Fig. 45.1
Long leg X-rays show lateral opening of the joint space and lateral thrust during walking
Instability may occur during surgery due to accidental damage of soft tissues. Late instability may occur due to trauma, component subsidence or secondary soft tissue stretching or rupture due to overloading.
It remains unclear how much laxity the knee may tolerate in order to remain asymptomatic after TKR. Increased lateral laxity improves flexion in cruciate-retaining TKR [11]. A direct correlation has been reported between lateral joint opening and maximal knee flexion.
It has been shown that patients feel more comfortable with laxer knees after TKR [14]. The varus and valgus laxity ranged from 1° to 10° in this study. On the other hand, no correlation was reported between anteroposterior translation of up to 15 mm and the maximal flexion [8].
The results show that it is still unclear how much instability may be tolerated before loss of function, pain, increase in wear and aseptic loosening may occur [25].
Asymmetric instability should be differentiated from symmetric instability. The treatment of asymmetric instability requires either the tightening or repair of the soft tissue on the loose site or the release of the tight soft tissue on the contralateral site in order to rebalance the knee.
The causes of instability can be summarized as follows:
Asymmetric Instability
1.
Varus instability
Torn lateral collateral ligament (LCL)
Secondary instability due to severe varus malalignment with a tight MCL and lax LCL
Isolated subsidence of either the femoral or tibial component in septic or aseptic loosening
2.
Valgus instability (risk of secondary patella dislocation)
Torn medial collateral ligament (MCL)
Secondary instability due to severe valgus malalignment
Isolated subsidence of either femoral or tibial component in septic or aseptic loosening
3.
Posterior instability (tear of the posterior cruciate ligament)
Symmetric Instability
1.
Mediolateral instability in both extension and flexion
Flexion instability
Extension instability
Midflexion instability
2.
Combined anteroposterior and mediolateral instability after knee dislocation
There are several strategies for treating knee instability after TKR. One may distinguish between ligamentous repair or reconstruction, leaving the components in place or changing the components. Changing the components is the more traumatic procedure for the knee, as it requires removal of well-fixed components. Due to the fact that total constrained implants rely to a smaller degree on function of the collateral ligaments, good clinical outcome can be achieved.
The following options for revision surgery in unstable knees should be considered:
1.
Repair or reconstruction of the torn medial or lateral collateral ligaments.
2.
Tightening and augmentation of the lax soft tissue by using hamstring tendon autograft or allografts. The sliding technique of the medial or lateral epicondyle is another technique to re-tension the medial or lateral collateral ligament by readjusting the femoral insertion site.
3.
Partial revision of the TKR may include soft tissue release of the contralateral side in order to rebalance the knee and use of a higher inlay.
4.
Complete revision of the TKR by replacing the components with a higher degree of constraint, such as a posterior stabilized, total stabilized or hinged TKR design.
Biological repair using hamstring tendon autograft or release of the soft tissue of the contralateral side should be considered. The nonbiological repair means changing the components to a higher constraint design such as posterior stabilized, condylar constraint or total hinged design.
45.1 Medial Instability
Medial instability may occur due to damage of the MCL during surgery or later due to acute trauma or chronic overloading. Secondary instability may occur in severe valgus malaligned TKR due to continuous medial collateral ligament stretching. However, this type of instability is considered to be rare, as varus-valgus laxity typically does not increase over the time [29].
Acute rupture of the collateral ligament due to high stress might be treated conservatively using a brace. The medial collateral ligament may heal conservatively due to the large tibial insertion site and good vascularised surrounding tissue. However, successful primary healing of the MCL after TKR is less likely. Reconstruction of the medial collateral ligament and the posteromedial corner can be performed using the semitendinosus tendon [15]. The semitendinosus tendon is released proximally and remains attached to the pes anserine. The femoral insertion site needs to be identified using an imaging intensifier. After correct placement of the K-wire, a tunnel is drilled, 6 mm in size allowing the insertion of a loop of the tendon. The tendon is fixed ipsilaterally using an interference screw or contralaterally using a button. The free end of the tendon is finally pulled into the canal, which is placed at the insertion site of the deep MCL (Figs. 45.2 and 45.3).
Figs. 45.2 and 45.3
Reconstruction of the medial collateral ligament and the posteromedial corner using the semitendinosus tendon. The tendon is stripped proximally but remains attached to the pes anserinus
A lax but intact MCL may be tightened due to a sliding osteotomy of the medial epicondyle. An osteotomy parallel to the femoral epicondyle allows proximalisation and possibly anterior or posterior shift depending on the tension pattern of the collateral ligament. A similar technique has been described by Mullaji et al. in severe varus malaligned osteoarthritic knees with rigid medial soft tissue structures [22].
Medial instability may also be treated due to lateral soft tissue release in order to rebalance the collateral ligaments. It requires an increase in size of the inlay. However, the procedure is demanding and requires balancing of the ligaments in both flexion and extension. Different sequences of soft tissue release have been proposed. The lateral soft tissue stabilizer consists of:
1.
Iliotibial band
2.
Lateral collateral ligament
3.
Popliteus tendon and posterolateral capsule
4.
Posterior cruciate ligament
Different release techniques have been proposed, mostly based on the surgeon’s personal experience. A few biomechanical studies have investigated the effect of the stepwise release of the anatomical structures at the medial and lateral side. Matsueda et al. recommended the five-step sequential algorithm for the lateral side [19]:
1.
Release of the iliotibial band at joint line level
2.
Release of the popliteus tendon from the femoral side
3.
Release of the lateral collateral ligament from the femoral side
4.
Release of 50 % of the posterior cruciate ligament
5.
Release of 100 % of the posterior cruciate ligament
The effect of the sequential lateral release technique by Matsueda et al. was analysed in a cadaveric study using navigation (Table 45.1) [17]. A total lateral joint space opening of 10 mm was reported in both extension and 90° of flexion after complete release.
Table 45.1
Change of leg alignment (in degree) into varus after sequential release of the lateral soft tissue [17]
Sequential soft tissue release of the lateral side | Amount of varus deflection |
|---|---|
Before the soft tissue release | 1.9 ± 1.9° |
Iliotibial band on the level of the joint line | 4.0 ± 1.6° |
Release of the femoral attachment of the popliteus tendon | 5.6 ± 2.4 |
Release of the lateral collateral ligament from the femoral site | 7.5 ± 1.7° |
Release of the posterolateral capsule from the femoral side | 9.4 ± 1.6° |
Release of the lateral half of the posterior cruciate ligament | 10.4 ± 1.7° |
Complete release of the posterior cruciate ligament | 11.6 ± 1.5° |
A sequential technique similar to the one described by Matsueda was reported by Kanamiya et al. [10] (please see Chap. 50). The release was started with the iliotibial band and followed by the popliteus tendon, lateral collateral ligament and posterior cruciate ligament. A maximum varus deflection of up to 15° and increase in external rotation of up to 20° was observed after complete release [10].
Krackow and Mihalko [13] included in their algorithm of lateral soft tissue release the release of the lateral head of the gastrocnemius muscle.
There is a high risk of joint line elevation, when lateral release is performed excessively in medial instability. The new balanced joint space is much larger than the original one and requires a significantly thicker polyethylene liner. Changing the femoral component and using distal augments for lowering the joint line or changing of both components to a total constraint design has to be considered. Interestingly, the study by Azzab et al. showed that patients undergoing revision for the tibial or femoral component are doing better than those after isolated polyethylene exchange [1].
Lateral sequential release should be performed as follows:Iliotibial band – popliteus tendon – lateral collateral ligament – 50 % of the PCL – 100 % of the PCL
45.2 Lateral Instability
The lateral collateral ligament shows poor healing capability in contrast to the medial one. Direct repair of the lateral collateral ligament of the tendon is not recommended.
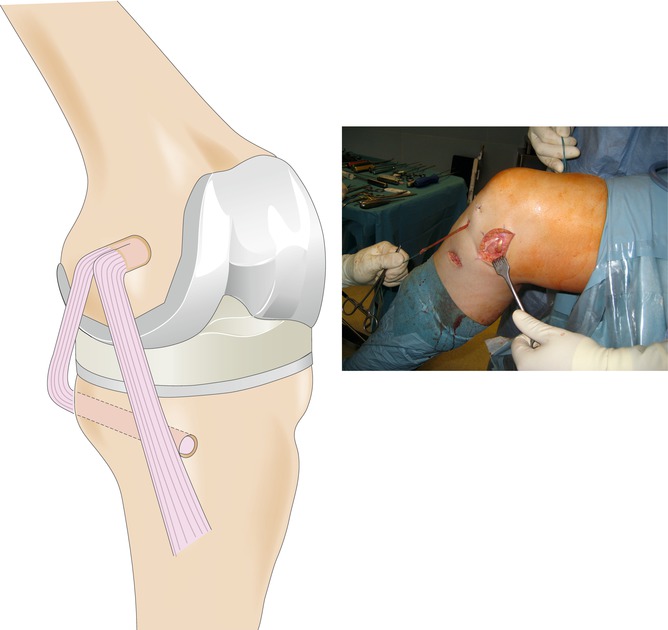
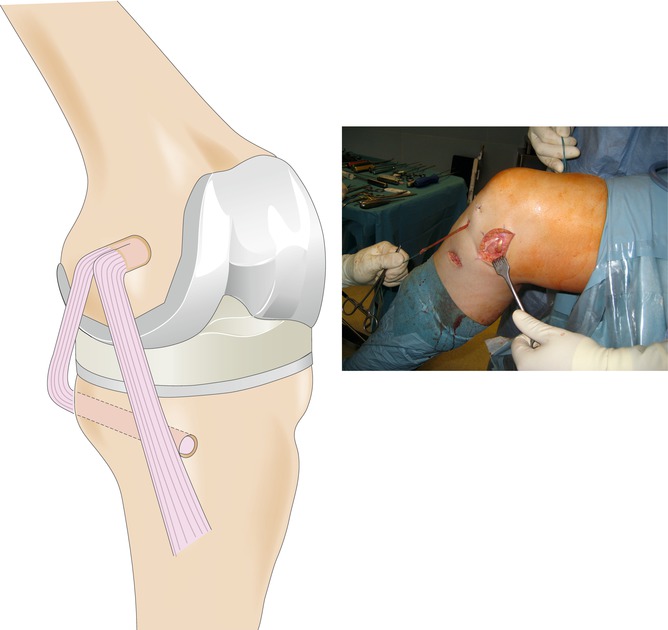
Gracilis or semitendinosus tendon autograft can be used for repair of the lateral collateral ligament. Different techniques have been described [2]. The technique initially described by Slocum and Larson seems to be very reliable when used in a modified way [28, 30].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








