Triangular Fibrocartilage Complex Tears: Arthroscopic Management Options
Kevin D. Plancher
Sheryl L. Lipnick
CLINICAL EVALUATION
Pertinent History
The functions of the distal radial ulnar joint (DRUJ) as well as its major structure, the triangular fibrocartilage complex (TFCC), have been reported extensively. The TFCC acts as a cushion between the distal end of the ulna and the radial ulnocarpal joint. It is a ligamentous connection between the distal radius and the ulnar side of the carpus. Loss of TFCC support may result in subluxation or dislocation of the DRUJ. Complete excision of the TFCC, a previously recommended treatment for the painful DRUJ, has been shown to lead to an increase in ulnar lunate abutment and erosion of the cartilage, causing increasing wrist pain.
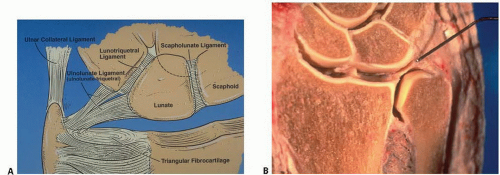
The TFCC consists of various parts including the triangular fibrocartilage, the articular disk, the dorsal and palmar ligamentous attachments, the meniscus homologue, and the extensor carpi ulnaris (ECU) subsheath (Fig. 42.1A, B).
TFCC injuries are a common cause of ulnar-sided wrist pain, especially in athletes. There are multiple pathologies that can result in ulnar-sided wrist pain. The differential diagnosis includes ligamentous/tendinous, osseous, vascular, neurologic, and other etiologies. Ligamentous/tendinous injuries include TFCC tears, intrinsic or extrinsic ligamentous damage, tendinitis of the flexor carpi ulnaris or ECU tendons, and ECU tendon subluxation. Osseous sources such as fracture, nonunion, malunion, and arthritis can also cause ulnar-sided wrist pain. Ulnar artery thrombosis, hemangiomas, ulnar nerve entrapment, neuritis and complex regional pain syndrome represent vascular and neurologic sources of pain. Tumors and avascular necrosis of the lunate (Kienbock’s disease) are additional causes of ulnar-sided wrist pain.
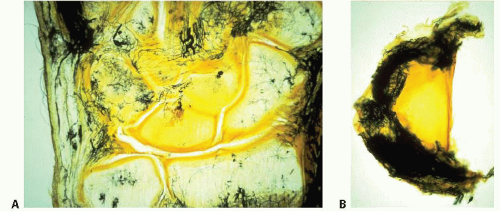
The majority of the blood supply to the TFCC has been shown to be along the peripheral edge of the TFCC (Fig. 42.2). The primary vascular supply comes from the anterior interosseous artery and the ulnar artery. The dorsal branch of the interosseous artery supplies most of the dorsal periphery, and the palmar branch supplies the volar periphery near the radial attachment. The ulnar artery supplies the styloid region and ulnar portion of the volar periphery. Vascular penetration extends to only the peripheral 15%, leaving the central portion of the disk relatively avascular. There has also been a concern over the healing potential of radial-sided TFCC lesions. However, Cooney et al., Plancher et al., and others have showed adequate healing of radial-sided TFCC repairs. The neural supply, similar to the vascular supply, excludes the central portion of the disk. The ulnar nerve supplies the volar and ulnar portions of the TFCC, while the posterior interosseous nerve supplies the dorsal portion. There is a variable contribution of the dorsal sensory branch to all portions of the TFCC.
One main function of the TFCC is load transmission, which is dependent upon forearm rotation. The TFCC has been shown in biomechanical studies to distribute up to 20% of the load across the ulnar wrist. The ulna assumes a relatively shortened position in supination and a relatively lengthened position in pronation. The primary stabilizers of the DRUJ are the dorsal and volar radial ulnar ligaments. The TFCC has a number of primary functions. It extends over the articular surface of the distal radius to cover the ulnar head. It partially absorbs the load while it transmits an axial force across the ulnocarpal joint. The TFCC provides a strong but flexible connection between the distal ulna and the radius, allowing for forearm rotation. Lastly, the TFCC supports the ulnar portion of the carpus through the connections established to both the ulna and the radius.
The history of a patient with a TFCC tear may include ulnar-sided wrist pain with pronation or supination, especially with weight-bearing. The patient may also report a sense of clicking or popping with forearm rotation, such as turning a doorknob or swinging a racquet or golf club. Activity usually exacerbates the symptoms, where rest can relieve them. Traumatic TFCC injuries are usually the result of a fall on an outstretched hand, where there is an extension-pronation force on an axially loaded wrist. Other mechanisms include either a dorsal rotation injury or a distraction force applied to the volar forearm or wrist. In addition, patients with distal radius fractures have been found to have tears of the TFCC.
Physical Examination
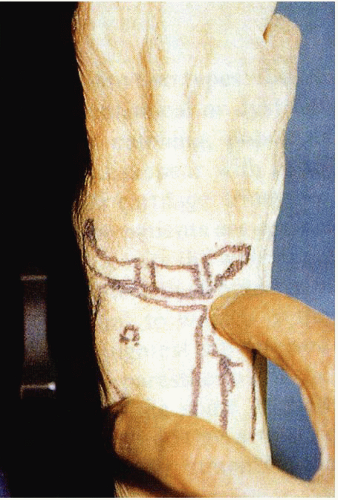
The physical examination of a patient with a suspected TFCC tear begins with adequate inspection of both the affected and the unaffected sides. The wrist, forearm, and DRUJ should be assessed for swelling. The extremity should be palpated for tenderness, specifically over the TFCC in the soft spot between the flexor carpi ulnaris, the ulnar styloid, and the triquetrum (Fig. 42.3). Range of motion of the wrist and DRUJ, both active and passive, should be evaluated and compared with the opposite extremity. The examiner should be aware of other wrist pathologies that may mimic TFCC tears, such as DRUJ arthritis, ECU tendinitis/subluxation, and lunotriquetral ligament tears. Supination and ulnar deviation should exacerbate subluxation of the ECU. The shear or ballottement test can aid in the evaluation of lunotriquetral ligament tears.
DRUJ instability is assessed with passive manipulation of the ulna and radius. Increased translation in the anteroposterior plane is evident and should be evaluated in a neutral, supinated, and pronated forearm position. The ulnocarpal stress test may reproduce the symptoms caused by disk tears or ulnocarpal degeneration. The forearm is placed in a vertical position on the examiner’s table. An axial load is then placed through the wrist while the wrist is moved through radial and ulnar deviation with simultaneous pronation and supination. The press test is another way to dynamically load the ulnocarpal joint. The patient grasps the arms of a chair and pushes up to a standing position. The press test, although not particularly specific, is positive if symptomatic ulnar wrist pain is elicited with this maneuver.
Imaging
Radiographs, including a zero-rotation posteroanterior (PA) and lateral views of the wrist, should be obtained. Ulnar variance measurements can be obtained on the PA view, which is taken with the shoulder abducted to 90° and the elbow flexed to 90° with the hand flat on an X-ray cassette. DRUJ instability can be accentuated through a lateral stress view in which the patient holds a 5-lb (2.26 kg) weight with the forearm pronated and the X-beam directed “cross-table.”
Arthrography, while once having a key role in assessing for TFCC tears, has slowly fallen out of favor due to poor clinical correlation and increased use of MRI and arthroscopy. Not only has a high incidence of perforations been detected in asymptomatic wrists of various ages but studies have also shown low sensitivity of arthrography compared with arthroscopy. Nonetheless, a negative arthrogram can be a useful screening tool. After arthrogram,
if dye is present within the substance of the TFCC, a partial thickness tear is suspected. A full thickness tear should be suspected if the dye passes from the wrist joint into the radioulnar joint.
if dye is present within the substance of the TFCC, a partial thickness tear is suspected. A full thickness tear should be suspected if the dye passes from the wrist joint into the radioulnar joint.
CT can evaluate for fractures, degenerative arthritis, and possibly DRUJ instability. To adequately assess for DRUJ instability, both forearms need to be evaluated in identical forearm positions. MRI, which is noninvasive, is commonly used to assess injuries of the TFCC. The sensitivity, specificity, and accuracy, however, vary widely. MRI can also be used to evaluate for bony edema, the thickness of the articular cartilage, the subchondral bone of the distal ulna and carpal bones, and the integrity of the lunotriquetral ligament.
Arthroscopy can be used as a diagnostic and therapeutic modality and is considered to be the gold standard for diagnosing injuries of the TFCC. A number of other wrist injuries or carpal pathologies can also be treated with arthroscopy. A lax or hypermobile TFCC can be determined with direct probing. This “trampoline” effect is indicative of an unstable TFCC (Fig. 42.4). Evidence of TFCC injury may also include scarring or vascular invasion seen along the periphery and tears of the lunotriquetral interosseous ligament or ECU sheath.
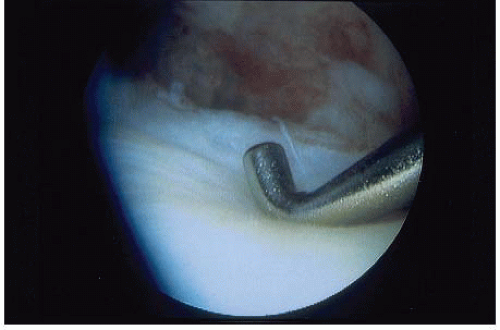 FIGURE 42.4. The “trampoline” effect is shown by directly probing a lax or hypermobile TFCC. The increased laxity represents a tear of the TFCC. (© Kevin D. Plancher.)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|