A variety of lesser toe (i.e., toes two through five) deformities, such as the hammer toe, claw toe, crossover toe, mallet toe, and metatarsophalangeal dislocation may be associated with pain, stiffness, and footwear restrictions. Although much attention has been focused on the treatment of problems of the great toe (e.g., hallux valgus, hallux rigidus, hallux varus), conditions affecting the lesser toes often cause severe, debilitating symptoms even when there is no association with a hallux problem. Deformities of the lesser toes may involve the metatarsophalangeal (MTP) or interphalangeal (IP) joints or both and may involve single or multiple digits. The incidence of pain and impairment due to second MTP synovitis and MTP joint instability and dislocation has become more evident in recent years.
The many causes of lesser toe deformities include neuromuscular diseases and peripheral neuropathies such as Charcot-Marie-Tooth disease, connective tissue diseases, inflammatory arthritides (e.g., rheumatoid arthritis, Reiter’s disease, psoriatic arthritis), traumatic injuries, compartment syndrome, congenital anomalies, and iatrogenic causes. Anatomic factors and constricting footwear also play roles in the development of lesser toe disorders. A long second toe is at risk for becoming a mallet toe or hammer toe. Irregularity in the shape of the middle phalanx can cause deviation of the distal phalanx. Extrinsic pressure of the hallux against the second toe may result in hammer toe deformity, subluxation, or dislocation of the MTP joint.
Choosing the appropriate surgical procedure for individual disorders can be difficult, and recommendations in the literature often are conflicting. Elements from several soft tissue and bony procedures are usually combined to completely correct the deformity. Treatment should aim to restore function to the lesser toes, to alleviate pain, and to allow a reasonable variety of footwear. Thorough evaluation and careful treatment choices can achieve these aims in most patients with lesser toe disorders, remembering that these problems often are multiplanar and complete correction of the deformity while restoring full motion of the joints of the involved digit may not be possible. Before surgery, patients must be made aware of the complexity of these seemingly straightforward disorders.
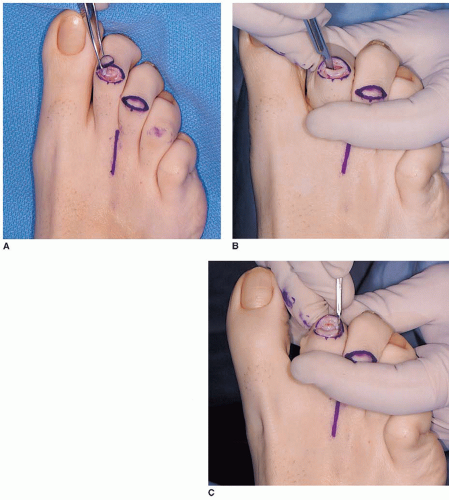
The term hammer toe is used most often to describe an abnormal flexion posture of the proximal interphalangeal (PIP) joint of one of the lesser four toes (
1). The flexion deformity may be fixed (i.e., not passively correctable to the neutral position) or flexible (i.e., passively correctable). If the flexion contracture at this middle joint of the digit is severe and of long enough duration, the MTP joint becomes deformed in the opposite direction (i.e., extension or dorsiflexion), which may lead to MTP subluxation and dislocation. The distal interphalangeal joint (DIP) may stay supple, but it too may develop an extension or a flexion deformity.
Claw toe and hammer toe are sometimes used interchangeably, but most providers generally differentiate the deformities by the following:
Claw toes frequently are caused by neuromuscular diseases, and often a similar deformity is present in all toes, whereas a hammer toe deformity usually affects only one or two toes.
Claw toes always have extension deformity at the MTP joint, but in hammer toe deformity, abnormal extension of the MTP joint may or may not be present.
Claw toes often have a flexion deformity at the DIP joint, but this usually does not occur in hammer toes.
Three areas may be painful in lesser toe deformity. The most common area is the dorsum of the PIP joint in the hammer toe and crossover toe or at the DIP joint in the mallet toe (
2). A corn caused by pressure from the toe box or vamp of the shoe develops. When a flexion posture of DIP joint is present, a painful callus will develop just plantar to the nail end. This is called an end-bearing corn (
Fig. 9.1). A painful callus may develop beneath the metatarsal head if the proximal phalanx subluxates dorsally (
3). In patients who have conditions that result in decreased sensibility, such as diabetes mellitus or myelomeningocele, ulceration and deep infection can develop at one or more of these areas of pressure, complicating the treatment plan and endangering the toe or foot.
Nonoperative treatment of lesser toe deformities involves educating patients about appropriate footwear with a softer “upper” and adequate space in the toe box. The upper may also be enlarged over the affected toe with a ring-and-ball stretcher. A silicone sleeve over the toe will reduce the discomfort over the PIP soft corn. A toe crest will relieve discomfort from an end-bearing corn. Shoe inserts are of limited value as they occupy space in the shoe. Manipulating the toes, taping, and strapping may not appreciably alter the alignment or motion.
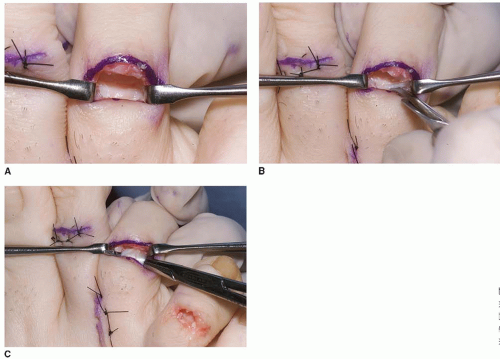
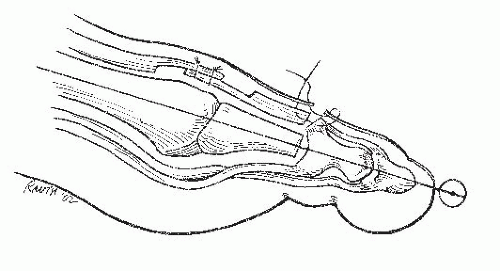
The lesser MTP joints also are affected by these lesser toe deformities. A hammer toe may be associated with dorsal MTP subluxation or complete dislocation (
4,
5,
6,
7 and
8). The joint may deviate in the transverse plane in varus or valgus, called a crossover toe. Long-standing MTP dislocation can lead to chondral erosion, degenerative arthritis, and a dorsal concavity or crater in the metatarsal head where the base of the phalanx is perched. In many instances, the MTP dislocation can be reconstructed and stability restored.
INDICATIONS AND CONTRAINDICATIONS
The indications for surgery are pain, impairment, and difficulty with footwear. Improving cosmetic appearance is not an indication. Most patients who undergo lesser toe deformity correction have joint stiffness at one or more levels and must understand that this stiffness will persist even after successful surgery.
If there is reluctance to comply with appropriate footwear recommendations, surgery should not be considered. If there is a previous failed lesser toe surgery, further surgery may or may not be advisable, and has the potential of creating a flail or floppy toe, or a dysvascular digit. Contraindications include infection, neuropathy, and a dysvascular foot.
A painful, dislocated MTP joint may be successfully reconstructed; however, restoration to a normal condition is uncommon.
PREOPERATIVE PLANNING
It is important to assess the flexibility of the lesser toe deformity with the patient sitting and weightbearing. The toe posture while weightbearing is important as it may more clearly demonstrate the deformity at multiple levels such as flexion at the PIP joint and dorsal subluxation at the MTP joint. Surgery at multiple levels (e.g., PIP and MTP) may be necessary to successfully address more advanced deformities. A limited operation, such as a tenotomy or hemiphalangectomy for a complex toe condition may lead to incomplete correction or early recurrence.
It is important to assess the adjacent toes as well, as they may impact the potential for recurrence and may be part of the underlying cause of the lesser toe problem. Hallux valgus is associated with a higher recurrence rate of second toe deformities. In patients who have hallux and lesser toe malalignment in which both are painful, both conditions should be corrected or the patient should understand the likelihood of recurrent second toe deformity if the hallux valgus is untreated. The local and general medical condition of the patient should be considered in the decision for surgical treatment.
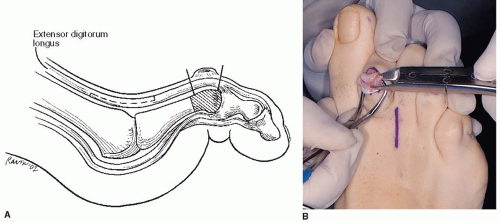
Flexible deformities are often less symptomatic and may not require operative treatment. They may be addressed with loose-fitting footwear with an adequate toe box, patient education, and observation. Rigid deformities are more commonly associated with pain and impairment. The use of soft tissue reconstruction procedures alone such as flexor digitorum longus (FDL) tenotomy may not result in permanent correction of lesser toe deformities (
Table 9.1). However, in selected patients with symptomatic flexible hammer toes that interfere with footwear, operations such as flexor-toextensor tendon transfer may be appropriate.
The most commonly used procedure for the correction of hammer toe is hemiphalangectomy, which involves resection of the condyles of the proximal phalanx. Hammer toe encompasses a spectrum of deformities, and the indicated procedure varies, depending on the stage of the deformity and the diagnosis.
Treatment of hammer toe deformity should focus on the PIP joint and often the MTP joint (
1,
9,
10). Any fixed deformity of the PIP joint exerts a linkage effect at the MTP joint, and maximal active and passive flexion of the MTP joint will slowly decrease. Over a lengthy period, the plantar plate also becomes attenuated. This attenuation decreases the ability of the plantar plate to restrict minor degrees of dorsal subluxation of the base of the proximal phalanx. The stage is set for an instability pattern in the sagittal plane to develop at the MTP joint.
As the base of the proximal phalanx with the first and second dorsal interossei insertions (in the second toe) subluxates dorsally, the flexion moment of the interossei at the MTP joint is decreased because of their normal proximity to the center of rotation of the MTP joint on the metatarsal head. The interosseous tendons pass plantar to this center of rotation. A weakened flexion moment at the MTP joint is further affected by intrinsic and extrinsic extensor forces at the MTP joint, and the MTP joint gradually deforms in extension and eventually becomes fixed. As the MTP joint extends, the flexion forces at the PIP and to some degree DIP joints increase.
Operative treatment usually is performed in patients with lesser toe deformities for pain relief; these symptomatic patients are more likely to have rigid hammer toe without MTP subluxation, rigid hammer toe with MTP subluxation, rigid hammer toe with MTP dislocation, or mallet toe. The operative approach to each is unique and is addressed separately. The crossover toe is discussed separately.