the intercondylar notch.
Once in the intercondylar notch, the ACL remnant is probed to identify the level of injury. The empty wall and vertical strut signs may be present. Intercondylar notch width is assessed at this time in preparation for notchplasty. An arthroscopic shaver is inserted via the medial portal. Debridement may be facilitated by morselizing the remnant tissue with arthroscopic scissors and an arthroscopic osteotome. Hemostasis is controlled with an arthroscopic electrocautery. Once the ACL remnant is resected, the PCL is examined and the diagnostic portion is complete.
Notch Preparation
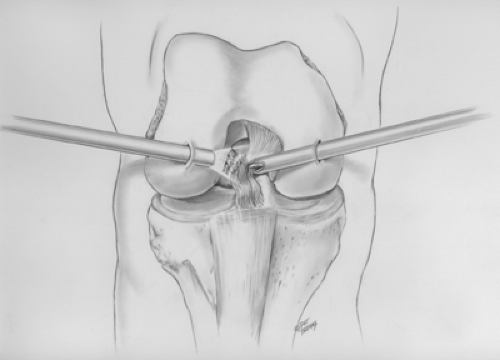
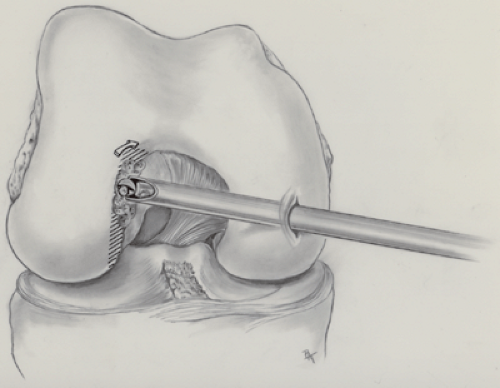
The intercondylar notch is prepared by first removing residual ACL tissue, which is cut with arthroscopic scissors, osteotome, shaver, and electrocautery (Fig. 38-1). After removal of the ACL remnant, a notchplasty is performed with a 0.25-inch curved osteotome, a mallet, and grasper. The notchplasty is then competed with a spherical burr until the over-the-top position is clearly confirmed with an arthroscopic probe (Fig. 38-2).
Graft Preparation
As the notchplasty is being performed, the case can be expedited by having an assistant prepare the allograft. This will significantly reduce anesthesia time for the patient. A fresh frozen, nonirradiated whole or hemi-patellar allograft obtained from a single supplier is preferred. The graft is placed in a warm saline bath at the beginning of the case once ACL insufficiency is confirmed. During the thawing
phase, the graft should be kept inside its plastic packaging. This prevents the ligamentous portion of the allograft from becoming edematous. An oscillating saw is used to fashion the bone plugs. The bone plugs are shaped to be 25 mm in length. Sizing tubes are used to confirm that bone plug width and soft tissue width is 10 mm. Two 0.062 K-wire drill holes are placed through the distal bone plug for passage of two no. 5 Tycron sutures. The tendo-osseous junctures are marked with a sterile marking pen (Fig. 38-3). The cortical edge of the distal bone plug is marked to allow for orientation. The total length of the soft tissue construct is measured. The prepared graft is wrapped in a moist saline sponge and set aside.
phase, the graft should be kept inside its plastic packaging. This prevents the ligamentous portion of the allograft from becoming edematous. An oscillating saw is used to fashion the bone plugs. The bone plugs are shaped to be 25 mm in length. Sizing tubes are used to confirm that bone plug width and soft tissue width is 10 mm. Two 0.062 K-wire drill holes are placed through the distal bone plug for passage of two no. 5 Tycron sutures. The tendo-osseous junctures are marked with a sterile marking pen (Fig. 38-3). The cortical edge of the distal bone plug is marked to allow for orientation. The total length of the soft tissue construct is measured. The prepared graft is wrapped in a moist saline sponge and set aside.
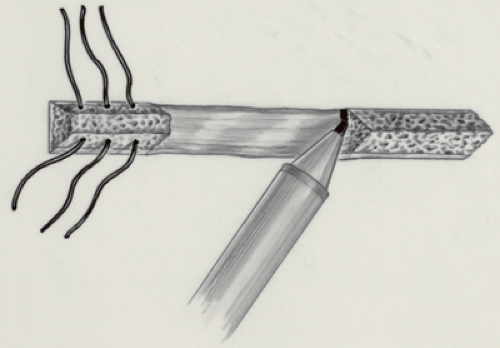 Fig. 38-3. The tendo-osseous junction of the graft is marked for orientation. (Reproduced with permission from Hardin GT, Bach BR, Bush-Joseph CA, et al. Endoscopic single incision ACL reconstruction using patellar tendon autograft: surgical technique. Am J Knee Surg. 1992;5:144–155.)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|