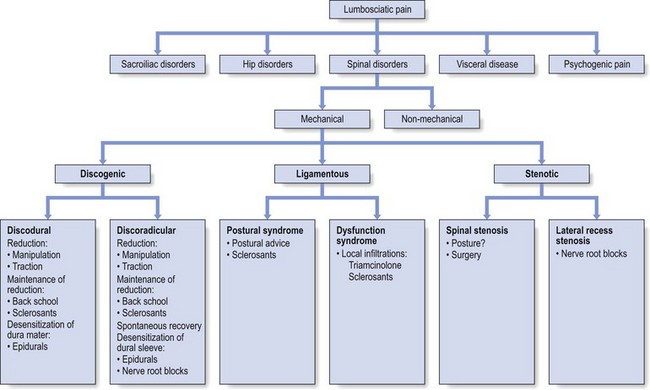
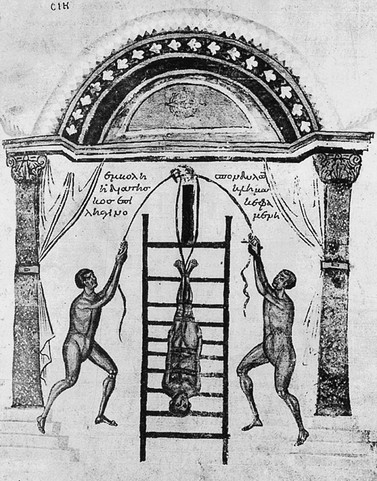
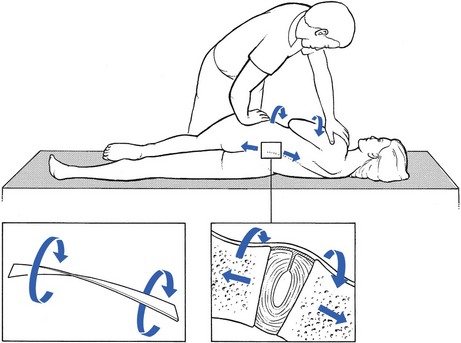
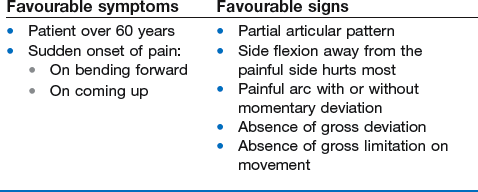
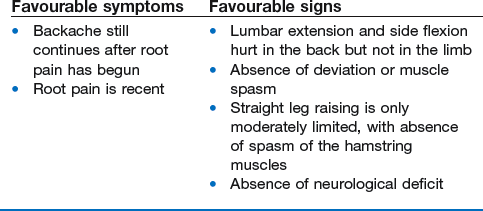
40 A wide variety of non-surgical treatments are advocated in the management of low back pain. Back school instructions, bed rest, cryotherapy, medication, exercises, manipulation, traction, mobilization, local blocks, epidural infiltrations and spinal orthosis all claim to have their successes but until now, controlled studies of large, unselected populations have not demonstrated the superiority of any one of these measures,1–7 which thus supports the view that there seems to be no definite evidence that any treatment for low back pain is much better than the placebo effect.8,9 Some authors even suggest that the main effects of the therapies are produced not through the reversal of physical weaknesses targeted by the corresponding exercise method but rather through some ‘central’ effect, perhaps involving an adjustment of perception in relation to pain and disability.10 Obviously, these studies have reinforced therapeutic nihilism. As conservative measures are not proven to be effective, the patient is told to learn to live with the disability until it disappears spontaneously.11 However, in analysing the results, one striking factor emerges – the lack of a proper diagnosis. In current clinical trials on the effectiveness of treatment for lumbar disorders, the course of one symptom only (pain) is evaluated in randomized groups of patients. This is completely wrong. Controversies over treatment are usually the result of studies performed on widely differing lesions. A group of patients complaining of ‘backache’ is very heterogeneous. Even if, in most cases, the disc is responsible for the pain, the mechanism will differ considerably from patient to patient. Before any kind of randomization is done, the individual disorders in any group of patients should be clearly identified; treatment could then be given not for a symptom but for a well-defined condition.12 We therefore believe that, before treatment of any kind is instituted, a clear diagnosis must be made and the physician must have a distinct idea of the underlying cause. Treatment can then be prescribed selectively, according to the type and the severity of the lesion. For example, a recent systematic review of randomized clinical trials on spinal manipulation could find no evidence of effectiveness, except in some subgroups of patients, using clearly delineated clinical inclusion criteria.13 The history and clinical examination almost always indicate the best method of treatment for an individual patient. It is our personal experience that, if conservative treatment techniques are employed intelligently, there is definite evidence that in each case one treatment is better than another or than the placebo effect. Also, only a few patients will remain wholly unrelieved, in which case surgery may be required. Even when surgery is indicated, the decision must be made on clinical grounds alone. An abnormality seen on imaging and not confirmed by clinical examination is not an indication for surgery.14 It is important to exclude psychogenic pain and pain of visceral origin referred to the back. • Reduction of the displacement: achieved by manipulation or traction. • Maintenance of reduction: obtained by sclerosing injections and/or back school instructions. • Desensitization of the dura mater: acute or gross inflammation requires desensitization of the dura mater before manipulation or traction is attempted. Alternatively, if the dura mater remains inflamed after discodural contact has ceased, the treatment is epidural local anaesthesia. • Desensitization of the dural nerve root sleeve: in intense discoradicular contact leading to some degree of parenchymatous involvement, attempts at reduction fail. De-inflammation and desensitization of the dural sleeve, while spontaneous recovery is awaited, is then a good and defensible therapeutic approach. Epidural local anaesthesia via the sacral canal is the technique of choice. Should this fail, a sinuvertebral and nerve root block can be substituted. Desensitization of the dural sleeve is also recommended when the discoradicular contact has lasted for some time or when the nerve root remains inflamed after the conflict has ceased (Fig. 40.1). The following questions must be addressed when devising a treatment plan: • What attitude does the patient have towards the problem? • Is there a desire to get better? • Is there any compensation claim? • Is there evidence of psychoneurosis? • Will active and sometimes unpleasant forms of treatment be tolerated? These questions must be addressed when devising a treatment plan. If treatment is employed along these lines, only a few patients will remain unrelieved. This approach has also proved to be safe and, at the same time, is a meaningful, realistic and practical response to the enormous liability of lumbar disorders in terms of cost and needless human suffering. In 1986, the annual cost of back pain in the USA approached $81 billion.15 By 1995, the total cost to society of low back pain was more than $100 billion16 and the economic loss 101.8 million workdays.17 In the UK, the direct healthcare cost of back pain in 1998 was estimated to be £1632 million. However, this figure is insignificant compared to the cost of the production losses related to it, which was £10 668 million, making back pain one of the most costly conditions for which an economic analysis has been carried out.18 A substantial portion of low back care costs reflects expensive surgical therapy, when many patients could have been effectively treated if the above-mentioned less costly regimens had been tried first. Unfortunately, the average spinal surgeon is usually neither trained in nor knowledgeable about conservative spinal therapy. In fact, in some of the present state healthcare systems, surgery is routinely performed in almost all cases of low back pain (Burton14: p. 105). This has been confirmed by Finneson,19 who studied one series of 94 patients in whom back surgery had failed and found that in 81% the original surgery was not indicated. Manipulation and traction are no exceptions to the rule that all medicine can be traced back to Hippocrates (400 bc). His methods of treating back disorders were practised in the subsequent centuries by other famous physicians: for example, Apollonius, Galen, Avicenna, Ambroise Paré, Percival Pott, Sir James Paget and many others. In China, the technique of manipulation was fully established during the Tang Dynasty (ad 618–907). Illustrations show that the ancient methods of manipulation and apparatus traction did not differ very much from the methods of treatment practised nowadays in low back pain and sciatica (Fig. 40.2). Manipulation and traction are methods of reducing pain and disability caused by internal derangement of intervertebral cartilaginous structures. This treatment undoubtedly stems from man’s experience with those examples of lumbago, low back pain and sciatica that were relieved by a sudden twist or a fall. Schiötz and Cyriax20 described several examples in which patients reported such a sudden relief of symptoms after an unintentional movement. One of our colleagues reported a patient who recovered from backache on falling down her basement cellar steps. Undoubtedly, such experiences have given rise to various, sometimes bizarre mechanical treatments in folk medicine, such as trampling on a patient’s back, wrestling the back, striking the back with the weight of a steel bar or standing back to back ‘weighing salt’ (two persons stand back to back, hooking their arms at the elbow; each person bends forwards in turn, lifting the other from the floor). These measures seem non-specific and possibly harmful but Schiötz commented: ‘It seems justified to infer that methods found effective by the natives of parts of the world as far apart as Norway, Mexico and the Pacific Islands over many, many centuries must be valid.’ These primitive methods are also the models for more modern techniques of manipulation and traction taught and practised by trained doctors and therapists all over the world. Although different methods and different theoretical concepts developed, this seemed not to matter much as all claimed their successes. Cyriax21 was convinced that, in nearly all cases, a similar mechanism is at work – a dislocated fragment of disc returns to position or a protrusion is ‘sucked back’. He also stated: ‘Spinal manipulative methods of orthopaedic medicine are perfectly straightforward and possess an explicable intention directed to a factual lesion. They are based on the discovery of disc lesions as the primary cause of degenerative change and pain of spinal origin.’ It is hard to believe that, even nowadays, many doctors still refuse to recommend manipulation of the back as the treatment of choice in nearly all cases of acute low back pain and sciatica. Avoiding discussion of the topic of spinal manipulation is also unwise, since a significant number of their patients will have received or will be considering this form of treatment: in the USA in 1980, 120 million surgery visits were made to chiropractors.22 An increasing number of controlled clinical trials on well-delineated subgroups have been published, which compare the results of manipulation to different forms of placebo therapy as well as to other forms of conservative management.23–34 The positive effects of manipulation appear to occur either immediately after the manipulation session or within the first 4–6 weeks of treatment.35–37 In orthopaedic medicine, spinal manipulation is defined as a method of conservative treatment by passive movements, carried out with a single thrust or sustained pressure, in order to return a displacement to its proper position (see Ch. 5, p. 95). During the thrust, an audible click is often produced. This may accompany immediate relief of symptoms and signs, which supports the precision of the diagnosis and selected therapy. There are different schools of thought in manipulation, which derive from different attitudes towards spinal disorders. The theories on which manipulation is based include the reduction of disc protrusions,38,39 the correction of posterior joint dysfunction,40 the mobilization of blocked vertebral joints,41–44 the reduction of nerve root compression,45,46 the normalization of reflex activity47–50 and the relaxation of muscles.51 • The lumbar spine is positioned in such a way that the affected intervertebral joint opens, i.e. gives the loose fragment room to move. • The manipulation is usually carried out during traction. This tautens the posterior longitudinal ligament and causes suction in the disc, so exerting a centripetal force (Fig. 40.3). Most other manipulative schools claim to work more selectively, i.e. on the affected level only. They claim to have developed the clinical skills to localize, by palpation, the exact site of the ‘fixation’ or ‘locking’. Several studies have failed, however, to demonstrate the reliability of this approach.52–57 We support McKenzie’s58 conclusion that demystification of spinal manipulative therapy is an urgent priority. Both chiropractice and osteopathy thrive by creating the impression that there is something complex and exclusive about the practice of passive end-range motion that only chiropractors or osteopaths can understand or have the skills to ‘feel’. They generate the belief that, in order to become skilled in the understanding and delivery of spinal manipulative therapy, it is necessary to undergo 3 or 4 years of training.59 This suggestion is undermined by the fact that the majority of lay manipulators in Britain have never had any tuition at all and yet have amassed many satisfied clients and also very rarely figure in actions for damages.20 • The displacement should be cartilaginous, not too large and not placed too far laterally. Soft nuclear protrusions are seldom reduced by manipulation unless they are small and very recent, and the technique of manipulation is changed to sustained pressure. If the consistency of the displacement is not quite clear, with symptoms and signs pointing in opposite directions, it is worthwhile making one attempt at manipulation. During the first session, it is usually quickly apparent whether reduction by this means will prove feasible or not. If it fails, traction is substituted the next day. Reduction of cartilage displacements, together with full relief of symptoms and signs, has proved to be possible in two-thirds of all cases of backache and in one-third of all cases of sciatica.60 Just about half of all lumbago cases are relieved in one treatment.61,62 • The patient must be mentally stable and keen to get well. If this psychogenic aspect is neglected, on some occasions a patient may be treated who claims to have been made worse by a type of therapy that is regarded in retrospect as unacceptable. Hence it is important to avoid these active methods of treatment when the patient’s attitude appears to be more important than the minor mechanical disorder found on examination. History and clinical examination almost always supply sufficient information to select those cases suited to manipulation (see Box 40.3, below). Reduction should always be attempted, except in hyperacute cases where the attempt proves impossible to bear. An epidural injection is then substituted and followed by manipulation the next day. If such an injection is refused, it is still possible for the patient to recover in about a fortnight with bed rest and the use of McKenzie’s extension mobilizations58 and anti-deviation techniques. The moment the process has ceased to be hyperacute, treatment by manipulation can be tried again. • A partial articular pattern in which some movements are only painful at extreme range: for example, flexion, extension and side flexion away from the painful side • The existence of a painful arc with or without momentary deviation • Absence of gross deviation caused by muscle spasm on standing or during as much flexion as the patient can tolerate • Absence of gross limitation on movement – gross deviation or limitation of movement always requires several sessions of manipulation (Box 40.1). These may be divided into circumstances in which manipulation is absolutely contraindicated and those in which manipulation is of no use, although not harmful to the patient (Box 40.3). Appropriate selection of patients and choice of techniques can avoid such serious complications as have been reported.63,64 Acute lumbago and bilateral sciatica with compression of the nerve roots at the same level are examples of a large central protrusion in which bulging of the posterior longitudinal ligament is to be expected. Such a protrusion may also cause spinal claudication. These patients have symptoms during walking, immediately relieved by lying down.67 Manipulation of patients on anticoagulant therapy may lead to an intraspinal haematoma.68 A patient who has a clotting abnormality should also not be subjected to forceful manipulations. Manipulation should not be employed at any time if there is any predisposition to miscarriage. Protrusions causing impaired root conduction All such protrusions are impossible to reduce by either manipulation or traction. If clinical signs of muscle weakness, cutaneous analgesia or reflex disturbances are present, the protrusion is too large (and located too far laterally) to be replaced.38,69–73 Epidural local anaesthesia is the treatment of choice. Acute nuclear lumbago is also an example of a protrusion that is too soft to manipulate with a thrust. The history is of pain that began gradually, after much stooping and lifting, and became slowly worse over the next few hours. The following morning, the patient wakes unable to get out of bed because of severe lumbar pain. The patient is always under 60 years old and, although manipulation is indicated, it must be exerted by sustained pressure. If this makes the patient better, techniques should follow in the supine, side-lying and standing positions to correct a persisting lateral deviated position of the trunk (see pp. 554–556). Alternatively, an epidural injection can be tried, again followed the next day by manœuvres to correct a lateral deformity. However, if these measures all fail, constant pelvic traction, in a supine position and continued for some days, is called for, slowly changed to periodic half an hour daily traction. Extension mobilizations, as recommended by McKenzie,58 have also been found to be effective; this treatment is based on McKenzie’s hypothesis that flow or displacement of fluid, nucleus or sequestrum can occur within the intact annulus of the intervertebral disc as a result of prolonged or repetitive loading. This most commonly occurs with flexion loading. He recommends well-defined extension forces in order to reverse the direction of flow or displacement. Central stenosis, lateral recess stenosis and the ‘self-reducing’ disc protrusion do not respond to manipulative treatment. In stenosis, the underlying condition is the reason that attempted manipulation or traction fails.71,74,75 The self-reducing disc protrusion, with symptoms at the end of the day only, may be reduced by manipulation but will prove to be transient anyway.38 Lumbar manipulation is quite safe.63,64 The most frequently reported serious complication is further prolapse of a herniated disc, resulting in a cauda equina syndrome. However, the risk of spinal manipulation causing a cauda equina syndrome is estimated to be less than 1 per 3.7 million treatments.65,76 Most of the incidents were described in patients undergoing manipulation under anaesthesia or chiropractic adjustments.66 Long-lever, high-force rotation techniques in the side-lying position are regarded as responsible. This is only partly true: the underlying cause is the lack of adequate examination to rule out unsuitable disorders. If, in contrast, manipulative procedures are instituted after a thorough examination, those described in this book have never led to severe accidents. The main advantages of these manipulations are: • A great deal of traction is used to exert a strong centripetal force on the intervertebral joint. • Movements towards flexion, which can intensify potentially harmful centrifugal forces, are excluded. • Each manœuvre is followed by a fresh assessment of dural, root and articular signs, which affords a clear pointer to what has happened inside the joint and what the next step should be.
Treatment of the lumbar spine
Introduction
Is the pain caused by a spinal disorder?
If the spinal disorder is activity-related (mechanical), to which ‘concept’ does it belong?
Is the disorder a discodural or discoradicular interaction?
What sort of person is the patient?
Manipulation
Introduction
Definition of manipulation
Indications for manipulation
Acute annular lumbago
Backache
Contraindications
Absolute contraindications
Danger to the fourth sacral roots65,66
Anticoagulant medication
Final month of pregnancy
Cases in which manipulation is not useful
Too large a protrusion
Too soft a protrusion
Compression phenomena
Dangers of manipulation
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Treatment of the lumbar spine