Chapter 83 Treatment of Periprosthetic Fractures Around a Total Knee Arthroplasty
The number of primary knee arthroplasties performed annually in the United States continues to increase. It is estimated that 0.3% to 2.5% of patients will sustain a periprosthetic fracture as a complication of total knee arthroplasty.1,11,31 Patient-specific risk factors such as rheumatoid arthritis, osteolysis, osteopenic bone, and frequent falls, common in the older population, and technique-specific risk factors such as anterior femoral cortical notching have all been implicated as potential causes of periprosthetic fractures. The economic impact and disability associated with these fractures is substantial; therefore, having an effective strategy to manage these challenging injuries is important. Typically, fractures occur in the supracondylar area of the femur above a well-fixed total knee arthroplasty (Fig. 83-1).2,18,24 Fractures of the tibia are much less common and are frequently associated with implant loosening.12,17 Decision making regarding the treatment of periprosthetic fractures around a total knee arthroplasty is divided, as noted earlier. In general, patients with fractures around loose implants are considered candidates for revision total knee arthroplasty, whereas fractures around well-fixed implants are candidates for open reduction and internal fixation. Various methods of internal fixation have been described for the treatment of these injuries.5,33 There has been recent enthusiasm for minimally invasive osteosynthesis of these injuries with the use of locked plates. Revision arthroplasty in this setting can be very demanding, with a unique set of technical challenges. The purpose of this chapter is to review the decision making, contemporary techniques, and potential complications of the management of periprosthetic fractures of the femur and tibia around a total knee arthroplasty. Periprosthetic fractures of the patella are discussed in Chapter 67.
Open Reduction and Internal Fixation
Supracondylar Periprosthetic Fractures
The typical clinical situation that the orthopedic surgeon will encounter is a supracondylar femoral fracture above a well-fixed, well-functioning, total knee arthroplasty in an older patient (Figs. 83-2 and 83-3).1,11 Minimally displaced stable fractures and those impacted in good alignment may be candidates for nonoperative treatment. In our experience, however, these situations are rare. Long-leg casting with or without incorporation of a hip guide brace to control leg rotation is recommended. Close radiographic follow-up is indicated, with early surgical intervention if fracture instability is noted. Prolonged attempts at managing unstable fractures with casting may result in further erosion of the distal bone stock and potentially compromise the success of any future reconstruction.

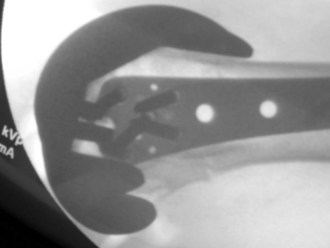
Figure 83-3 Lateral view of the patient in Figure 86-2. Note the fracture at the level of the anterior femoral flange, the most common fracture location.
The principles of treatment of these injuries include obtaining bony union, maintaining correct limb alignment, length, and rotation, and avoiding complications. Surgical challenges to achieving these goals include the often short, osteopenic distal bony fragments, fracture comminution, areas of osteolysis, and parts of the femoral component that can make obtaining stable distal fixation difficult, such as lugs, boxes, and stems. Such fractures usually require an internal fixation device that provides coronal plane stability to avoid the deformity, typically varus collapse, that can occur during the healing process. In the past, devices such as the 95-degree angled blade plate and dynamic condylar screw have been used, with mixed results.*
Because of the extremely distal nature of these fractures, the blade of the blade plate or the lag screw of the dynamic condylar screw must often be inserted more proximally to avoid portions of the femoral component, and thus distal fixation is often suboptimal. The traditional condylar buttress plate offers more freedom of angulation of distal screws but provides no coronal plane stability. Unacceptable rates of varus collapse have been reported when this device was used for unstable fractures.10
Retrograde intramedullary nailing has been used successfully in many series to manage these fractures and offers the advantage of soft tissue–friendly, minimally invasive stability for complex periprosthetic fractures.1,5,11,18–20 Challenges to successful union with intramedullary techniques include the marginal distal fixation provided by locking screws for the typically comminuted, osteopenic distal bony fragments (Figs. 83-4 and 83-5). Also, intramedullary nailing is not practical with implants that substitute for the posterior cruciate ligament because the femoral housing precludes access to the intramedullary canal. We currently reserve intramedullary techniques for fractures above cruciate-retaining designs with sufficient distal bone to allow purchase with a minimum of two distal locking screws. Furthermore, biomechanical evidence has suggested that in the presence of medial comminution, retrograde intramedullary nails may be mechanically more stable than laterally placed locking plates.4 Occasionally, antegrade femoral nailing can be used for periprosthetic distal femoral fractures as well, provided that a sufficiently long distal fragment is present. In our experience, such fractures are extremely rare. The main challenge with antegrade techniques is obtaining appropriate alignment and stable distal fixation. Additionally, with antegrade techniques, an area of high-stress concentration is created between the distal end of the nail and the femoral component.
Locking plate technology has gained popularity for the management of complex periarticular fractures about the knee.* Threads on the screw heads are threaded into corresponding threads in the plate holes, thereby forming a fixed-angle construct and providing coronal plane stability.15 These devices have been used with excellent results for the management of complex periarticular injuries and have an excellent track record for providing reliable distal fixation. Additionally, such devices allow multiple locked screws to be placed around and between portions of the femoral component to improve distal fixation (Figs. 83-6 to 83-8).38 Kregor and colleagues24,25 have reported a series of 38 periprosthetic fractures treated with the Less Invasive Stabilization System (LISS) device (Synthes, West Chester, Pa). There were only two failures (5%). One patient required revision knee arthroplasty and one required bone grafting to achieve solid union. Ultimately, 37 of 38 fractures (97%) healed. Medical and orthopedic complications were uncommon. Leaving metaphyseal comminution undisturbed, thereby preserving vascularity to the fragments, is critical to predictable healing with this technique.
In addition to providing excellent mechanical stability, several locked plating designs also offer the added theoretical biologic advantage of allowing percutaneous insertion.23 This type of insertion minimizes the need for additional large incisions around the knee and potentially minimizes the soft tissue complications and stiffness associated with the traditional exposures used for open reduction and internal fixation.16 When percutaneous techniques are used, vigilance is required to avoid malalignment, typically valgus deformity and hyperextension of the distal fragment. Many commercially available locked plating designs offer the surgeon the option of open or percutaneous insertion. When possible, we perform the internal fixation percutaneously to take advantage of the mechanical stability provided by these devices, as well as the advantages that percutaneous insertion allows.12
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree