Peroneal Tendon Repair and Reconstruction
Harold B. Kitaoka
Diane L. Dahm
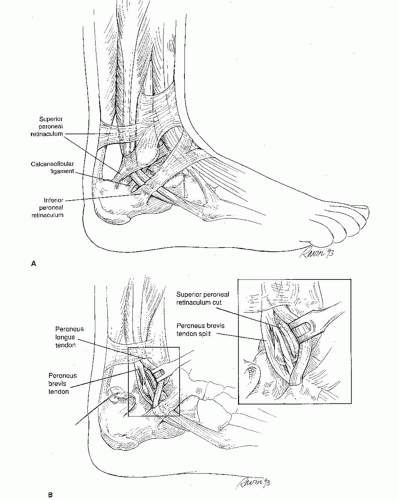
The peroneus longus and peroneus brevis tendons originate in the lateral compartment of the leg and course distally, posterior to the lateral malleolus toward their insertions in the foot. The peroneus longus courses posterior to the peroneus brevis tendon, and both tendons pass through a common peroneal synovial sheath approximately 4 cm proximal to the lateral malleolus. Within this synovial sheath, the tendons pass through a fibro-osseous tunnel at the level of the lateral malleolus. This tunnel is formed by the fibula anteriorly, the superior peroneal retinaculum posterolaterally, and the calcaneofibular and posterior talofibular ligaments medially (Fig. 25.1A). An indentation in the posterior surface of the distal fibula is known as the retromalleolar sulcus. The sulcus is 6 to 7 mm wide and is concave in 82% of fibula specimens (1). At the posterolateral border of the fibula, a 3- to 4-cmlong fibrocartilaginous ridge is typically present, augmenting stability of the tendons within the tunnel.
The superior peroneal retinaculum is formed as a confluence of superficial fascia, peroneal tendon sheath, and distal fibula periosteum, approximately 2 cm proximal to the fibula tip. It is approximately 2 cm wide and is important in maintaining stability of the peroneal tendons. Peroneal tendon dislocation involves stripping of the superior peroneal retinaculum and periosteum from the lateral malleolus, creating a false pouch into which the tendons dislocate. This often occurs from trauma in which there is a sudden dorsiflexion to stress with forceful contraction of the peroneals (2, 3 and 4). Other factors, such as a congenitally shallow retromalleolar sulcus, may contribute to peroneal tendon instability. Chronic peroneal dislocation is often associated with recurrent ankle sprains, which can contribute to incompetence of the superior peroneal retinaculum.
Longitudinal tears of the peroneus brevis may occur at the level of the distal fibula (Fig. 25.1B). These tears are often associated with ankle sprains and typically occur with peroneal subluxation over the fibrocartilaginous ridge of the posterolateral aspect of the distal fibula (5). Other pathologic conditions include peroneal tendinitis or tenosynovitis, which involves inflammation of the tendon and surrounding synovial lining. Complete peroneal tendon rupture is commonly associated with peroneal tenosynovitis and often occurs in locations such as at the level of the retromalleolar sulcus, the peroneal tubercle, and the cuboid groove, where stenosing tenosynovitis is observed (5). A low-lying peroneus brevis muscle belly or an anomalous peroneus quartus tendon may contribute to stenosis within the sheath and subsequent tendon irritation.
Nonoperative management of acute peroneal tendon subluxation or dislocation includes treatment in a short-leg cast with the ankle in neutral to slight inversion for 6 weeks, but this treatment is associated with a 30% to 40% rate of redislocation. Nonoperative treatment of patients with tendinitis or tenosynovitis includes a period of immobilization in a brace such as a walking boot or in a cast, anti-inflammatory medications, activity modifications, and, occasionally, a corticosteroid injection.
INDICATIONS AND CONTRAINDICATIONS
Indications for surgery include an active patient with significant pain and impairment localized to the peroneal tendons.
Contraindications to surgery include infection and severe peripheral vascular disease.
PREOPERATIVE PLANNING
Patients with peroneal tendon subluxation or dislocation often present with a history of a traumatic event involving dorsiflexion and eversion of the ankle but may also report a history of recurrent inversion type of ankle sprain and lateral ankle instability (4,6, 7 and 8). The clinical course may initially be similar to that of an acute lateral ankle ligament sprain, but with time, it may be possible to distinguish ligament from tendon injury. The symptoms and signs of ligament instability are localized to the anterolateral and lateral ankle, whereas with peroneal tendon injuries, they are localized to the posterolateral ankle. There may be obvious ankle instability seen with anterior drawer and inversion stress testing of the ankle in the case of ligament sprains. Patients with dislocating peroneal tendons may be able to voluntarily dislocate the tendons. In some cases, both problems coexist.
On examination, swelling is often observed in the posterolateral ankle and hindfoot along the peroneal tendon sheath. There is tenderness posterior to the lateral malleolus along the peroneal tendons. Subluxation or dislocation of the peroneal tendons may be provoked by active dorsiflexion and eversion. There may be weakness to resisted eversion strength testing, particularly in the setting of significant tendinitis, tenosynovitis, and partial or complete peroneal rupture. Ankle stability should be examined with anterior drawer and inversion stress testing. A diagnostic lidocaine injection into the peroneal tendon sheath can be helpful in confirming the source of pain.
Plain film radiographs of the ankle should include anteroposterior (AP), lateral, and mortise views, as well as AP and oblique views of the foot. The mortise view of the ankle may show a shell-like avulsion fracture of the lateral malleolus, indicating disruption of the superior peroneal retinaculum. A fracture of the os peroneum may indicate peroneus longus rupture. Stress radiographs of the ankle (e.g., anterior drawer, talar tilt) can confirm the presence of lateral ligamentous instability.
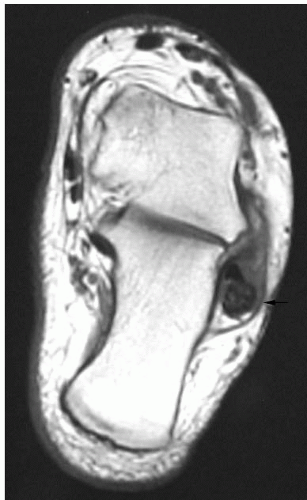
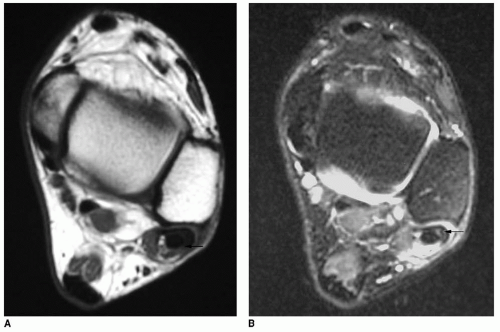
If the diagnosis is uncertain, magnetic resonance imaging (MRI) examination can be helpful (9). It provides information about the specific tendons affected and the extent of injury. MRI allows visualization of disorders such as tendinitis or tenosynovitis, partial tendon tears, and peroneal tendon ruptures (Figs. 25.2 and 25.3). T1-weighted spin echo and T2-weighted fast spin echo images
in axial and coronal cuts are obtained. Some advocate sagittal and oblique axial views. Increased intrasubstance signal intensity in T1- and T2-weighted images is seen in cases of partial tears. Tendon distortion, bisected tendon, tendon enlargement, complete tendon rupture, increased fluid in the tendon sheath, and a convex or flat fibular groove may be observed (10,11). It is common for the peroneus longus tendon to appear normal and the brevis tendon to be enlarged and distorted. It is possible to visualize the superior peroneal retinaculum and the muscle belly of the peroneus brevis with MRI. An anomalous tendon, such as a peroneus quartus, can also be observed with MRI.
in axial and coronal cuts are obtained. Some advocate sagittal and oblique axial views. Increased intrasubstance signal intensity in T1- and T2-weighted images is seen in cases of partial tears. Tendon distortion, bisected tendon, tendon enlargement, complete tendon rupture, increased fluid in the tendon sheath, and a convex or flat fibular groove may be observed (10,11). It is common for the peroneus longus tendon to appear normal and the brevis tendon to be enlarged and distorted. It is possible to visualize the superior peroneal retinaculum and the muscle belly of the peroneus brevis with MRI. An anomalous tendon, such as a peroneus quartus, can also be observed with MRI.
Other studies such as ultrasound, tendon sheath endoscopy, computed tomography, tenography, and kinematic MRI can aid in the diagnosis of peroneal tendon pathology, but they are not as widely used.
SURGICAL TECHNIQUES
Technique 1: Peroneal Tendon Repair and Retinacular Reconstruction
The patient is positioned supine, with a sandbag under the ipsilateral hip or, alternatively, in the lateral decubitus position. Spinal or general anesthesia may be used. A thigh tourniquet is typically used.
A curvilinear, 5- to 7-cm incision is made along the posterolateral fibula in line with the peroneal tendons (Fig. 25.4). Full-thickness flaps are developed, and the superior peroneal retinaculum is identified.
In the cases of tendon dislocation, the outpouching of the retinaculum away from the posterior margin of the lateral malleolus is observed (Fig. 25.5A). The peroneal sheath and superior peroneal retinaculum are incised close to the posterolateral border of the fibula, preserving a cuff of tissue for later repair (Fig. 25.5B and C).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree