PREOPERATIVE CONSIDERATIONS
Certain considerations should be made before triple arthrodesis is performed. These include patient expectations, the desired goal of the fusion and its functional effect, timing of the surgical intervention, biomechanical and positional considerations of the subtalar joint (STJ) and midtarsal joint, the position and alignment of the ankle and leg, bone quality, soft tissue quality, the patient’s age, and the anticipated recovery time.
Candidates for triple arthrodesis usually possess conditions that have proven resistant to conservative therapy, or they have a condition that cannot be expected to respond to conservative measures and one in which the surgeon can expect an adequate result with fusion. The elimination of STJ and midtarsal joint motion may restrict the ability of the patient to adapt to uneven surfaces and terrain; however, in candidates for triple arthrodesis, this motion is often either painful or absent preoperatively. Additionally, the existing deformity often prevents the motion from serving any benefit for the patient, due to either painful arthritis or uncontrollable instability.
Evaluation of ankle joint range of motion is a critical part of the preoperative assessment. This may reveal either an arthritic limitation or a soft tissue equinus contracture, altering the surgical plan. Careful examination needs to be performed in a patient with a severely collapsed pes valgus deformity because significant amounts of dorsiflexion may occur at the midtarsal joint level. In patients with rigid pes valgus conditions, it is difficult to position the foot adequately to assess the true amount of ankle dorsiflexion until the joints have been resected at the time of surgery. In contrast, ankle joint dorsiflexion in patients with a pes cavus deformity may first appear inadequate because of the increase in the osseous height from the maximally supinated position of the midtarsal joint and STJ. Upon restoring a more plantigrade osseous alignment after fusion, one may note a suitable increase in the dorsiflexory motion at the ankle.
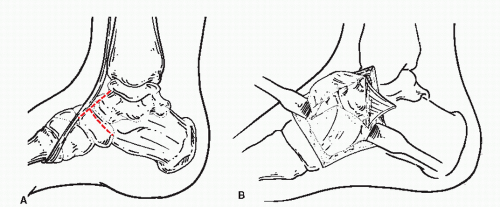
Perhaps the most critical aspect of triple arthrodesis is the ultimate position of the foot after fusion. Poor or inappropriate positioning of the foot may be one of the primary reasons for residual pain and the creation of adjacent arthritis postoperatively. The heel should be aligned to rest in a neutral to slightly everted position. The greatest success in triple arthrodesis has been achieved with the midtarsal joint positioned in slight valgus when fused, that is, with the medial column slightly plantarflexed relative to the lateral column. This position increases the stability of the medial column and first ray, permitting enhanced first metatarsophalangeal joint motion. The valgus positioning may also be more easily accommodated with an orthotic device postoperatively. If the medial column is dorsiflexed relative to the lateral column, the patient is left with a fixed forefoot varus deformity for which no suitable compensation exists.
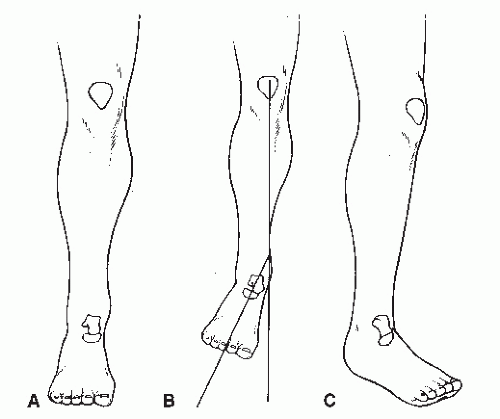
It is important to plan the alignment of the forefoot to the rearfoot and the rearfoot to the leg (
Fig. 58.1). This is especially critical in determining the final position of fusion. The foot normally exhibits 10 to 15 degrees of abduction from the line of progression in gait. In arthrodesis of the rearfoot, the surgeon must know the position of the knee during gait as well as during the surgical procedure. If the knee functions when medially rotated at 15 degrees, then it would be desirable to abduct the foot on the leg 30 degrees, thus resulting in a 15-degree abduction from the line of progression. It is not advisable to abduct a foot if the patient already possesses 15 to 30 degrees of lateral position of the knee in gait. In the latter instance, the foot may be aligned directly with the knee.
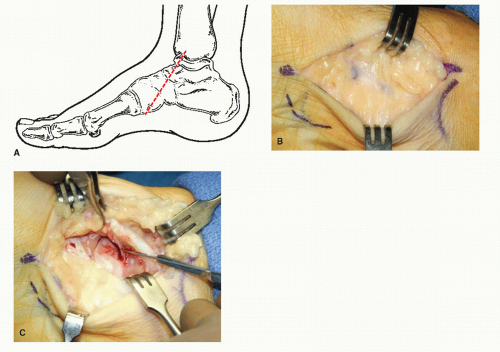
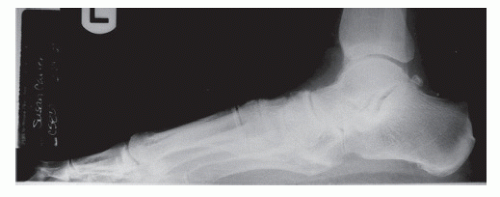
These preoperative assessments are aided by a series of weight-bearing radiographs (
Fig. 58.2) including dorsoplantar, medial oblique, lateral, and calcaneal axial views. Weightbearing films allow a more representative view of osseous alignment. The degree of deformity should be evaluated in each of the cardinal planes prior to proceeding with surgical reconstruction.