Triple Arthrodesis of the Hindfoot
James D. Michelson
A triple arthrodesis is classically described as the fusion of the subtalar, calcaneocuboid, and talonavicular joints (1, 2, 3 and 4). Anatomically, the fusion involves four bones (calcaneus, talus, navicular, and cuboid), so, technically, the fusion also includes four joints. The joint that is omitted in most discussions is the navicular-cuboid, which is a true synovial articulation. The goals of the surgery are multiple:
Provide hindfoot stability
Restore hindfoot alignment
Relieve pain
INDICATIONS AND CONTRAINDICATIONS
The indications for a triple arthrodesis can be segregated into the same categories:
Hindfoot arthritis: that is, rheumatoid arthritis, osteoarthritis, posttraumatic arthritis, and adult symptomatic tarsal coalition (5,6)
Hindfoot instability: that is, posterior tibialis tendon (PTT) dysfunction or rupture, neuromuscular diseases such as Charcot-Marie-Tooth disease (7,8)
Hindfoot malalignment: that is, valgus secondary to ruptured PTT; varus secondary to peroneal tendon dysfunction or PTT overpull (stroke)
Typically, patients have more than one indication for surgery (e.g., both instability and pain). Arthrodesis should be reserved for instances in which all conservative measures have failed. In cases involving hindfoot deformity or instability, consideration should be given to motion-sparing procedures, such as tendon transfers or osteotomies or limited hindfoot arthrodeses, before deciding on a triple arthrodesis. If only one of the three joints is the source of clinical symptoms, that specific joint usually should be fused rather than doing a triple arthrodesis. However, if two of the hindfoot joints are symptomatic, fusing all three joints often is preferable because the functional consequences of fusing two joints are about the same as fusing three, whereas fusing only two carries a higher risk of clinically significant nonunion.
A contraindication is a patient with inadequate vascular supply to the foot; appropriate evaluation and vascular specialist referral may be indicated. Advanced patient age is not a contraindication for surgery, nor is the presence of diabetes mellitus, although it has implications for the postoperative regimen.
PREOPERATIVE PLANNING
The history and examination are useful in providing clues to the diagnosis and to indicate the specific concerns that need to be treated. A routine foot and ankle physical examination should be undertaken. Observing the patient’s gait can reveal the functional derangements potentially causing symptoms. The patient should be observed for signs of an antalgic gait. The inability to perform a single-leg heel rise is a reliable test for posterior tibial tendon dysfunction. Observing the patient
in a standing position anteriorly and posteriorly generally demonstrates the deformity (Fig. 24.1). A cavus foot should raise suspicion about an underlying neuromuscular cause, such as Charcot-Marie-Tooth disease or a spinal lesion.
in a standing position anteriorly and posteriorly generally demonstrates the deformity (Fig. 24.1). A cavus foot should raise suspicion about an underlying neuromuscular cause, such as Charcot-Marie-Tooth disease or a spinal lesion.
 FIGURE 24.1 Severe hindfoot valgus is observed in both feet. Abduction of the forefoot produces the “too many toes” sign. |
Whether the foot is plantigrade, meaning that it contacts the floor in a physiological manner, should be determined. The non-weight-bearing examination focuses on the measurement of ankle and hindfoot range of motion and stability. It is useful to determine painful joint motions, numbness, swelling, and the presence of callosities in the medial or lateral forefoot associated with malalignment and deformities such as claw toes. Muscle strength testing, sensation assessment, and palpation of pulses should be part of the examination.
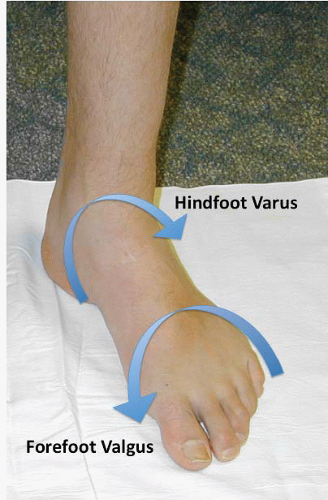
The varus hindfoot seen in a cavus foot is usually associated with a compensatory valgus forefoot deformity and an adducted forefoot (Fig. 24.2). In the more common pes planus from posterior tibial dysfunction, the hindfoot is in valgus, and the forefoot has a compensatory varus-abducted deformity. Generally, these compensatory deformities occur through the Chopart joint and can be
corrected with the triple arthrodesis without the need for additional surgery in the anterior foot. There may also be a secondary Achilles tendon contracture due to the valgus, laterally deviated calcaneus which places the Achilles tendon in a shortened position. This can be ascertained by the Silfverskiöld test, in which ankle dorsiflexion is significantly limited when the knee is extended. In a rigid valgus hindfoot, with the talus locked in a plantarflexed position, this contracture sometimes cannot be definitively determined preoperatively, but restricted dorsiflexion of the ankle should be ascertained intraoperatively using the Silfverskiöld test. Inadequate dorsiflexion due to tendon contracture may require a partial gastroc lengthening or, rarely, a formal tendo-Achilles lengthening. This should be discussed preoperatively with the patient.
corrected with the triple arthrodesis without the need for additional surgery in the anterior foot. There may also be a secondary Achilles tendon contracture due to the valgus, laterally deviated calcaneus which places the Achilles tendon in a shortened position. This can be ascertained by the Silfverskiöld test, in which ankle dorsiflexion is significantly limited when the knee is extended. In a rigid valgus hindfoot, with the talus locked in a plantarflexed position, this contracture sometimes cannot be definitively determined preoperatively, but restricted dorsiflexion of the ankle should be ascertained intraoperatively using the Silfverskiöld test. Inadequate dorsiflexion due to tendon contracture may require a partial gastroc lengthening or, rarely, a formal tendo-Achilles lengthening. This should be discussed preoperatively with the patient.
 FIGURE 24.3 The talometatarsal angle can be measured on the AP (A) and lateral (B) views of the foot. In both projections of a normal foot, the angle should be close to 0°. |
All patients should have weight-bearing radiographs of their feet and ankles: anteroposterior foot, lateral foot, and anteroposterior ankle views. In the flatfoot, the anteroposterior (Fig. 24.3A) and lateral talocalcaneal angles (Fig. 24.3B) diverge, whereas in the cavus foot, these angles tend to be parallel or converge. The ankle radiographs are necessary, as they can reveal calcaneofibular impingement (which is not unusual) and significant arthritis (Fig. 24.4). Failure to appreciate these preoperatively can lead to an unhappy outcome because of persistent ankle complaints. The weight-bearing ankle radiographs also provide insight into the overall alignment of the lower extremity.
Although the usual goal for a triple arthrodesis is a plantigrade foot, the optimal position of the foot has to be determined with respect to the entire lower extremity. In those cases in which proximal deformity will also be corrected (e.g., total knee arthroplasty, tibial osteotomy), the interaction of the proximal realignment on ultimate plantigrade position must be anticipated to prevent the foot from being placed into too much valgus or varus by the triple arthrodesis. Computed tomography, radioisotope bone scanning, and magnetic resonance imaging usually are unnecessary for preoperative assessment. Selective joint injections with a long-acting local anesthetic (e.g., mepivacaine [Carbocaine], bupivacaine [Marcaine]) are occasionally useful diagnostically to help determine the most symptomatic joints.
Autograft bone graft, which may not be needed, can be obtained from the iliac crest or proximal tibia, or demineralized bone graft allograft (250- to 400-μm particles) can be used (9). The latter has the advantage of avoidance of an additional, sometimes painful, incision with attendant blood loss, and it carries no risk of viral infection transmission. The union rates for grafting technique are equivalent.
The goals and limitations of surgery should be discussed with the patient. Patients’ expectations must be realistic, or they are likely to be unsatisfied with the result.
SURGICAL TECHNIQUE
Every effort should be made to use sharp dissection and to gently handle the soft tissues. The approach is made with a minimum of blunt dissection and avoidance of raising subcutaneous skin flaps. The closure should be performed carefully. The use of 5-0 chromic sutures for skin closure has been found to yield excellent cosmetic results. While a Surgairtome (or equivalent) with a 5-mm-long shaft, pineapple-shaped cutting burr can be used for the debridement of cartilage and subchondral bone, the possibility of thermal necrosis is avoided by using a light touch with the burr. Alternatively, one can choose to use sharp osteotomes (straight and curved), curettes, and rongeurs to debride the joint surfaces. The tourniquet can be placed on the upper calf with adequate soft roll padding to protect the common peroneal nerve as it wraps around the proximal fibular head. This allows use of lower cuff pressures, typically 250 mm Hg, and results in less ischemic tissue compared with the use of thigh tourniquets. In addition to the usual surgical skin preparation and draping, it is generally easiest to drape the surgical field using a stockinette and an extremity drape that is reversed so that the long end of the drape is unfolded cephalad. The stockinette can be opened distally and rolled proximally, and the toes and forefoot can be covered using a surgical glove or iodine adhesive plastic. This reduces the potential for contamination of the surgical field from debris adjacent to the toenails. The exposed skin is covered with an iodine adhesive plastic to reduce skin contamination of the wound. Preoperative antibiotics are administered.
The patient is placed in a semilateral decubitus position by pacing the towel roll under the ipsilateral buttock. This internally rotates the leg to permit easier access to the lateral hindfoot. The tourniquet is placed on the upper calf, with underlying soft roll padding. The leg is exsanguinated using an elastic wrap, and the tourniquet is inflated to 250 mm Hg.
The operation is accomplished through two incisions: the dorsal lateral sinus tarsi incision for the subtalar, calcaneocuboid, and lateral talonavicular joints, followed by the dorsomedial approach to the talar neck and medial talonavicular joint. The surgeon sits at the lateral side of the foot.
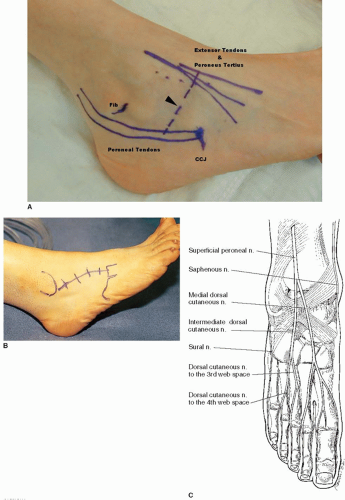
The calcaneocuboid joint and talonavicular joint are palpated externally and marked (Fig. 24.5). The intermediate branch of the superficial peroneal nerve can frequently be palpated as it runs over the anterior lateral aspect of the ankle and runs inferiorly and laterally over the region of the sinus tarsi. The extensor tendons dorsally and the peroneal tendons posterolaterally should be palpated and marked, as should be the inferior aspect of the lateral malleolus (Fig. 24.5A). The incision runs obliquely along the lines of Langer from the peroneal tendons posterolaterally to the lateral margin of the extensor tendons.
An alternative, incision runs from 1 cm distal to the fibula toward the base of the fourth metatarsal (Fig. 24.5B). This approach has the advantage of completely avoiding the intermediate branch of the superficial peroneal nerve, to which it runs parallel. With this incision, the talonavicular joint can be exposed, although not as easily as with the dorsal lateral sinus incision. However, the talonavicular joint can be exposed through a separate dorsal medial incision. Trauma to the intermediate branch of the superficial peroneal nerve using the oblique sinus tarsi incision can occur. If there is concern regarding damaging the nerve, the alternative longitudinal incision is a good option.
The incision is made sharply through the skin and subcutaneous tissues with a scalpel and Littler scissors, taking care to isolate and coagulate the traversing veins. The intermediate branch of the superficial peroneal nerve is frequently encountered and can be retracted superiorly through the remainder of the approach.
The fascia investing the extensor hallucis brevis (EDB) is sharply incised along the lines of the original skin incision (Fig. 24.6). Care is taken at the upper and lower boundaries of this incision to not incise the peroneus tertius and peroneal tendon sheath, respectively. The EDB muscle attachment to the calcaneus can be sharply dissected and raised as a distally based flap, or alternatively, the EDB muscle can be detached using electrocautery. The preservation of the fascia of the EDB and its muscle belly is useful in preparation for the ultimate wound closure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree