Fig. 44.1
The most challenging problem is when the insertions of ligaments or tendons or the ligaments themselves are affected by osteolytic processes [1]
An underestimated problem deals with the deep medial collateral ligament (dMCL) and the posterior oblique ligament (POL). Their tibial insertion is close to the proximal tibial resection line and is therefore in danger (Fig. 44.2 [2]).
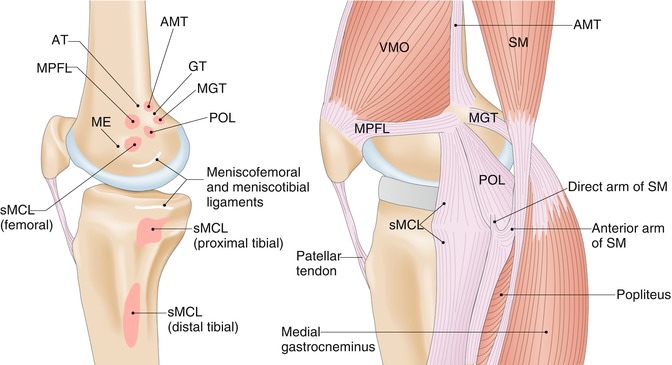
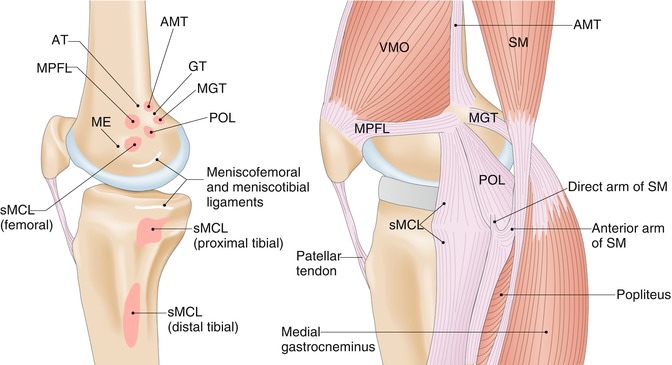
Fig. 44.2
Anatomy of the medial side of knee joint. The medial side: AT adductor tubercle, GT gastrocnemius tubercle, ME medial epicondyle, AMT adductor magnus tendon, MGT medial gastrocnemius tendon, sMCL superficial medial collateral ligament, MPFL medial patellofemoral ligament, POL posterior oblique ligament, VMO vastus medialis obliquus muscle, SM semimembranosus muscle, MGT medial gastrocnemius tendon, AMT adductor magnus tendon
If sufficient stability cannot be restored by positioning and sizing of the TKR components, more constraint is needed. This constraint can vary from a deep dish up to a hinged prosthesis, depending on the amount of instability present.
As long as the medial collateral ligament is intact or can be firmly reconstructed, a hinged prosthesis can be avoided in most cases. Isolated lesions of the deep posterior medial collateral ligament can sometimes be addressed by a posterior stabilized component with a high post and little rotational freedom. The disadvantage of this type of implant is post wear. Therefore, the patient’s activity must be limited.
In extreme circumstances, such as gross instability of the medial collateral ligament, massive bone loss, comminuted fracture, and chronic dysfunction of the extensor mechanism, a hinged revision TKR should be performed [3].
At the distal and posterior, femoral cut augments help to restore the appropriate level of the joint line; stems and cones provide the necessary stability for fixation of the TKR components. At the tibial side, the joint line and the axis can be restored using wedges or cones. Defects can be filled with bone or cement as long as adequate stability is provided by the augmented component (including stems).
44.5 TKR Implant Requirements
With the choice of TKR components two main goals are addressed: Firstly, a stable fixation of the TKR in the remaining bone and, secondly, a well-guided, stable range of motion. This can be achieved either by ligamentous stability or by the constraints of the prosthesis. Because increased constraints influence the longevity of the prosthesis and the activity pattern of the patient, a careful evaluation of the remaining stability of the knee is crucial.
1.
Primary stability of the TKR can be improved by the use of augments, wedges, cones, stems, and cement.
2.
Constraints can be increased to the necessary level from curved inserts to posterior stabilized components up to a hinged prosthesis [4].
3.
Gap mismatch can be addressed by proper sizing and positioning of the components combined with an adequate (or reconstructed) resection level.
4.
Problems with the extensor apparatus can be treated by resurfacing of the patella and proper sizing and positioning of the components (patella, femur, and tibia). The goal is to correct rotational errors at the femoral and tibial side and to avoid overstuffing of the patellofemoral gap. A proper mediolateral position of the femoral component can improve the stability of the patella. More problematic is a patella alta due to a tear of the patellar ligament or an avulsion at the tibial tuberosity.
5.
Changing a patella component is only necessary in well-fixed all-polyethylene patellae if the old component was gamma irradiated in air [5]. If the patellar bone stock is severely altered or there is only a bony shell remaining, in some cases the reinforcement of the remaining bone by a trabecular metal insert can be a solution. It can help to protect the remaining bone and preserve the overall thickness of the patella in order to reconstruct the patellar lever arm. Patellectomy, is strongly advised against, as this comes along with diminished quadriceps strength or disruption of the extensor apparatus [6].
Constraints can be increased to the necessary level, from curved inserts to posterior stabilized components up to a hinged prosthesis.
44.6 Removing Previous TKR Components at Revision Surgery
To avoid damage and bone loss, the removal of TKR components has to be carefully performed using a bone-sparing technique.
Usually, implant extraction starts at the femoral side. After exposure of the TKR implant-cement-bone interface, it is approached by an oscillating saw with a thin, flexible, and short saw blade. Further separation of the interface can be done by thin Simal osteotomes (Fig. 44.3). These osteotomes are carefully placed step-by-step from the medial and lateral side in a way that the separation of the interface can be palpated and visually controlled. Finally, the TKR component can be manually removed, generally without any additional bone loss.


Fig. 44.3
Removal of TKR components at revision surgery using Simal osteotomes
This technique can be used for cemented as well as uncemented TKR components. In cemented TKR, the saw and osteotomes should be placed in the layer between the cement mantle and the TKR component. Specific extractors are rarely necessary at the femoral side. However, press-fit or cemented stems could make the extraction more difficult. Application of heavy forces can lead to extensive femoral bone loss or even breakage of the femoral condyles and hence should be avoided under all circumstances.
After removal of the femoral component, the posterior recess is carefully cleaned of debris and scar tissue to gain sufficient access to the anterior and medial border of the tibial tray. Again, the interface between the tibial tray and cement/bone is separated by an oscillating saw with a thin saw blade. Separation of the proximal tibial interface is finalized using small, flat osteotomes. In nonstemmed tibial TKR components, the tray can be carefully removed without further preparation. In stemmed TKR, loosening of the stem-shaft interface needs to be performed. In some cases slight rotational movements applied by a well-fixed handle are sufficient to allow extraction of a stemmed tibial tray. If this is not successful, you have to decide if you want to separate the stem from the tibial tray with a Gigli saw, which is a cumbersome procedure. Another option is to perform an extended osteotomy of the tibial tuberosity to gain access to the stem. Another decisive key to a safe removal of the tibial component is the exposure of the tibial head. Here the tibial component needs to easily pass the distal femur during removal.
Removal of the patellar component, if necessary, starts again with a small oscillating saw with a thin saw blade to open up the bone-cement/implant interface. Then, a small, flat osteotome can be used to separate the patellar component from the bone.
For removal of the previous TKR components, the femoral and tibial TKR components have to be exposed then separated from the bone or cement using a small oscillating saw and finally loosened using thin osteotomes. For extraction of the components, only gentle hammer strokes should be used.
44.7 Proper Alignment and Choice of Constraints
Intraoperative reassessment of TKR at revision surgery:
2.
Determination and readjustment of flexion and extension gap.
3.
Alignment of the desired flexion-extension axis (transepicondylar axis) and assessment of femoral and tibial rotation and tibial slope (Fig. 44.4: Joint axis [4]).


Fig. 44.4
A combination of the femoral anteroposterior axis, transepicondylar axis, posterior condylar axis, and tibial shaft axis is used to determine the correct femoral component rotation. Deficiencies of the lateral femoral condyle are commonly seen in cases of valgus deformity. This can render the posterior condylar axis inadequate as a sole reference for the determination of the femoral component rotation
4.
Choose the optimal amount of constraint (Fig. 44.5) [4].


Fig. 44.5
The graphic illustrates the continuum of constraint available with TKR implant designs. As the degree of deformity, bone loss, contracture, ligamentous instability, and osteopenia increases, so does the demand for prosthetic constraint [4]
After extraction of the TKR components, the level of the joint line needs to be determined. There are a number of bony landmarks proposed to measure the joint line in revision surgery. Generally, there is a large variation of bony landmarks depending on the size of the knee joint. Hence, these measurements should be compared to the contralateral side. The distance from the tip of the fibular head to the joint line is on average 14 mm. There is no gender difference but a high intervariability. The distance from the joint line to the tibial tubercle is on average 22 mm. The distance from the lateral epicondyle to the joint line is related to the femoral width and is gender related [7]. The mean distance of the medial epicondyle to the joint line is about 30 mm, and the mean distance of the lateral epicondyle to the joint line is about 25 mm [11]. If available, the meniscal scar can also provide the surgeon with some orientation to determine the original joint line.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








