Ulna Shortening for Impaction Syndrome
John M. Rayhack
Indications
Ulnar Impaction
Ulnar shortening (1,2,3,4,5,6) is typically indicated for patients with an ulnar impaction syndrome resulting from a positive ulnar variance. Impaction commonly results from a distal radial fracture associated with subsequent metaphyseal subsidence. Radiographic demonstration of cystic involvement of the lunate owing to chronic impaction frequently accompanies this positive ulnar variance (Fig. 41-1).
Triangular Fibrocartilage Tears
Lunotriquetral Ligament Tears
Patients with lunotriquetral ligament tears may also be candidates for ulnar shortening in lieu of lunotriquetral fusion or capsulorrhaphy (9,10). Magnetic resonance arthrograms may clearly demonstrate occult ligament tears that are not necessarily associated with lunotriquetral joint instability that would necessitate a more aggressive procedure such as a lunotriquetral arthrodesis.
Essex Lopresti Injuries
Patients who have sustained Essex Lopresti injuries with radial head resection or arthroplasty with subsidence are also considered candidates for ulnar shortening, although further proximal radial migration could contribute to a resultant secondary ulnar-positive variance (11).
Madelung Deformity
Minimal Radioulnar Degenerative Arthritis
Minimal osteoarthritis of the distal radioulnar joint may also be treated by an ulnar-shortening osteotomy. Changing the contact area of the radial–ulnar articular surfaces with an ulnar-shortening osteotomy may provide pain relief (13).
Radial Malunion
Patients with a radial malunion undergoing a radial metaphyseal osteotomy and grafting may maintain an ulnar-plus variance intraoperatively owing to the effect of soft-tissue constraints and, thus, may be considered for a concurrent ulnar-shortening osteotomy (14,15).
Radial Malunion in the Elderly with Positive Ulnar Variance
Elderly patients with settled radial malunions and moderate radial articular dorsiflexion with resultant positive ulnar variance may be candidates for ulnar shortening. Ulnar shortening may provide the patient with significant ulnar-sided pain reduction and increased functionality.
Contraindications
Absolute
Significant osteoarthritis of the distal radioulnar joint is an important contraindication to ulnar shortening.
Relative
Cigarette smokers are at risk for delayed union and nonunion (16). Teenagers with open radial and ulnar physes may be questionable candidates for ulnar shortening unless their potential for additional growth can be anticipated and calculated into the amount of planned ulnar shortening.
Preoperative Preparation
Ulnar Variance
Ulnar variance is established by obtaining a posteroanterior (PA) radiograph with the arm abducted, elbow flexed at 90 degrees, and the forearm at neutral rotation. Because the variance will increase with pronation activities, it is advisable to achieve a final variance of negative 1 to 2 mm.
Technique
Instrumentation (Rayhack® Ulnar Shortening System, Wright Medical Technology, Inc. Arlington, TN)
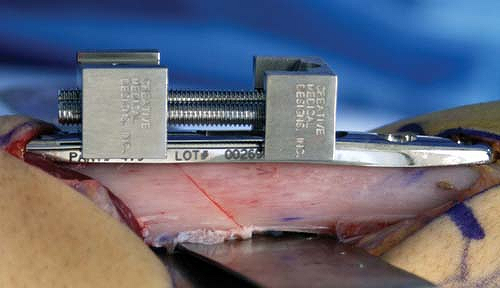
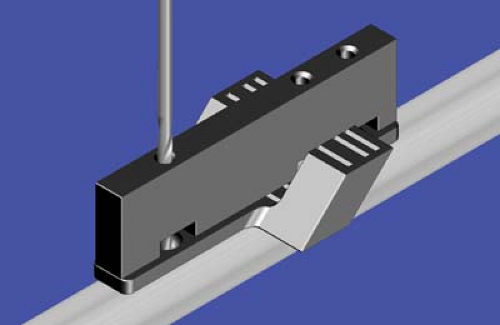
The Rayhack® Generation II surface mount saw guide (Fig. 41-3) or traditional Generation I wraparound ulnar saw guide permits the performance of precise 45-degree oblique osteotomies resulting in ulnar shortenings of 3.5 to 18.1 mm. With the surface mount Generation II saw guide, the surgeon has the option of placing the guide on either the volar–ulnar, or ulnar–subcutaneous surface. The author has no personal experience with dorsal application advocated by some surgeons. The low-profile Generation II compression device (Fig. 41-4) that snugly straddles the plate provides for significant compression capabilities without the potential for rotatory abnormalities.
Position
Position the patient supine with the elbow resting on the table with fingers held vertically toward the ceiling. Right-handed surgeons sit between the extremity and the patient’s body for a left ulnar shortening and between the extremity and the patient’s head for a right ulnar shortening. Left-handed surgeons will find it easiest to sit between the patient’s head and extremity for a left ulnar shortening and between the extremity and the patient’s body for a right ulnar shortening. This position also enables clear visualization of the blade in the proximal to distal orientation of the sagittal saw while performing the osteotomy.
Incision
Make a 10-cm incision along the ulnar subcutaneous border between the extensor carpi ulnaris and the flexor carpi ulnaris.
Retract soft tissues and make a periosteal incision to reflect the periosteum from the ulna. Soft tissues must be protected at all times, particularly at the site of the intended osteotomy. A malleable Davis brain retractor may be placed around the ulna at the site of the intended osteotomy. This added protection should assure that all structures, including the ulnar nerve and artery and the flexor and extensor tendons, are protected at all times.
Saw Guide Placement
The distal end of the plate should be approximately 3 cm proximal to the distal ulnar articular surface. The ulnar subcutaneous surface is slightly convex, but plate placement is easily accomplished despite the absence of a completely flat surface. Surgeons desiring a more protected location may chose to place the plate anteriorly on the ulnar surface. Slightly more soft-tissue retraction is required during the osteotomy process if this volar location is chosen.
The ulnar plate may be first placed on the ulna and marked to assure appropriate location for the saw guide placement (Fig. 41-5). Align hole no. 2 of the surface mount saw guide over this mark.
After applying the straight drill guide on the saw guide surface, drill hole no. 2 with a 2.5-mm drill bit (Fig. 41-6).
Apply a 3.5-mm cortical screw of appropriate length after measuring and tapping the screw hole (Fig. 41-7). Self-tapping screws are generally avoided because of the concern of the screw cutting a new bone thread as a result of subsequent screw removal and reinsertion.
Reinsert the straight drill guide to permit drilling of hole no. 4 (Fig. 41-8).
Insert a 3.5-mm cortical screw after measuring and tapping the hole (Fig. 41-9).
Accomplish final fixation of the saw guide with application of screw no. 3 (Fig. 41-10).
Planning and Performing the Osteotomy
Use preoperative radiographs to determine the intended amount of ulnar shortening and chose the appropriate slots from the graphic (Table 41-1).

Figure 41-5 Provisional placement of the plate on the ulna with marking to assure appropriate location for the saw guide placement.
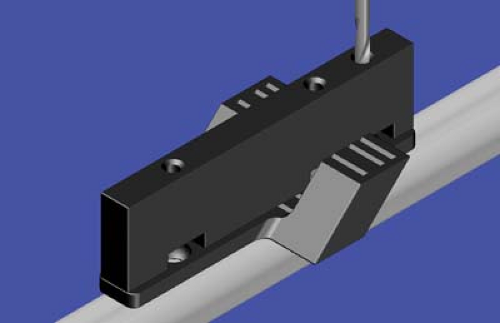
Figure 41-6 Straight drill guide applied on the saw guide surface with 2.5-mm drill bit drilling of hole no. 2.

Figure 41-7 A 3.5-mm cortical screw of appropriate length applied after measuring and tapping screw hole no. 2.

Get Clinical Tree app for offline access