Management of Extensor Mechanism Ruptures
Bruce S. Miller MD
James E. Carpenter MD
History of the Technique
Disruption of the quadriceps or patellar tendon usually occurs as a result of eccentric overload of the extensor mechanism in a flexed or hyperflexed knee and planted foot.1 Patellar tendon ruptures occur most commonly in athletic individuals under the age of 40.1,2 Quadriceps tendon ruptures are most commonly seen in older individuals or those with systemic disease, including diabetes, uremia, lupus, and obesity. Bilateral, simultaneous quadriceps tendon ruptures have been described in patients with systemic disease.
Rupture of the patellar or quadriceps tendon results in a loss of extensor mechanism continuity, which is essential for normal knee function. A palpable defect, weakness, and buckling are the hallmarks of diagnosing these injuries. Despite such seemingly obvious findings, ruptures of these structures continue to go unrecognized, at times leading to a potentially long delay in presentation and subsequent treatment. Because of the profound effect of extensor mechanism disruption on knee function, all complete patellar and quadriceps tendon ruptures require operative repair. Partial ruptures may occur acutely, but most commonly are chronic injuries due to repetitive force involving full contractions as seen in jumping sports such as basketball and volleyball (hence the term “jumper’s knee”). There is some evidence that acute, complete ruptures often occur in areas of pre-existing partial injuries (tendinosis). Management of tendinosis or partial tendon injury is beyond the scope of this chapter.
Repair of the acutely ruptured extensor mechanism involves an anatomic end-to-end suture repair of the injured structures, as described below. Few, if any, technical advances have been made in the acute repair of the quadriceps or patellar tendon as the results of primary suture repair through transosseous tunnels appear to have stood the test of time. Operative intervention for a chronic or neglected rupture of the extensor mechanism usually requires reconstruction with a soft tissue autograft or allograft, and this is addressed below.
Indications and Contraindications
Traumatic disruptions of the extensor mechanism lead to marked functional loss if left untreated.3 Thus, all recognized ruptures of the quadriceps or patellar tendon should be surgically repaired as soon as the skin and soft tissues allow. The most favorable functional outcomes have been reported after early repair of an acute rupture, and patellar tendon repairs have been reported to have better functional outcomes than quadriceps tendon repairs.1,2,3,4 A delay in diagnosis or treatment can lead to tendon retraction and muscle atrophy and may preclude primary repair. In the case of the neglected or chronic tear, reconstruction or supplementation with a soft tissue graft may be necessary.2 In general, the results of early repair are superior to those of late reconstructions.1,2
Ruptures of the extensor mechanism can be associated with underlying medical co-morbidities including renal failure, connective tissue disorders, and corticosteroid dependence.1 In these cases, aggressive medical management of the underlying disorder is recommended.
Surgical Techniques
Quadriceps Tendon Rupture
Anesthesia and Positioning
After successful anesthesia is administered, the patient is positioned supine on the operating table and a thigh tourniquet
is placed as proximal as possible on the injured extremity. If the leg lies in external rotation a soft support or bump can be placed under the ipsilateral hip to maintain the leg in a position with the patella positioned directly upward. The leg is then prepped and draped in the standard fashion.
is placed as proximal as possible on the injured extremity. If the leg lies in external rotation a soft support or bump can be placed under the ipsilateral hip to maintain the leg in a position with the patella positioned directly upward. The leg is then prepped and draped in the standard fashion.
Surface Anatomy
Relevant anatomic landmarks include the patella, patellar tendon, tibial tubercle, and joint line. These landmarks can be marked at the beginning of the procedure. A palpable defect is often appreciated at the site of the rupture proximal to the patella, but may be obscured by soft tissue swelling or a hemorrhagic bursitis.
Skin Incision and Surgical Procedure
The leg is exsanguinated and the tourniquet elevated. A midline longitudinal skin incision is made from a point approximately 2 cm below the inferior pole of the patella to a point approximately 10 cm above the proximal pole of the patella. Dissection is carried sharply through the skin and subcutaneous tissues to the deep fascia of the leg. The defect in the distal quadriceps tendon is entered and hematoma evacuated. The hematoma will communicate directly with the suprapatellar pouch of the knee joint. The injury is often accompanied by transverse tearing of the extensor retinaculum and joint capsule. This associated injury should be identified for later repair. The medial and lateral edges of the quadriceps tendon are exposed. The area for anatomic insertion of the quadriceps tendon at the proximal pole of the patella is identified and any residual tendinous or granulation tissue is debrided. At times, especially with subacute or delayed repairs, fibrous tissue has filled the gap between the superior pole of the patella and the more proximal tendon stump. This tissue needs to be mobilized out of the way to allow for a direct tendon to bone repair; however, it can sometimes be reflected and used later to reinforce and protect the repair junction. The anatomic insertion is then carefully decorticated with a bur to facilitate healing at the bone-to-tendon interface of the repair site.
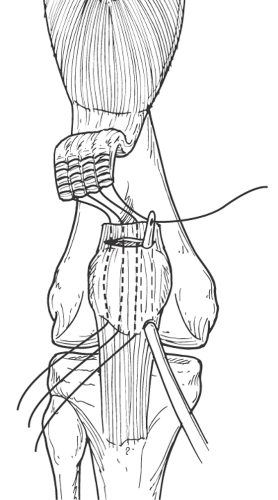
A no. 5 braided nonabsorbable suture (or one of the new extra strength sutures, e.g., Arthrex FiberWire) is then whipstitched from one edge of the distal tendon stump proximally, and then returned centrally down the tendon in an in-and-out fashion. This suture technique minimizes strangulation of the tendon. A second suture is then applied to the other edge of the tendon in a similar fashion. Tension is applied to the distal suture limbs to ensure that no laxity remains in the suture as it courses through the tendon. Depending on the size of the tendon, a third suture may be used in a similar fashion.
A 2-mm drill bit is then employed to make three (or four) longitudinal parallel tunnels through the patella. One drill hole is placed in the center of the planned repair site at the proximal pole of the patella, and the other two tunnels are positioned parallel on either side of the central one. These drill tunnels exit the distal pole of the patella, just anterior to the origin of the patellar tendon.
A Hewson Suture Retriever (Smith & Nephew, Andover, Mass) is used to facilitate passage of the quadriceps tendon sutures through the osseous tunnels in the patella. Marking one of the sutures with ink prior to passage through the osseous tunnels will facilitate suture management. The most medial suture limb is passed through the medial drill hole, the most lateral suture is passed through the lateral drill hole, and the central suture limbs are passed through the central drill hole(s). With the knee in full extension, the quadriceps tendon is reduced to the proximal pole of the patella by applying distal tension to the sutures. The medial suture is then tied to its matching limb that has passed through the central tunnel, and this process is then repeated with the lateral suture. This repair technique is illustrated in Figure 55-1.
The disrupted retinaculum and joint capsule medial and lateral to the tendon rupture site are then repaired with interrupted no. 2 nonabsorbable sutures. The knee is then gently flexed, and the degree of flexion at which tension in the repaired quadriceps tendon develops is noted. This information is helpful in protecting the repair during the early rehabilitation process.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree