4 Trigger point dry needling
safety guidelines
Safety Considerations
Introduction
Box 4.1 Glossary of acronyms
HAI: Healthcare associated infection
NMES: Neuromuscular electrical stimulation
PENS: Percutaneous electrical nerve stimulation
TENS: Transcutaneous electrical nerve stimulation
TRP: Myofascial trigger points
TRPDN: Trigger point dry needling
USCDC: United States Centers for Disease Control and Prevention
WHO: World Health Organization
Dry needling (DN) is an invasive procedure that poses certain risks, in part, not generally associated with other physical therapy or chiropractic treatments. The focal point of this chapter is on safety issues associated with DN. DN can be divided into superficial dry needling (SDN) and trigger point dry needling (TrP-DN). Ultimately, the health and welfare of the patient should be the first consideration (World Health Association 2006), but the welfare of healthcare workers (HCWs) and third parties should not be overlooked. Guidelines and checklists have been employed to improve the quality and safety of complex systems and practices in, for example, aviation, engineering, medicine and surgery (Gawande 2009). A practice guideline is a formal statement about a defined task or function in clinical practice (Barlow-Pugh 2000). DN practice guidelines have been developed in Australia (ASAP 2007), Canada (CPTA 2007) and Ireland (McEvoy et al. 2012). The main focus of this chapter is on patient safety, but HCWs and third party risks are also recognized.
DN is the use of a solid filament needle for the treatment of pain and dysfunction of various body tissues. DN is an invasive technique within the scope of practice of multiple disciplines, such as physical therapy, chiropractic, medicine, dentistry and acupuncture. There are a variety of conceptual models as outlined in other chapters of this book, including TrP-DN and SDN, which are commonly employed to treat pain and dysfunction associated with myofascial TrPs as described by Travell and Simons (Travell & Simons 1983, 1992, Simons et al. 1999). Clinicians may employ one or a combination of conceptual models in clinical practice.
TrP-DN is practiced by physical therapists in many countries including Canada, Chile, Ireland, the Netherlands, South Africa, Spain, Switzerland and the UK (Dommerholt et al. 2006). An increasing number of states in the USA, the American Physical Therapy Association and the American Academy of Orthopaedic Manual Physical Therapists have ruled DN to be under the scope of physical therapy practice (AAOMPT 2009, APTA 2012). Other disciplines also employ TrP-DN, such as chiropractors in the UK and in several US states, massage therapists in Australia and dentists in various countries, among others. With the increase in DN amongst clinicians internationally, it is important to focus on safety, which must be considered the number one priority. In this chapter, DN is approached from a physical therapy perspective, but the safety precautions are of course applicable to all HCWs.
Trigger point dry needling: safety
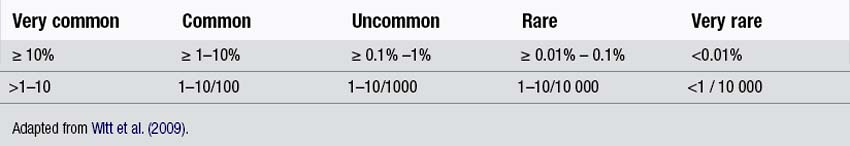
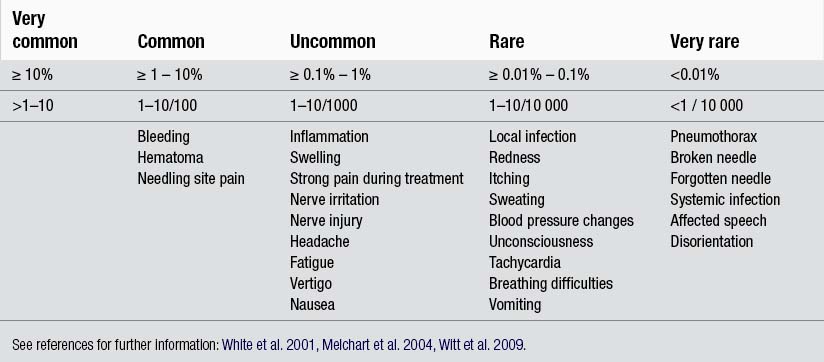
TrP-DN poses potential risks to patients, HCWs and third parties. Many of these risks are not associated with traditional non-invasive physical therapy treatments and may include bruising, pneumothorax, infection, internal tissue damage and bleeding. The term adverse event (AE) is used to describe any ill effect of a treatment, no matter how small, that is unintended and non-therapeutic (White et al. 1997). The severity of AEs can be graded as mild (minor), significant and serious (White et al. 2001, 2008). A mild AE is considered of short duration, reversible and does not particularly inconvenience the patient; a significant AE requires medical attention or interferes with the patient’s activities; a serious AE requires hospital admission with potential persistent or significant disability or death (White et al. 2008). Quantification and qualification grading of AEs has been proposed to objectify risk and this is invaluable for patient education and informed consent. AEs can be categorized into very common, common, uncommon, rare, and very rare with corresponding quantification (Table 4.1; Witt et al. 2009). This grading is helpful when reviewing AE studies.
There are no Medline cited TrP-DN AE studies apart from one individual case study (Lee et al. 2011). Despite the lack of studies, clinician experience would suggest that significant TrP-DN AEs are rare. However, there is a need for TrP-DN AE studies to quantify risk. A prospective TrP-DN AE study amongst physiotherapists has been initiated in Ireland in 2011 (Brady et al. 2011). Though TrP-DN and acupuncture differ in terms of historical, philosophical, indicative, and practical contexts, similarities do exist in terms of solid filament needle skin penetration to varying depths within the body. In this context, acupuncture AE studies assist in identifying TrP-DN risks. Notwithstanding the differences between traditional acupuncture and TrP-DN, clinicians practicing TrP-DN should familiarize themselves with acupuncture AE studies to optimise safe practice and also for patient informed consent. Acupuncture is considered one of the safer forms of medical treatment (Vincent 2001, White et al. 2008). Despite this safety statement, AEs do occur. Peuker & Gronemeyer (2001) grouped acupuncture AEs into five categories including delayed or missed diagnosis, deterioration of disorder under treatment, vegetative reactions, infections, and trauma to tissues or organs (Table 4.2).
Table 4.2 Acupuncture adverse events
| Adverse event category | Example |
|---|---|
| Delayed or missed diagnosis | Cancer |
| Deterioration of disorder under treatment | Increased pain |
| Vegetative reactions | Autonomic type reaction, nausea etc. |
| Bacterial and viral infections | Hepatitis B |
| Trauma of tissue and organs | Pneumothorax, nerve lesion |
Categories adapted from Peuker & Gronemeyer (2001).
A significant number of acupuncture safety and AE studies have been published. Three studies are of particular interest to TrP-DN as they were carried out on physiotherapists and medical doctors and may best reflect clinicians with Western medical training. A summary of the main AEs is presented in Table 4.3.
White et al. (2001) reported AEs related to acupuncture in a prospective clinician survey of 32000 treatments of 78 British physiotherapists and medical doctors. Common minor AEs included bleeding and needling pain, while uncommon minor AEs included aggravation of symptoms, faintness, drowsiness, a stuck or bent needle and headache. Significant AEs were rare or very rare (n=43) and included administrative problems (forgotten needle, forgotten patient), issues at the application site (cellulitis, needle allergy, needle site pain), cardiovascular problem (fainting), gastrointestinal problem (nausea, vomiting), neurological and psychiatric problem (anxiety, panic, euphoria, hyperesthesia, headache, slurred speech), exacerbation of symptoms (back pain, fibromyalgia, shoulder pain, vomiting, migraine). No serious AE was reported in 32 000 treatments surveyed. It was concluded that acupuncture in skilled hands is one of the safer forms of medical intervention (White et al. 2001).
Witt et al. (2009) reported AEs related to acupuncture in a prospective 229230 patient based survey consisting of 2.2 million treatments delivered by German physician acupuncturists. AEs were reported per patient (n=229230) and not per treatment (n=2.2 million) and this should be taken into account when comparing with White et al. (2001), who reported AE per treatment (N=32000). A noteworthy 8.6% of patients reported at least one AE, where 2.2% of patients required medical treatment (significant or serious AE). Common side-effects included bleeding and hematoma (n=14083; 6.1%) and pain (n=4681; 2%). Uncommon side-effects included strong pain during needling (n=490; 0.2%), vegetative symptoms (n=1663; 0.7%), nerve irritation and injury (n=601; 0.26%). Rare and very rare side-effects included local infection (n=31; 0.014%), systemic infection (n=5; 0.002%) and pneumothorax (n=2; 0.001%). As this is arguably the most comprehensive AE acupuncture study, clinicians should familiarize themselves with this study and the expansive quantification of side-effects.
Melchart et al. (2004) reported AE after acupuncture in a prospective clinician-based survey of 97733 patients (760000 treatments) delivered by German physician acupuncturists. Again, similar to Witt et al. (2009), the incidence of AE was reported per patient and not per treatment. Non-serious AEs were seen in 7.10% of patients included needling pain, hematoma and bleeding in 3.28%, 3.19% and 1.3%, respectively. Serious AE were reported in six of 97733 patients including exacerbation of depression, acute hypertensive crisis, vasovagal reaction, asthma attack with hypertension, angina, and pneumothorax in two cases.
Despite the generally good safety of acupuncture, a review of acupuncture systematic reviews from 2000 onwards identified 95 cases of severe AEs including five fatalities (Ernst et al. 2011, Choi 2011). Peuker & Groneeyer (2001) reported on rare but serious complications of acupuncture due to traumatic lesions in a review of the literature from 1965 onwards. According to the authors, all traumatic lesions described could be avoided if clinicians had better anatomical knowledge or applied existing knowledge.
Hygiene
DN is an invasive procedure that poses infection risks to patients, clinicians and third parties which are not normally associated with manual treatments. In 2002, US healthcare-associated infections (HAI) amounted to 1.7 million recorded incidents with 98987 deaths (Klevens et al. 2007). As many as one in 10 patients acquire a HAI (HSE 2009). Infectious agents include bacteria (e.g. Staphylococcus, E. coli), viruses (e.g. hepatitis B and C, human immunodeficiency virus), fungi (e.g. tinea pedis, Candida albicans), protozoa (e.g. toxoplasmosis) and prions (e.g. Creutzfeldt–Jakob disease). The chain of infection is a six element way of describing infectious disease transmission (HSE 2009) and consists of an infectious agent, a reservoir (infectious agent area), a portal of exit (from infected person), a means of transmission, a portal of entry (to target person), and a susceptible host.
Standard Precautions are clinical guidelines to prevent transmission of infectious agents and are published by the United States Centers for Disease Control and Prevention (USCDC) (Siegel et al. 2007, HSE 2009). The purpose of Standard Precautions is to break the chain of infection by focusing particularly, but not exclusively, on the mode of transmission, portal of entry and susceptible hosts (HSE 2009). Standard precautions require HCWs to assume that every person is potentially infected or colonized with an organism that could be transmitted in the healthcare setting and apply a set of work practices to minimize the risk of contamination (HSE 2009). Work practices relevant to DN include attention to hand hygiene, glove usage, skin preparation, management of needles and medical waste, and needle stick injuries (NSI) (Dommerholt 2011).
Hand hygiene
Hand hygiene is considered the single most important intervention to prevent transmission of infection (SARI 2005). Hand hygiene activity recommendations have been evidenced-categorized (I, II, III):
• Category I: supported by experimental, clinical or epidemiological studies based on strong theoretical basis
• Category II: supported by suggestive clinical or epidemiological studies or a theoretical-based rationale
• Category III: recommended by healthcare experts from experience.
1. When the hands are visibly soiled with dirt, soil or organic material (I), they should be washed thoroughly to remove the contaminant.
2. Before and after each patient contact (II).
3. At the beginning and end of each work shift (III).
5. After moving from a contaminated area (II).
6. After handling soiled equipment, materials or environment (II).
7. After personal bodily functions (e.g. blowing nose, after using the toilet) (I).
Hand hygiene and decontamination should be a quality standard in all health care institutions (SARI 2005) and is a learned skill. It may appear rudimentary, but attention to hand decontamination technique is important and often is practiced poorly by HCWs. Handwashing with regular soap can remove dirt, but is generally ineffective in preventing antimicrobial activity, whereas alcohol-based hand rub is generally effective (Ehrenkranz & Alfonso 1991). Antimicrobial soap is somewhat more efficient than non-antimicrobial soap and produces a statistically significant reduction in microbial activity compared to non-antimicrobial soap (Montville & Schaffner 2011). However, the use of alcohol in either soap or gel is more effective than antimicrobial or bland soap without alcohol (Paulson et al. 1999). Recommendations for best practice have been made.
Handwashing with soap (Boyce & Pittet 2002, SARI 2005, HSE 2009)
2. Apply an amount of suitable soap to the hands as recommended by the product manufacturer.
3. Rub hands vigorously for at least 15 seconds encompassing all surfaces of the hands and fingers.
5. Dry hands with a good quality single-use disposable paper towel.
6. Use towel to turn off faucet and dispose of in pedal bin.
7. Avoid using hot water as this may increase skin dryness and dermatitis.
Multiple-use cloth towel, either roll type or hanging style are not appropriate for the healthcare setting (Boyce & Pittet 2002).
Hand decontamination with alcohol-based hand rub (Boyce & Pittet 2002, SARI 2005)
Hands can be decontaminated with suitable alcohol-based hand rub or gel once the hands are visibly clean. Alcohol-based hand rub can be inactivated by organic material and therefore if hands are visibly soiled, they should be washed per the above recommendations. Alcohol-based hand sanitizer is usually recommended at a 70% concentration by weight of isopropanol, ethanol, or n-Propanol. Higher concentrations may increase the risk of skin dryness and dermatitis. The USCDC recommends handwashing with soap after every 5–10 applications of alcohol-based hand gel due to build-up of emollients on the hands (Boyce & Pittet 2002). Manufacturer’s instructions of such products should be noted.
1. Apply product to palm of one hand and rub hands together.
2. Covering all surfaces of hands and fingers.
As HCWs wash and decontaminate their hands up to 30 times per shift (Boyce & Pitte 2002), there is a significant risk of skin irritation and dermatitis. Irritant dermatitis is a non-immunological inflammatory skin response to an external agent and may leave the skin more prone to harbor micro-organisms (SAR 2005). Prevention and management of all forms of dermatitis is important for the safety of patients and HCWs. The USCDC recommends the addition of 1–3% glycerol to alcohol-based hand gel as this can reduce or eliminate as the drying effect of the alcohol (Boyce & Pittet 2002). Advice for the prevention of occupational dermatitis in the healthcare setting includes (SAR 2005):
1. Follow manufacturer’s recommendations on use of hand hygiene product.
2. Use products with low irritation potential and when able with emollient.
3. Receive feedback from HCWs on products used.
4. Use alcohol-based hand rubs with emollients.
5. Promote the use of suitable hands lotions to assist in skin hydration and replace skin lipids.
Gloves
Gloves should be single use, disposable and conform to international community standards. Latex-free gloves should be available for clinicians and used with patients with known latex allergies. Latex-free surgical glove are being used more frequently due to latex hypersensitivity in HCWs and patients, however some may not offer the same protection as latex gloves (Boyce & Pittet 2002, Aldlyami et al. 2010). The Food and Drug Administration has approved several powered and powered-free latex gloves with reduced protein contents and synthetic gloves for latex-sensitive HCWs (Boyce & Pittet 2002). Nitrile gloves are usually preferable in those with latex allergy concerns. Gloves should be donned immediately before and removed immediately after the DN procedure is completed and if contaminated with blood or body fluids, should be disposed of in appropriate healthcare waste. Wearing gloves provides an ideal environment for bacterial growth and hands should be washed after removal of gloves.
Patient skin preparation
Patient skin disinfection is not usually required prior to DN if the skin is visibly clean, which is in line with the World Health Organization’s (WHO) best practice for intradermal, subcutaneous and intramuscular needle injections (Hoffman 2001, Hutin et al. 2003, Baldry 2005, BAC 2006, ASAP 2007, White et al. 2008). Resident skin bacteria are unlikely to lead to infection if host immunity is not compromised (Hoffman 2001). Many countries do not have formal regulations regarding skin disinfection for needling procedures (Dommerholt 2011). The National Acupuncture Foundation recommends disinfecting the skin with 70% isopropyl alcohol prior to needling (Given 2009). The British Acupuncture Council Code of Safe Practice recommends to use 70% isopropyl alcohol or products which contain 0.5% chlorhexidine before needling in ‘areas of the body where moisture or exudates may collect, such as the groin and genital area, ears, feet, under arms and the area below the breasts, near the mouth, nose, scalp and other hair covered areas’. In contrast, Dutch guidelines (WIP 2008, Dommerholt 2011) in line with WHO, do not recommend to disinfect the skin, with the exception when using semi-permanent needles or performing ear acupuncture. If the skin is visibly soiled it should be washed with warm water and soap and dried accordingly prior to DN. Clinicians should not needle into joints or bursae. During DN the clinicians should only touch the needle at the handle and should avoid touching the needle shaft. If this occurs the needle should be removed, disposed of and replaced with a fresh sterile needle. Similar practice should be applied if the needle lies onto the patient’s skin. Multi-pack needles are not recommended for DN as their use increases the likelihood of touching the needle shaft.
Immunocompromised patients may not be suitable for DN and special consideration is required. If DN is considered suitable, skin preparation with a sterilizing solution such as 2% iodine in 70% alcohol should be used and left on the skin to dry for a minimum time of 2 minutes (ASAP 2007).
Needle and medical waste disposal
Needle and medical waste disposal should be done in accordance with local jurisdictional policies and procedures. Clinicians should be knowledgeable with local laws and regulations as standards differ internationally. In the US, regulated medical waste is material derived from animal or human sources or from biomedical research as described by UN-3291 (USDA 2009). All sharps and blood or bodily fluid soiled waste from DN needs to be disposed of in suitable waste disposal per local jurisdictional policies. Used needles are disposed of in a regulated ‘sharps container’ meeting regulatory standards such as UN-3291. Medical waste, such as soiled gloves or blood swabs (but no sharps objects), is placed in a suitable clinical waste bag. Both sharps containers and clinical waste bag should be disposed in accordance with local laws and procedures, which may entail the use of a licensed medical waste company.
Needle stick injury
NSI is a common occupational injury amongst HCWs. In the UK, 37% of nurses reported a prevalence of NSI (Yang & Mullan 2011). In Ireland, medical interns reported a 26% incidence of NSI in the first 8 months of work with only 26% commonly using gloves in phlebotomy-like tasks (O’Sullivan et al. 2011). US based medical students reported a 59% NSI rate during their training (Sharma et al. 2009). It has been estimated that over 20 bloodborne pathogens can be transmitted from contaminated needles including hepatitis B (HBV), hepatitis C (HCV) and human immunodeficiency virus (HIV) (Yang & Mullan 2011) and therefore NSI creates a serious risk for HCWs. Surprisingly, NSI’s commonly go unreported. In one study only 17.5% of incidences were reported (Hettiaratchy et al. 1998). The associated risk of infection transmission of HIV following a hollow needle NSI is about 0.3%, compared with 3% for HCV and 30% for HBV (Parsons 2000). Exposure risk increases with a larger quantity of blood, for example when the needle is visibly contaminated with the patient’s blood (Rodts & Benson 1992). Furthermore, hepatitis B virus can survive for 1 week in dried blood, which underpins the importance of good hygiene techniques and needle and waste disposal (Bond et al. 1981). Other factors that increase NSI infection transmission include piercing deeply or directly into an artery or vein with the contaminated needle (CDC 1995). The risk of NSI infection with a solid filament needle would be expected to be less than a hollow needle; however, NSI risk should be taken seriously. If a NSI occurs, the USCDC recommends immediately washing the punctured area with soap and water, reporting the incident to the appropriate line manager, and seeking medical assessment as soon as possible (CDC 2011). HCWs should have hepatitis A and B vaccinations as required.
Contraindications and precautions
It is important to recognize contraindications, relative contraindications and special precautions for safe DN practice (WHO 1999, Batavia 2006, ASAP 2007, White et al. 2008). Patients should be routinely screened for current or historical presence of contraindications or precautions. Special attention should be paid to medical diagnoses and comorbidities (e.g. a patient with low immune function and history of diabetes). Further, when a contraindication is present, it is important that the clinician is not persuaded to needle by an enthusiastic patient (White et al. 2008).
Absolute contraindications
DN therapy is contraindicated and should be avoided in patients under the following circumstances (ASAP, 2007; White et al., 2008):
1. In a patient with needle phobia.
2. Patient unwilling – fear, patient belief.
3. Unable to give consent – communication, cognitive, age-related factors.
4. Medical emergency or acute medical condition.
5. Over an area or limb with lymphedema as this may increase the risk of infection/cellulitis and the difficulty of fighting the infection, if one should occur (Filshie 2001, Goodman et al. 2003).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree