Tarsometatarsal Arthrodesis
Andrew L. Merritt
Bruce J. Sangeorzan
Sigvard T. Hansen Jr
The tarsometatarsal (TMT) or Lisfranc joints consist of complex articulations between three cuneiform bones, the cuboid, and the bases of all five metatarsal bones. The joints have differing amounts of stability and normal motion because of the bony anatomy and the ligamentous restraints. The joints are generally separated into two groups based on stability: the medial three joints that are more stable with limited motion and the lateral two joints that are relatively mobile. Arthritis of the TMT joints can occur, with the medial joints more commonly affected than the lateral two. Arthritis is usually secondary to trauma, inflammatory arthritis, or Charcot arthropathy and is rarely a result of primary osteoarthritis (1, 2 and 3). Other contributing factors to the development of arthritis include a tight heel cord causing secondary midfoot breakdown or a short first ray and a long second ray (4). In both cases, the normal mechanics of the midfoot are altered with increased force concentrated in the TMT joints.
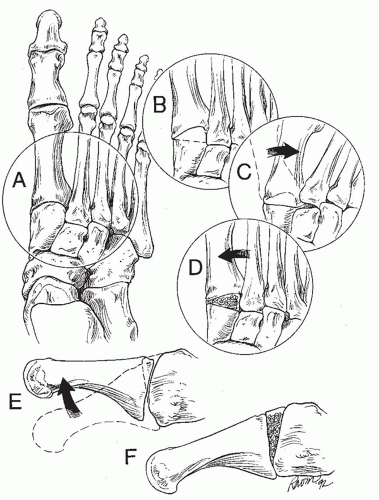
The habitus of a normal lower limb is slightly externally rotated, and the center of mass of the body is in the midline, medial to the foot. During toe-off, the body weight acts medially to the foot to push the forefoot outward. If arthritis develops in the TMT joints, this continued pressure on the forefoot leads to erosion of the dorsal and lateral aspects of the cuneiforms and progressive valgus deformity (Fig. 18.1). This leads to the patient’s complaint of foot deformity and pain during walking. On exam, this can be assessed by evaluating the abduction of the forefoot during heel rise or toe-off. The valgus midfoot alignment is evident on exam, and often there is a deformity over the medial border of the foot due to the malaligned valgus first metatarsal.
History, symptoms, and findings consistent with TMT arthritis:
History of midfoot trauma or systemic inflammatory arthritis
Pain and instability of the midfoot during the propulsive phase of gait, often worse when walking uphill or on stairs. The pain is usually medial and involves the first to third TMT joints more than laterally.
Foot fatigue with ambulation
Complaint of “foot turning outward” or “a bump along the inside of the foot.” The patient can have trouble with shoe fit due to this deformity.
Deformity at the midfoot
Abduction of the forefoot with gait or heel rise
Decreased sensation in the foot if due to Charcot arthropathy
When clinically important arthritis or instability develops in the TMT joints, nonoperative treatment may be effective in relieving short-term symptoms or an acute exacerbation of chronic symptoms (5). Since there is no current treatment for joint arthritis, nonoperative management is palliative not curative. Nonsteroidal anti-inflammatory drugs (NSAIDs) can be helpful in the short run, but extended use is concerning due to systemic side effects. The main strategy for nonoperative treatment is external support that decreases the forces across the TMT joint. In the short term, this can be achieved by a cast, but this treatment is not durable. If the cast is effective and the patient finds it cosmetically acceptable, a custom-molded polypropylene clamshell orthosis may be an acceptable treatment. A rocker-bottom sole can also be very effective, but both of these treatments are not aesthetic, making compliance unpredictable. More cosmetically acceptable options are stiff carbon fiber or metal shanks in the shoe. All of these options can be effective in decreasing pain and improving the instability, but function is often inadequate in the long term for an active person.
INDICATIONS AND CONTRAINDICATIONS
Indications
Surgical treatment of TMT arthritis is indicated when pain and instability develop that affect daily living. Usually the patient has tried and failed conservative management. Arthrodesis is the currently established salvage procedure for TMT arthritis involving the medial three joints. The fourth and fifth TMT joints are frequently involved in the abduction deformity of the forefoot, and they need to be corrected if malaligned. Correction of these joints is performed without fusion, if possible. Unlike the medial three TMT joints, the fourth and fifth TMT joints are mobile during normal gain so realignment should be done without restricting the motion through arthrodesis. In selected patients, primary tarsometatarsal arthrodesis is indicated for severe Lisfranc fracture dislocation injuries (6,7). The role of arthrodesis for primarily ligamentous Lisfranc injury is unclear (8).
Contraindications
Inadequate soft tissue envelope
Inadequate arterial inflow
Inability to be non-weight bearing postoperatively
Relative Contraindications
Perioperative smoking
PREOPERATIVE PLANNING
The preoperative planning for TMT joint arthrosis involves the following components:
Appropriate weight-bearing x-rays of the affected and contralateral foot
Arterial evaluation for adequate inflow
Venous evaluation for patency
Evaluation of social parameters that will effect healing such as the need to stop smoking in the perioperative time, ability to be non-weight bearing for 3 months, assistance in activities of daily living, and need for a posthospital nursing home
Maximizing of perioperative health, especially diabetes and nutrition
Selection of the appropriate joints to be addressed including if any intercuneiform joint fusions are required
Preoperative templating and evaluation of the bony defect and need for structural bone graft
Radiographic examination is critical in the evaluation and treatment planning for patients with midfoot pain and deformity. The views include full-weight-bearing anteroposterior (AP), lateral, and oblique views. The AP view is aligned perpendicular to the medial TMT joints, and the oblique view is aligned perpendicular to the lesser TMT joints, acting as an “AP” of the fourth and fifth TMT joints. Sometimes it is useful to obtain multiple oblique views. The films must be full weight bearing; otherwise, it is impossible to determine the severity of the midfoot collapse. Also, weight-bearing films are required to determine the amount of correction that is required, particularly in the dorsoplantar direction. Contralateral films are required for comparison preoperatively and in the operating room to assess the deformity reduction. With advanced arthritis resulting in bony erosions, it can be difficult to assess alignment without comparison to the other side. Since TMT arthritis is often unilateral because of the posttraumatic etiology, the contralateral foot often has no TMT deformity and is therefore the best guide of reduction.
Fluoroscopy can be used to evaluate instability and motion in the TMT and intercuneiform joints, but this assessment is generally not necessary. Computed tomography (CT) is generally not required, but it may be useful in sorting out problems in joints that are difficult to visualize with plan film radiography, such as the intercuneiform joints. Magnetic resonance imaging (MRI) is not indicated for planning but may be helpful in rare cases for diagnostic purposes.
Vascular evaluation of the foot requires assessment of the arterial inflow and the venous outflow because both effect healing. Patients with TMT arthritis are usually elderly and often have diabetes mellitus, which can damage the arterial inflow. Dorsalis pedis and posterior tibial pulses are evaluated, and if both are palpable, then it is safe to proceed with surgery. The dorsalis pedis is at risk during surgery and may be injured during the approach or with the reduction, so the presence of a patent posterior tibial artery is essential. If no pulse is palpated in the posterior tibial artery, then a preoperative consultation with a physician specializing in vascular disorders is requested regardless of the presence of a dorsalis pedis pulse. At the direction of the vascular physician, formal ankle-brachial
indices (ABIs) using ultrasonography and/or transcutaneous oxygen tension tests are performed to evaluate for adequate arterial flow for healing. In addition, ultrasonography can be used to evaluate for anomalous vascular anatomy. Venous patency is usually evaluated clinically. If there is significant venous stasis that compromises the soft tissue of the foot, then surgery would be contraindicated.
indices (ABIs) using ultrasonography and/or transcutaneous oxygen tension tests are performed to evaluate for adequate arterial flow for healing. In addition, ultrasonography can be used to evaluate for anomalous vascular anatomy. Venous patency is usually evaluated clinically. If there is significant venous stasis that compromises the soft tissue of the foot, then surgery would be contraindicated.
Social factors are very important to address preoperatively. It is difficult for elderly patients to be non-weight bearing for at least 6 weeks as is required for this surgery. If surgery is required, they may require a skilled nursing facility or in-home care. They must have a caretaker at least at the beginning of the recovery before reliably mobile on assistive devices. It is also important to have the patient’s other medical comorbidities optimized prior to surgery and have diabetes mellitus under good control to decrease the risk of infection. Finally, we determine perioperative smoking to be a contraindication to this procedure, and this must be addressed before deciding on operative management.
The first, second, and third TMT joints are almost always affected and require treatment, but surrounding joints may also contribute to the pain and deformity. The fourth and fifth TMT joints are often involved in the deformity, and they may need to be temporarily immobilized to aid healing after the realignment procedure.
The joint between the medial and intermediate cuneiform is often a contributor to pain and may require fusion. This joint has more motion that in generally recognized and is a frequent site of occult injury. Careful examination of this joint may reveal whether it is involved or not. To examine this joint, stabilize the midfoot with one hand, and grasp the first metatarsal head with the other. Passive plantarflexion and dorsiflexion of the first ray will cause pain in the midfoot if the intercuneiform joint is arthritic. In addition, lateral weight-bearing x-rays may demonstrate extension of the cuneiform, which can suggest instability of the intercuneiform joint and a possible etiology for midfoot pain. If there is any question about the contribution of the intercuneiform joint with the symptoms, selective injection of lidocaine into the joint may be helpful. The use of a miniature fluoroscopy unit can help document that the needle is placed accurately in the joint. If there is still some uncertainty after selective injection, we generally fuse the joints we suspect are related to the painful symptoms. The additional work required to fuse an extra joint is limited, and the loss of motion is negligible. Fusion of an additional intertarsal joint seems preferable to continuing pain or having to do a secondary fusion.
Planning the correction is critical prior to surgery and includes templating the deformity on x-ray. Using the AP and lateral weight-bearing radiograph views, a tracing is made that includes the lateral three rays. The metatarsals are cut out and the articulations are reduced into the appropriate position as compared to the contralateral film. It is necessary to restore the anatomic position and length, and using this template, it will become evident if a corticocancellous bone graft is needed. Planning also helps give the surgeon a good idea of the amount of reduction that will be required.
SURGICAL TECHNIQUE
The following technique describes an arthrodesis of the medial three TMT joints due to arthritis with significant bony erosion of the medial cuneiform. In this incidence, the fourth and fifth TMT joints are subluxed as part of the deformity, but the joints have minimal arthritis and are salvageable. No cuneiform fusions are required. Additional considerations are considered in the next section.
Exposure and Debridement
The patient is supine on a radiolucent operating room table with a small roll beneath his hip on the operative side. All bony prominences are well padded. A pillow is placed beneath the knee to allow the ankle to plantarflex. The patient’s entire leg is prepped to include the iliac crest for autogenous bone graft.
The pulses are again evaluated and its relationship to the first web space is documented. The limb is exsanguinated using an Esmarch bandage, and a sterile tourniquet is inflated.
The primary dorsal incision is marked over the second ray that permits access to the first through third TMT joints (Fig. 18.2). An incision is drawn medially on the foot over the medial first TMT joint that may be used if the reduction is problematic. A more lateral incision is planned over the medial border of the fourth metatarsal to allow exposure of the third, fourth, and fifth TMT joints. Ensure enough separation between the three incisions.
The dorsal incision over the second ray is made, and the superficial peroneal nerve is identified and protected. The dorsalis pedis artery and the large branch of the first proximal perforating artery are identified and carefully protected (Fig. 18.3).
The first and second TMT joints are identified and debrided of scar tissue using a small rongeur and curette.
The more lateral incision is made, the lateral three TMT joints are identified, and scar tissue is similarly debrided. The medial three joints are completely debrided of articular cartilage and subchondral bone (Fig. 18.4). Once all of the scar tissue and affected articulations are debrided, the reduction is performed.
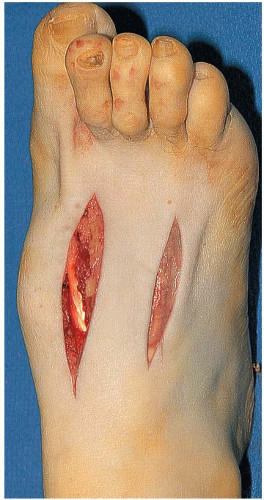 FIGURE 18.2 Surgical approach. The dorsal surface of a right foot is shown. Notice the medial dorsal deformity. The incisions allow access to two TMT joints each. |
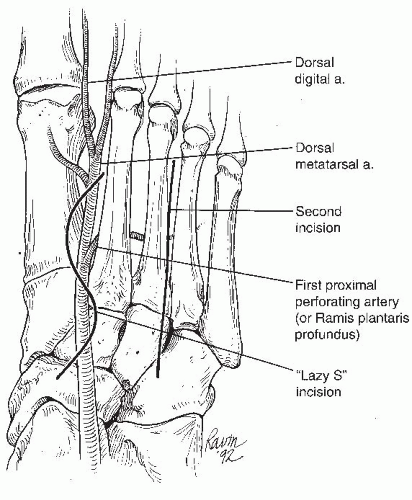 FIGURE 18.3 Dorsal view representing the location of the skin incisions and perforating arteries. The lazy-S incision is represented by a line
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|