Anterior Cruciate Ligament Reconstruction in the Skeletally Immature Patient
Mininder S. Kocher MD, MPH
Anterior cruciate ligament (ACL) injuries in skeletally immature patients are being seen with increased frequency. Management of these injuries is controversial. Nonreconstructive treatment of complete tears typically results in recurrent functional instability with risk of injury to meniscal and articular cartilage. A variety of reconstructive techniques have been utilized, including physeal sparing, partial transphyseal, and transphyseal methods using various grafts. Conventional adult ACL reconstruction techniques risk potential iatrogenic growth disturbance due to physeal violation. Growth disturbances after ACL reconstruction in skeletally immature patients have been reported.
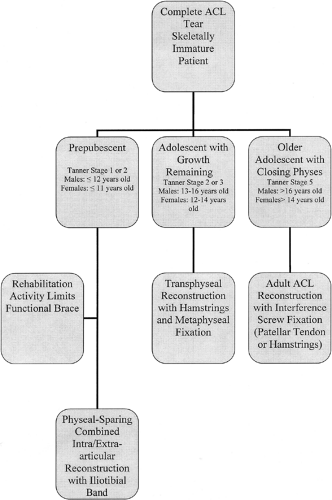
In this chapter, we discuss our approach to ACL reconstruction in the skeletally immature patient based on physiological age (Fig. 42-1). In prepubescent patients, we perform a physeal-sparing, combined intra-articular, and extra-articular reconstruction utilizing autogenous iliotibial band. In adolescent patients with significant growth remaining, we perform transphyseal ACL reconstruction with autogenous hamstrings tendons with fixation away from the physis. In older adolescent patients approaching skeletal maturity, we perform conventional adult ACL reconstruction with interference screw fixation using either autogenous central third patellar tendon or autogenous hamstrings.
History of the Technique
Intrasubstance ACL injuries in children and adolescents were once considered rare, with tibial eminence avulsion fractures considered the pediatric ACL injury equivalent.1,2,3,4 However, intrasubstance ACL injuries in children and adolescents are being seen with increased frequency and have received increased attention. ACL injury has been reported in 10% to 65% of pediatric knees with acute traumatic hemarthroses in series ranging from 35 to 138 patients.5,6,7,8,9,10
Controversy exists regarding the management of ACL injuries in patients with open physis. Nonoperative management of partial tears may be successful in some patients.11 However, nonoperative management of complete tears in skeletally immature patients generally has a poor prognosis with recurrent instability leading to further meniscal and chondral injury, which has implications in terms of development of degenerative joint disease.12,13,14,15,16,17,18 Graf et al.,13 Mizuta et al.,17 and Janarv et al.14 have reported instability symptoms, subsequent meniscal tears, decreased activity level, and need for ACL reconstruction in the majority of skeletally immature patients treated nonoperatively in series of 8, 18, and 23 patients, respectively. Similarly, when comparing the results of operative versus nonoperative management of complete ACL injuries in adolescents, McCarroll et al.15 and Pressman et al.18 found that those managed by ACL reconstruction had less instability, higher activity and return to sport levels, and lower rates of subsequent reinjury and meniscal tears.
Conventional surgical reconstruction techniques risk potential iatrogenic growth disturbance due to physeal violation. Cases of growth disturbance have been reported in animal models19,20,21 and clinical series.22,23,24 Animal models have demonstrated mixed results regarding growth disturbances from soft tissue grafts across the physis. In a canine model with iliotibial band grafts through 5/32 inch tunnels, Stadelmaier et al.25 found no evidence of growth arrest in the four animals with soft tissue graft across the physis, whereas the four animals with drill holes and no graft demonstrated physeal arrest. In a rabbit model using a semitendinosus graft through 2-mm tunnels, Guzzanti et al.19 did have cases of growth disturbance; however, these were not common: 5% shortening (1/21) and 10% distal femoral
valgus deformity (2/21). Examining the effect of a tensioned soft-tissue graft across the physis, Edwards et al.21 found a substantial rate of deformity. In a canine model with iliotibial band graft tensioned to 80 N, these investigators found significant increases, compared to the nonoperated control limb, in distal femoral valgus deformity and proximal tibial varus deformity despite no evidence of a bony bar. Similarly, Houle et al.20 reported growth disturbance after a tensioned tendon graft in a bone tunnel across the rabbit physis.
valgus deformity (2/21). Examining the effect of a tensioned soft-tissue graft across the physis, Edwards et al.21 found a substantial rate of deformity. In a canine model with iliotibial band graft tensioned to 80 N, these investigators found significant increases, compared to the nonoperated control limb, in distal femoral valgus deformity and proximal tibial varus deformity despite no evidence of a bony bar. Similarly, Houle et al.20 reported growth disturbance after a tensioned tendon graft in a bone tunnel across the rabbit physis.
Clinical reports of growth deformity after ACL reconstruction are unusual. Lipscomb and Anderson22 reported one case of 20 mm shortening in a series of 24 skeletally immature patients reconstructed with transphyseal semitendinosus and gracilis grafts. This was associated with staple graft fixation across the physis. Koman and Sanders23 reported a case of distal femoral valgus deformity requiring osteotomy and contralateral epiphysiodesis after transphyseal reconstruction with a doubled semitendinosus graft. This case was also associated with fixation across the distal femoral physis. Kocher et al.24 reported an additional 15 cases of growth disturbances gleaned from a questionnaire of expert experience, including eight cases of distal femoral valgus deformity with an arrest of the lateral distal femoral physis, three cases of tibial recurvatum with an arrest of the tibial tubercle apophysis, two cases of genu valgum without arrest due to a lateral extra-articular tether, and two cases of leg length
discrepancy (one shortening and one overgrowth). Associated factors included fixation hardware across the lateral distal femoral physis in three cases, bone plugs of a patellar tendon graft across the distal femoral physis in three cases, large (12 mm) tunnels in two cases, lateral extra-articular tenodesis in two cases, fixation hardware across the tibial tubercle apophysis in two cases, over-the-top femoral position in one case, and suturing near the tibial tubercle apophysis in one case.
discrepancy (one shortening and one overgrowth). Associated factors included fixation hardware across the lateral distal femoral physis in three cases, bone plugs of a patellar tendon graft across the distal femoral physis in three cases, large (12 mm) tunnels in two cases, lateral extra-articular tenodesis in two cases, fixation hardware across the tibial tubercle apophysis in two cases, over-the-top femoral position in one case, and suturing near the tibial tubercle apophysis in one case.
Surgical techniques to address ACL insufficiency in skeletally immature patients include primary repair, extra-articular tenodesis, transphyseal reconstruction, partial transphyseal reconstruction, and physeal sparing reconstruction. Primary ligament repair26,27 and extra-articular tenodesis alone13,15 have had poor results in children and adolescents, similar to adults. Transphyseal reconstructions with tunnels that violate both the distal femoral and proximal tibial physis have been performed with hamstring autograft, patellar tendon autograft, and allograft tissue.12,15,28,29,30,31,32,33,34,35,36,37 Partial transphyseal reconstructions violate only one physis with a tunnel through the proximal tibial physis and over-the-top positioning on the femur or a tunnel through the distal femoral physis with an epiphyseal tunnel in the tibia.38,39,40 A variety of physeal-sparing reconstructions have been described to avoid tunnels across either the distal femoral or proximal tibial physis.7,41,42,43,44,45,46,47
Table 42-1 Tanner Staging Classification of Secondary Sexual Characteristics | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree