Anterior Cruciate Ligament Reconstruction: Soft Tissue Grafts
Keith W. Lawhorn MD
Stephen M. Howell MD
History of the Technique
Historically, the use of a soft tissue graft such as a hamstring or tibialis tendon as a graft source for a torn anterior cruciate ligament (ACL) has been limited by the poor biomechanical properties of fixation devices and inconsistent placement of the tunnels. The fixation devices for use with soft tissue grafts were not as strong or stiff and were more prone to slippage than interference screw fixation of bone plug grafts like the bone-patella tendon-bone grafts (BPTB). Furthermore, the healing of a tendon to a bone tunnel is slower than a bone plug, which means that the fixation devices for a soft tissue graft must be better than for a bone plug graft and should allow circumferential healing of the tendon to the tunnel wall.1,2
Over the past decade, improvements in fixation devices have increased the use of soft tissue autografts and allografts to reconstruct the torn ACL. Biomechanical studies support the use of high strength and high stiffness fixation devices that resist slippage and allow circumferential healing of the tendon.3,4,5,6,7,8,9 Newer techniques that bone graft a soft tissue ACL graft in the femoral and tibial tunnel are now in use to promote graft-bone tunnel healing, fill voids, and further improve the stiffness at the time of implantation.9
A fixation technique, which uses the Bone Mulch Screw in the femur and WasherLoc in the tibia (Arthrotek, Warsaw, IN), was specifically developed for use with soft tissue grafts. The Bone Mulch Screw is a rigid crosspin placed through a stab incision on the lateral femur, and the WasherLoc is a multiple spiked washer that is compressed with a screw and countersunk in a recess in the tibia to avoid hardware symptoms. Both devices provide high strength and stiffness and resistance to slippage that is superior to interference screw fixation of BPTB grafts.6,10 Bone graft is used in conjunction with these two devices to promote circumferential tendon-tunnel healing, increase stiffness, and permit aggressive rehabilitation with soft tissue autografts and allografts.7,8
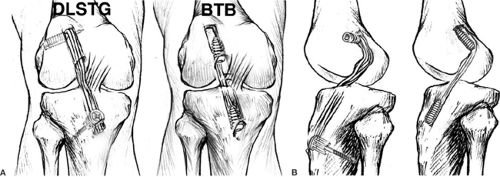
Over the past decade, improvements in the guidelines for placing the tibial and femoral tunnels in the sagittal and coronal plane has made the restoration of stability and motion of a knee reconstructed with a soft tissue graft better and more consistent. An error of a few millimeters in placement of the tibial and femoral tunnels causes impingement of a soft tissue graft against the roof in full extension, impingement against the posterior cruciate ligament (PCL) in flexion, and abnormal tension in the graft. Roof impingement causes extension loss and increased laxity, PCL impingement causes flexion loss and increased laxity, and abnormal graft tension overconstrains the knee. Impingement issues are more of a problem with the soft tissue grafts than with the bone plug grafts because the cross-sectional area of the soft tissue grafts is larger. Therefore, tunnel placement must be more precise with a soft tissue graft than a bone plug graft (Fig. 37-1).
Autografts: Soft Tissue versus Bone Plug Grafts
The most commonly used soft tissue autograft is the double-looped semitendinosus and gracilis (DLSTG) graft. The DLSTG autograft has several advantages over bone plug autografts, such as the BPTB and quadriceps tendon-bone graft. The use of a DLSTG autograft avoids extensor mechanism problems such as anterior knee pain, kneeling pain, quadriceps weakness, patella tendon rupture, infrapatellar contracture syndrome, and patella fracture, which can occur with bone plug grafts. The morbidity of autogenous DLSTG graft is low with
complete return of flexion strength and regeneration of the tendons following hamstring harvest.11,12,13,14,15,16 The DLSTG is stronger (4,304 to 4,590 N) and stiffer (861 to 954 N/mm) than the bone plug grafts.17,18 In contrast to the bone plug grafts, the biomechanical properties of a DLSTG do not deteriorate with age.19,20 Mechanically, the four strand DLSTG fixed with the Bone Mulch Screw in a single femoral socket replicates the reciprocal-tensile behavior of the native ACL, which does not occur with the single strand bone plug graft.9,18,21 The intra-articular biologic incorporation and remodeling of an autogenous DLSTG graft is more rapid than the bone plug grafts. The autogenous DLSTG graft does not die after transplantation,22 and viability depends on readily available synovial diffusion and not on revascularization23; whereas bone plug grafts undergo central necrosis and require the development of a vascular supply.24 Finally, clinical outcome studies support the use of autogenous DLSTG graft as they are as effective as an autogenous BPTB graft for restoring stability and function in the knee with a torn ACL.25,26
complete return of flexion strength and regeneration of the tendons following hamstring harvest.11,12,13,14,15,16 The DLSTG is stronger (4,304 to 4,590 N) and stiffer (861 to 954 N/mm) than the bone plug grafts.17,18 In contrast to the bone plug grafts, the biomechanical properties of a DLSTG do not deteriorate with age.19,20 Mechanically, the four strand DLSTG fixed with the Bone Mulch Screw in a single femoral socket replicates the reciprocal-tensile behavior of the native ACL, which does not occur with the single strand bone plug graft.9,18,21 The intra-articular biologic incorporation and remodeling of an autogenous DLSTG graft is more rapid than the bone plug grafts. The autogenous DLSTG graft does not die after transplantation,22 and viability depends on readily available synovial diffusion and not on revascularization23; whereas bone plug grafts undergo central necrosis and require the development of a vascular supply.24 Finally, clinical outcome studies support the use of autogenous DLSTG graft as they are as effective as an autogenous BPTB graft for restoring stability and function in the knee with a torn ACL.25,26
Allograft Soft Tissue Grafts
The most commonly used soft tissue allograft is the single loop of tibialis tendon from either the anterior or posterior tibialis tendon. Soft tissue allografts are more readily available than bone plug allografts because one cadaver provides six soft tissue allografts (i.e., two DLSTG, two anterior tibialis, two posterior tibialis) and only four bone plug allografts (i.e., two bone patella tendon bone (BPTB), two Achilles tendon). Soft tissue allografts are ideal for use in revision ACL surgery and in reconstruction of the knee with multiple ligament injuries. Soft tissue allografts are also useful in primary ACL reconstruction because they avoid harvest morbidity, decrease surgical time, and surgical scars.27 An allograft without a bone plug is quicker to thaw, easier to prepare, and has less disease transmission than an allograft with a bone plug.28 The strength and stiffness of a soft tissue allograft made from a single loop of tibialis tendon are greater than the bone plug grafts.20
The disadvantages of the use of soft tissue allograft center around cost, healing, and disease transmission. Soft tissue allografts generally cost a few hundred dollars less than the bone plug allografts. The added cost of the allograft may be offset to some degree by shortened operating time, less physical therapy, and quicker return to work. It is generally accepted that allografts require more time to incorporate and heal than an autograft.29 The longer time for graft incorporation with the allograft places greater demand on the performance of fixation devices that need to provide sound fixation properties over a longer period of time. The use of allograft has an inherent possibility of transmitting an infectious disease from the donor to the recipient. Although the risk is low, HIV, hepatitis, and bacteria have been transmitted through the use of allograft tissue and there is also the theoretical possibility of transmitting slow viruses (prions).30 Newer screening tests such as polymerase chain reaction (PCR) and nucleic acid testing (NAT) improve the detection of viral and bacterial DNA and RNA and may increase the accuracy of identifying infected donor tissue by minimizing the incidence of false-negatives and therefore the risk of disease transmission. Currently, tissue banks do not routinely perform PCR or NAT testing on allograft tissue. Irradiation of allograft tissue has been used to sterilize the tissue and lessen the risk of disease transmission. However, the high dose of irradiation (3 Mrad) required to sterilize allograft tissue also decreases the biomechanical properties of the allograft and does not prevent transmission of hepatitis when a bone plug allograft is used.31 There are no studies showing that cryopreserved allograft performs better than a fresh-frozen allograft, which is not surprising since few donor cells survive the cryopreservation process and none survive the transplantation. The viability of a cryopreserved and fresh-frozen allograft depends solely on repopulation of the allograft with cells from the recipient.32,33
Although infection is rare, surgeons must counsel their patients on the risks and benefits of the use of allograft tissue. The use of a reputable tissue bank that follows state of the art procurement, testing, and preservation guidelines should improve the safety of allograft tissue. In our practices, we consider the use of allografts in patients requiring revision ACL surgery, treatment of unstable knees with multiple ligament injuries, and in patients that request allograft for a primary ACL reconstruction because they wish to avoid the morbidity of graft harvest.
Fixation Devices
A variety of fixation devices for soft tissue grafts exist for ACL reconstruction. The principles of fixing a soft tissue graft include the use of fixation devices that have high strength, high stiffness, resist slippage under cyclic load, promote biologic incorporation of the soft tissue graft at the bone tunnel interface, and safely allow aggressive rehabilitation. In the femur, we use the Bone Mulch Screw femoral crosspin because of its high strength of 1,126 N, high stiffness of 225 N/mm, and resistance to slippage.5,9 In the tibia, we use the WasherLoc because of its high strength of 905 N, high stiffness of 248 N/mm, and resistance to slippage.5,6,9 The use of this combination of fixation devices and a DLSTG autograft or tibialis allograft allows the use of aggressive rehabilitation and a safe return to sports at 4 months.7,34
When choosing a fixation device the surgeon should consider whether the device enhances or retards the healing of a soft tissue graft to the bone tunnel. Tendons heal slower to a tunnel wall than a bone plug, and the healing isn’t equivalent until 6 weeks after implantation.1 Because healing of a soft tissue graft to a bone tunnel requires more time than healing of a bone plug to a bone tunnel, the fixation devices used with a soft tissue graft must be stronger, stiffer, and work for a longer period of time.2,9
Several controllable factors promote healing of a soft tissue graft to bone including lengthening the tunnel,35 avoiding the insertion of fixation devices between the soft tissue graft and tunnel wall (i.e., interference screw),3 increasing the tightness of fit,35 and adding biologically active tissue (i.e., periosteum, bone).36 Lengthening the tunnel and avoiding the insertion of an interference screw requires that the fixation device be placed at the end or outside the tunnel away from the joint line. Several studies have advocated fixation of a soft tissue ACL graft at the joint line with an interference screw to shorten the graft and increase stiffness.37,38,39 A disadvantage of joint line fixation is that the rate of tendon graft-to-bone healing is slower than distal fixation because the interference screw blocks healing between the ACL graft and the tunnel wall.3,40,41 Other studies have shown that distal fixation with the Bone Mulch Screw and WasherLoc provides even greater stiffness than joint line fixation with a wide variety of metal and bioabsorbable interference screws, even though the graft is longer.4,5,6,9 An advantage of distal fixation is that bone graft can be used as a supplementary fixation device. Bone graft in the form of drill reamings can be compacted into the femoral tunnel through a channel in the body of the Bone Mulch Screw, which increases stiffness 41 N/mm9 and allows reciprocal tensile behavior in the graft.21 A bone graft made from a dowel of cancellous bone harvested from the tibial tunnel with a coring device can be compacted back into the tibial tunnel in a space between the anterior surface of the soft tissue graft and WasherLoc and the tunnel wall, which increases stiffness 58 N/mm.42 Tightening the fit by adding an autogenous bone graft or a biologically active tissue such as periosteum improves the rate of healing of a soft tissue graft to a bone tunnel.35,36
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree