CHAPTER 62 Treatment of the Infected Total Elbow Arthroplasty
INTRODUCTION
Despite multiple improvements in total elbow arthroplasty design, infection was a relatively common and potentially catastrophic complication, with reported rates as high as 11% in earlier studies.* The rate had decreased considerably, and was 3% in our practice overall.39 Others have reported similar findings, with a slightly higher infection rate of approximately 8% in the revision setting,32 and 5% in patients with rheumatoid arthritis.1,11,30,35 Although not demonstrated with certainty, the rate seems to have increased since the introduction of the disease-remitting agents (DMARDs) to treat rheumatoid arthritis (see Chapter 54).
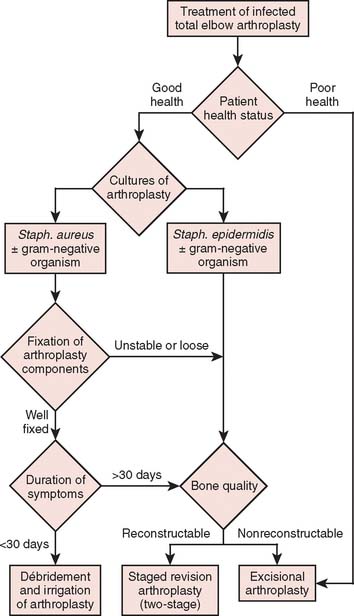
This difficult complication can be treated with either open débridement with placement of antibiotic beads and staged bushing exchange, removal followed by staged reimplantation of components, or resection arthroplasty, depending on the onset and chronicity of symptoms from the time of index arthroplasty. With little information on which to base treatment decisions, poorly functioning and sometimes painful resection arthroplasty has been the definitive procedure of choice, particularly in elderly patients who have relatively low demands on the elbow.14,27,38 Treatment options that have allowed concurrent eradication of the infection with either prosthetic retention or reimplantation have been explored with relatively good results in the past decade, especially at the knee and hip.15,16,21,22,24 Thus, this treatment strategy has been employed in the treatment of the infected total elbow arthroplasty under certain circumstances.6,39,40 Patients who have clinical evidence of infection but have negative cultures represent a treatment dilemma. Most are treated as if they are infected, with resection of the prosthesis, and staged reimplantation after cultures are followed to completion, with a course of parenteral antibiotics. However, this strategy increases the morbidity from a repeat general anesthetic as well as another surgical insult to the elbow. If the implants are well fixed, removal of the prosthesis may pose technically challenging.28,38 The objective of this chapter is to review the evaluation and treatment of the infected total elbow arthroplasty. In particular, patient presentation including health profile, duration of symptoms, fixation of components, and bacteriology are discussed in relation to indications for various treatment strategies for the infected elbow arthroplasty (Fig. 62-1).
ETIOLOGY AND INCIDENCE
Since the initial reports on infections of total elbow arthroplasties, the clinical presentation of these prosthetic infections has changed. Increased awareness of this complication has led to a high index of suspicion and hence earlier recognition.14 However, even at 3%, the rate of infection for elbow arthroplasties remains well above that for the lower extremity arthroplasties, in part because of the high prevalence of severe rheumatoid arthritis or post-traumatic arthritis.11,14,27,38 Risk factors for total elbow infections include rheumatoid arthritis,1,11,35 previous surgical procedures,27 previous local infections38,40 and use of tumor necrosis factor (TNF) antagonists.17 The elbow is a subcutaneous joint with a relatively thin soft tissue envelope, which increases its susceptibility to wound healing complications. In addition, patients with rheumatoid arthritis are often immunocompromised and are taking DMARDs, which may increase the incidence of periprosthetic infection.17 Those with post-traumatic arthritis frequently have undergone multiple operations that compromise the vascularity of the soft tissues and thus increase the risk of wound healing complications.14,38 Delayed wound healing, wound drainage longer than 10 days postoperatively, and reoperation are prognostic factors associated with increased infection rates.38
The incidence of infections following total elbow arthroplasties appears to have declined with improvements in surgical techniques but is now possibly increasing because of the use of the DMARDs. Our experience has shown a decrease in infection rate from an initial report of 8% to a more recent incidence of about 3%.25,27,39 In one long-term series of total elbow arthroplasty, there was no reported infections after the institution of routine use of antibiotic impregnated cement.37 It appears that the use of antibiotic-impregnated cement to implant the components, along with meticulous postoperative hematoma control, has been helpful in lowering the incidence of infections. By protocol at the Mayo Clinic, postoperative elbows are immobilized and elevated in full extension for a period of 24 to 36 hours to allow for edema control and wound epithelialization, before allowing range-of-motion exercises.
PATIENT PROFILE
The most important consideration in treating a patient with an infected total elbow arthroplasty is the overall status of the host. The health status comprises both the patient’s medical condition and his or her functional needs and expectations. Many patients with rheumatoid arthritis are medically debilitated owing to immuno-suppressive medications, anemia of chronic disease, previous surgery, and, sometimes, poor nutrition. Our protocol for these patients includes cessation of DMARDs, which are TNF antagonists (etanercept, infliximab, or adalimumab) at least 2 weeks before surgery and until 2 weeks postoperatively, because these medications have been shown in some studies to increase the incidence of periprosthetic infection.17
The clinical presentation of an infected total elbow arthroplasty may be subtle and only recognized by maintaining a high index of suspicion.38 Patients with an infected olecranon bursa should be assumed to have a deep infection unless proven otherwise. Systemic signs of sepsis (fever and tachycardia) may be absent,27 with the patient complaining of increased pain or pain at rest. Acute inflammation is usually detectable by local signs such as the presence of warmth, erythema, and tenderness. In some patients, there may be drainage from the wound or soft tissues.6,14,27,38 These points become important in determining the onset and thus chronicity of an infection.
Preoperative evaluation is critical to establish range of motion, stability of the elbow, neurologic status, and function of the biceps and triceps muscles. Laboratory data may be of limited value, with most patients having a normal leukocyte count but an elevated neutrophil count on differential analysis.27 The erythrocyte sedimentation rate (ESR) is often elevated but not specific, because many have systemic inflammatory disease. C-reactive protein (CRP) is now routinely collected to aid in the sensitivity of detecting occult infection.6 The definite step is to aspirate the joint (Fig. 62-2). Patients are considered infected when there are positive cultures or strong clinical suspicion (based on presence of a draining sinus, high white blood cell count, erythrocyte sedimentation rate, CRP, operative observations, and so on) in the context of supportive microscopic pathology.
DURATION OF SYMPTOMS
Traditionally, infections have been classified according to length of time from surgery. An infection is considered acute if it developed within 3 months of the index operation, subacute if presentation was between 3 months and 1 year, and late if it was recognized 1 year after surgery.27,38 The time interval from the index procedure to the development of infection has traditionally been thought to correlate with the ability to eradicate the infection, but we were unable to demonstrate this in our most recent assessment.6 The duration of symptoms, as in the experience with total knee arthroplasty, has demonstrated a correlation with successful treatment by irrigation and débridement.21,31 Therefore, delineating the onset of symptoms has correlated better with the onset of infection and has direct implications on the treatment strategy.
FIXATION OF COMPONENTS
Component fixation in the context of infection is based on the appearance of the bone cement interface on serial radiographs.6,30 The quality of implant fixation has been enhanced in recent years by the improvement in cement techniques. High-quality and comparison radiographs are necessary for the detection of the progression of radiolucent lines, interval changes in implant position, cortical erosions, and osteolysis, suggesting loosening of the prosthesis. Component retention is, of course, a contraindication with loose or poorly fixed components.
BACTERIOLOGY
The microorganisms of implant infections, as opposed to soft tissue infections, are often difficult to eradicate and continue to be a significant problem. This has been demonstrated in total elbow infections in which the type of organism has had a profound impact on the treatment methods.6,39 Organisms vary in virulence, adherence, and the elaboration of extracellular components. Many factors influence the adherence of bacteria to the prosthesis, including alterations in host immune competence and the ability of bacteria to produce an extracellular matrix.7,13 Unlike total hip and total knee replacements, the infection rate of elbow replacements with gram-negative microorganisms has been low.6,39 Studies of infected orthopedic implants have shown that up to 76% of the infectious microorganisms produce a significant biofilm extracellular matrix to improve adherence to the implant.7,13 Of these, coagulase-negative staphylococci, particularly Staphylococcus epidermidis, have been the most common and the most problematic biofilm producers.13,36
More virulent microorganisms such as coagulase-positive staphylococci (i.e., Staphylococcus aureus) have the capacity to invade and infect healthy tissues but have a lesser ability to form a significant biofilm. Coagulase-negative staphylococcal organisms, particularly S. epidermidis, have been recognized as the primary pathogen of orthopedic device infections owing to their unusual capacity to attach to and to colonize orthopedic implants.2,36 Although a relatively nonvirulent pathogen that normally exists on the skin, it can form a tenacious bacterial biofilm (“slime”), or polysaccharide glycocalyx (protein plus carbohydrate), that envelopes the bacteria. This biofilm promotes colonization and adherence, and protects the bacteria from desiccation and host defense mechanisms.7 It also protects from antibiotic penetration and can even permit adherence to antibiotic-impregnated cement. This accounts for the persistence of S. epidermidis and its resistance to treatment.13 Not surprisingly, the presence of S. epidermidis has thus been associated with high incidence of treatment failure in the setting of infected total elbow arthroplasty,6,39 especially with efforts at reimplantation.6,39 Based on our recent studies,6 in the context of resection arthroplasty for infection followed by reimplantation of total elbow arthroplasty, the most common infecting organism from cultures taken at the time of resection was S. epidermidis (44.8%), followed by methicillin-sensitive S. aureus (24%), and Klebsiella pneumoniae (7%). Negative cultures were found in 10.3%, in which case infection was diagnosed clinically on the basis of wound dehiscence, or a draining wound with an exposed prosthesis. Other organisms accounted for the remaining 14%: group A streptococcus in one elbow, aerobic diptheroids in one elbow, Propionobacter acnes in one elbow, and methicillin-resistant S. aureus in one elbow (Table 62-1).
TABLE 62-1 Distribution of Infectious Organisms in Patients Receiving a Reimplantation Following Management of the Septic Condition
| Organism | Percent |
|---|---|
| Staphylococcus epidermidis | 45 |
| Methicillin-resistant Staphylococcus aureus | 24 |
| Klebsiella pneumoniae | 7 |
| “Other” | 14 |
| Negative culture | 10 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree