, Paola Catalano1, Andrea Piccioli2, 3, Maria Silvia Spinelli4, 3 and Federica Zavaroni1
(1)
Anthropological Service, Soprintendenza Speciale per il Colosseo, il Museo Nazionale Romano e l’Area Archeologica di Roma, Rome, Italy
(2)
Oncologic Center “Palazzo Baleani” Azienda Policlinico “Umberto I”, Rome, Italy
(3)
The Italian Society of Orthopaedics and Traumatology (SIOT), Rome, Italy
(4)
Department of Orthopaedic and Traumatology, Catholic University Hospital, Rome, Italy
3.1 Introduction
Carla Caldarini5 , Paola Catalano5, Andrea Piccioli6, 7, Maria Silvia Spinelli8, 7 and Federica Zavaroni5
(5)
Anthropological Service, Soprintendenza Speciale per il Colosseo, il Museo Nazionale Romano e l’Area Archeologica di Roma, Rome, Italy
(6)
Oncologic Center “Palazzo Baleani” Azienda Policlinico “Umberto I”, Rome, Italy
(7)
The Italian Society of Orthopaedics and Traumatology (SIOT), Rome, Italy
(8)
Department of Orthopaedic and Traumatology, Catholic University Hospital, Rome, Italy
3.1.1 Historical Development of Osteosynthesis Techniques
For years, the most important principle in the treatment of fractures has been to create appropriate conditions for recovery, which in most cases followed alignment and immobilization. The first techniques in the surgical treatment of fractures were developed at the end of the eighteenth and the beginning of the nineteenth century, and the first fracture osteosynthesis using an iron wire was described in 1827 by Rodgers. The use of cerclage wires to fix fractures has remained popular over time: Malgaigne treated Flaubert for his fracture of the humeral diaphysis using a metallic suture in 1839 [1]. Later on, Lister started using metallic wires to fix fractures in 1870, then Trendelenburg adopted this technique in Germany, and Lucas Championnière in France [2–4]. In all of these cases, “osteosynthesis” meant an open reduction of the fracture followed by a very unstable fixation with cerclage wires. This method involved the combination of the disadvantages associated with conservative treatment, and the risks associated to surgery.
History of Medicine: Fracture Care
Valentina Gazzaniga and Silvia Marinozzi
Displacements, due to dislocations or bone fracture, are firstly treated with extension trying to set the limb in the right position, that is the most physiologically correspondent, considering the muscle retracted tension and contraction which could impair the right repositioning of the bony stumps, and the tendon and muscle lesions which could develop after twistings or changes of place, so severe to tear them and not to allow the right bone repositioning.
According to ancient sources, the right technique is to lay the muscular fibres in a straight line, to check the contraction and get an adequate reduction. Then the part is immobilized, in different ways depending on type and affected region, and broad-spectrum therapies are prescribed, considering the humoural theory of the ancient medicine disease. Diet, phebotomy, laxatives and diuretics draw corrupted humours away from the wounded area but lead to inflammation and can impair the healing to degenerate in gangrene.
Both Celsus and Galen prescribe a diet rich in light foods, infusions and drinkings with laxative and diuretic properties to draw corrupted humours away from the lesion area, leading to inflammation.
The fracture is treated with ointments and waxed to ease the suppurative process and exsiccative to fight inflammation. According the Hippocratic tradition, wine and oil based ointment and base waxed preparations, or wax, oil, rose water and other anti inflammatory substances (dry, astringent and hot are often used). Galen is particularly concerned about bandaging technique, carried out to hold but not compress a fracture, to avoid flesh inflammation and lesion (De Off. Med. II, 6–12 – K. XVIII/B: 738–758; De Medendi methodo, VI,4 – K. X: 423–444)
Open Fractures
In open fractures, a high risk of inflammation and necrosis is due to the resulting wounds and inflammation process. To medicate the lesions, greasy wool compresses are recommended, which have soothing properties as oil, soaked in red and row wine, less penetrating than the white one, and so less irritating, but exsiccative and purgative in the same way. Galen uses cooked or raw virdigris too, for its exsiccative, restraining and antiseptic property; with clear inflammation, a pitch-based wax, less penetrating and detergent, but soothing and palliative. A piece of leather is put under the limb to let the absorption of the humours and of the pharmacological liqueurs used.
For the limbs reduction, Galen uses a tool made of two leather rings to extend the bone far ends, concave or perforated to insert different length sticks depending on the anatomical structures and made of wood elastic enough to be put in the slightly curved rings, to make a natural pressure which, alone, can lead to the bones extension (Galen, De Fracturis, III, 27–32 – K. XVIII/B: 573–583; Celsus, VIII, 10,7; 25). Some physicians treat the wounds only with wood and soothing wax-based preparations, extend the bones only after 3 days, when needed. On the other hand, Galen immediately reduces the fracture, repositioning the bones with appropriate orthopaedic tools: levers to raise or lower the bone stumps during the extension; a wedge, to remove bony fragments and splinters which can lead to further flesh lesions, the wheel with the axle (Galen, De Fracturis, III, 38–40 – K. XVIII/B: 590–594).
Celsus cuts and smooths the sharp ends with the scalpel and, if the hand cannot get them, he holds the bones with pincers, which, in the convex part, are also used to raise and reposition the bony stumps. The wound is continuously washed to move the spoiled parts away, when there are rotting fragments; if the stumps do not come out but the inner bony splinters injure flesh and muscles, fomentations are carried out with cold water in the summer and cool water in the winter, applying a myrtle oil and wax based preparation and in the most severe cases the skin is cut and the splinters are resect. When the wound outcome involves a shortening of the limb because of dislocation or resection of the bones splinters, a little smooth stake is pushed deeper and deeper in the wound every day, to separate and align the two stumps; every day the wound is treated with myrtle, ivy and other verbenaceae dissolution as long as a bony callus develops. When a simple mechanical bone reduction is unsuccessfull, the extension is carried out manually detaching the consolidated parts of the bones and curetting the greasy part (callus) developed to disconnect and reposition them; then the wound is treated with albumen and pomegranate peel solution boiled in wine; dressed with the canonical bandage, from the third day, during the treatment fomentations are carried out with warm water, where verbenaceae have been boiled in and ferulas are put on the fifth day. If the bones are obliquely consolidated and tear the flesh, after the application of fomentations and liquid waxed packs, they are detached by the hands breaking the bony callus and during the extension they are handled to reposition them; if needed, the limb is dressed with a splint which presses on the protruding bone to align it. To treat or prevent an over growth of the bony callus, oil, salt and nitre frictions, salted water fomentations, pharmacological doughs medications are carried out together with a tight bandage, following a vegetable-rich diet and taking vomitives to drain plethoras away (overabundance of humours) localized on the fracture (Celsus, VIII, 10,7)
The bandage is similar to the one carried out for simple fractures, but with less pressure to avoid muscular and flesh lacerations and too severe inflammation; moreover, a greater number of bandage is used because wooden rods cannot be put on the wound (Galen De Fracturis, III 1–2 – K. XVIII/B: 532-–35). For more severe compound fractures, with spread and deep flesh lesions, Galen does not carry out any reduction operation, which could lead to “spasm”, a muscular contraction so severe to tear the vessels and flesh and cause acute inflammation which can degenerate in gangrene. In these cases, also bandage can be dangerous, because of its flesh compression against the splintered bones with the failure of the humours to draw away, with severe and damaging plethoric phenomena. So the leg is only lain straight on the bed, the patient is only put on a fast and the wounds are treated with ointment, tepid waxed, greasy wool soaked in oil and wine. Galen uses pitch-based ointments, compresses soaked in wine, chard and coltsfoot (tussilago farfara) and advices perfusion remedies, to penetrate to the recent sores, and not too much exsiccative, to avoid spasmodic outcomes. So, he uses the “barbaric” one, bitumen based but emollient (Galen De Fracturis, III 3–26 – K. XVIII/B: 535–573; Galen, De Articulis, IV, 15–30 K. XVIII/A: 683–712; Celsus, VIII, 25).
3.1.2 Intramedullary Nailing
Intramedullary fixation methods were developed at the end of the nineteenth century. In 1883, Stimson was the first person who described a synthesis method with ivory hinges fixed into the medullary cavity [5], but it was Ernest Hey-Groves who first used metal nails in 1912 [6]. The “true” intramedullary fixation technique, with the use of an intramedullary nail, was developed in the 1930s independently by the Rush brothers in Minnesota and by Gerhard Küntscher in Hamburg [7, 8], and this method was used and experimented on a large scale during World War II. The method became popular thanks to Klemm and Shelman, and Gross and Kemf in the 1970s [9, 10].
3.1.3 The External Fixator
Many surgeons were perplexed about the use of intramedullary nails in subjects with exposed fracture focus. In the first few years of the 1950s, Gavrijl Abramovich Ilizarov developed a circular fixator, which allowed to stabilize bone fragments, but also allowed three-dimensional reconstructions. In 1980, the technique was introduced to Europe thanks to the Italian surgeon Carlo Mauri, who had been treated successfully after a pseudo-arthritis of Ilizarov tibia. During the 1970s, De Bastiani developed the “dynamic axial fixator”, and Gotzen the “Monofixator” [11]. Nowadays the external fixator is still used in the treatment of fractures associated to a large range of soft tissue damages, and in the fixation of hip and long bones in poli-traumatized patients.
3.1.4 Plaques and Screws
Arbuthnot and Lambotte (1905) are considered the founders of synthesis with plaques and screws [12]. Later on, the principle of inter-fragmentary compression, described by Danis, became extremely popular thanks to the scientific work of the AO team at the end of the 1950s [13]. In 1967, Schenk and Willenegger demonstrated that, in anatomical reduction and with inter-fragmentary compression, bone necrosis and retraction are reduced, and the bone tissue growth occurs fast, thus leading to primary bone recovery without callus formation [14].
3.1.5 Conclusion
The healing of fractures needs some optimal conditions, which include stabilization, fragment juxtaposition, and a correct biology. Since the pioneers of traumatology, further synthesis means and more and more sophisticated and minimally invasive fixation techniques have been developed. Thanks to their contribution, in the last few years the development of new osteosynthesis techniques has allowed to achieve better and better immobilizations, and juxtaposition between the fracture heads, thus allowing the immediate load and a fast functional recovery.
3.2 Fracture of the Nasal Septum
3.2.1 Morphological and Palaeopathological Description of the Subject
The subject is male, and has a strong skeleton, even though the muscular insertions are generally poorly developed. On the inferior surface of the right clavicle, the rhomboid fossa lies as a deep depression with jagged margins and a rough surface, while the contra-lateral area is slightly porous and defined by irregular margins. These lesions [15] indicate generalized stress on the pectoral muscle, particularly when the shoulders are hunched forward while carrying heavy weights [16, 17]. Among the muscles involved in plantar flexion, the only one showing mild variations is the soleus muscle; the rest of the appendicular skeleton – both superior and inferior – does not show any enthesopatic alterations. Even though most somas of the thoraco-lumbar vertebrae were destroyed post-mortem, three Schmörl hernias have been detected, and these can probably be associated to the ponderal overload, in particular to the strain of carrying heavy weight on the back [18]. A massive periosteal reaction with new bone production is observable on the diaphyses of tibias and fibulas: there is a thick layer of bone tissue, characterized by irregular surfaces and thin spicules, lying perpendicularly to the cortical. Periostitis is more commonly found on the anterior surface of the tibial diaphysis.
Among the anatomical variants, the morphology of the first left rib is peculiar, as it shows a fork, with rounded corner at the sternal extremity (Luschka rib) [19]; since the body of the bifurcated rib (Fig. 3.1) is as tall as the contra-lateral, it is not a case of complete fusion of two consecutive ribs. The cranial and transverse fronto-parietal indices of the skull have intermediate values, which indicate mesocrany and metriometopy respectively, while the height index suggests a high skull (hypsicranic). The frontal crests diverge, the orbits are large, and the piriformis aperture is long and narrow (leptorrhine). A fracture can be seen on the nasal bone, with a deviation of the septum to the left (Fig. 3.2).

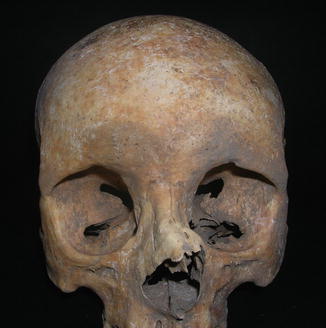

Fig. 3.1
Bifurcated rib
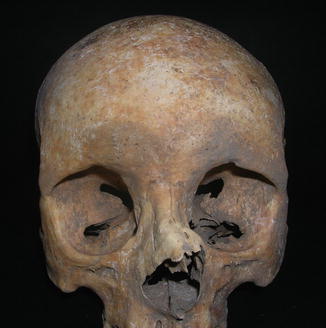
Fig. 3.2
Nose fracture
3.2.2 Description of the Fracture
The clinical case shows a deviation of the nasal pyramid on the left. The likely presence of bone callous on the surface suggests the hypothesis of a post-traumatic deviation as a consequence of the fracture of the pyramid, rather than a congenital deviation of the nose (Fig. 3.2). The most common dynamics is a direct trauma in the direction of the deviation (e.g. a punch on the nose). Among the fractures involving this region, the fracture with a deviation of the pyramid is the most common one, and it involves both nasal bones, the septum, and sometimes the frontal process of the maxillary sinus. The acute clinical case shows swelling, bruising and bleeding from laceration of the nasal mucosa and can hide the deformity, thus delaying a manual correction and resulting into deformity after swelling resolution. On top of the aesthetic damage, this type of fracture determines an obstruction of varying degree of one or both nasal cavities. The deviation can be clearly seen macroscopically, and from a radiology (Figs. 3.3 and 3.4), which only shows lateral deviation and does not allow further assessments due to the overlapping of several bone structures.

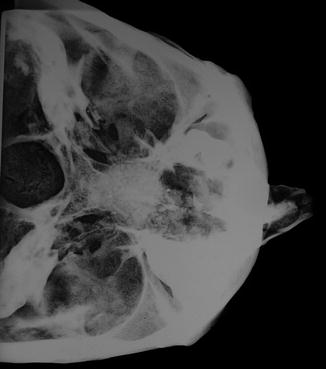

Fig. 3.3
X-rays (lateral view) of the nose
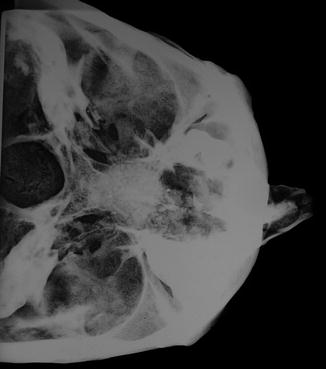
Fig. 3.4
X-rays (axial view) of the nose showing its lateral deviation on the left
3.3 Fracture of the Humerus
3.3.1 Morphological and Palaeopathological Description of the Subject
The subject is averagely built, with round-shaped humeri (euribrachy), and flattened femurs antero-posteriorly (platimery). The skull is high (hypsicranic) and elongated (dolichocranic), with averagely diverging frontal crests, the orbits are large (hypsiconchic) and the nose shows a long and narrow piriformis aperture (leptorrhine). The hypoplasia of the enamel and the simultaneous presence of cribra cranii and orbitalia suggest episodes of generalized suffering occurred during early childhood. The subject’s health is characterized by the presence of a few dental caries, the likely cause of the loss of several teeth intra-vitam. A large cavity affected the first left maxillary premolar, and its alveolus shows osteolisis, probably caused by an odontogenic abscess (Fig. 3.5) [20]. The deltoid tuberosity of the clavicles is irregular, with small enthesopathic bone spicules associated to erosions, and the insertion area of the pectoralis major muscle shows a strong, flattened surface. The infraglenoid tubercle of the right scapula highlights a wide, marked ruggedness at the insertion of the long head of the triceps brachii. The insertion area of the pectoralis major on the humerus is marked and rough bilaterally, the surfaces of the lesser and greater right tuberosities, where the muscles of the rotator cuff are attached, show alterations with erosions and ruggedness. The left ulna shows a mild enthesopatic ossification, implanted on the upper margin of the posterior facet of the olecranon (woodcutter’s lesion) [21]. The enthesopaties detected on the upper limbs affect the muscles promoting adduction and anteversion movements of the arm and extension of the forearm on the arm. The lower limbs do not show signs of any relevant muscular stress, even though the antero-posterior flattening of the superior third of the femoral diaphysis is generally associated to a strong development of the trochanters due to biomechanical stress. A pathological anomaly involves both patellas, where the superior lateral ossified nucleus is not welded to the rest of the bone (bipartite patella) (Fig. 3.6): in that area the margin is rough and eroded [22]. A small sessile ossification, 22 mm long and 8 mm wide, is situated on the cortical of the left femur’s posterior face (myositis ossificans) (Fig. 3.7): a traumatic episode, probably limited to the soft tissues, may have caused a haematoma, with the production of a calcification of the torn muscular tissue [23]. The subject has some mild arthritic degenerations, which are confined to a few skeletal regions. A widespread porosity on the sternal and acromial extremities of the clavicles, on the glenoid cavity of the scapulas and on the humeral heads are all signs of suffering of the shoulders’ joint cartilage. There are mild degenerations on the hip joints, with erosion and reshaping of the femoral heads and of the acetabulum. The bodies’ ventral margins and the articular facet of some cervical and lumbar vertebrae show small osteophytes. The thoracic vertebrae do not show any somatic alterations, except for the three small imprints of intraspongeous hernias and small laminal spurs on the superior border, in the insertion points of the inferior ligamenta flava.



Fig. 3.5
Odontogenic abscess

Fig. 3.6
Bipartite patellae
Fig. 3.7
Consequence of potential myositis ossificans
3.3.2 Description of the Fracture
The fractures of the distal humerus account for 2 % of all fractures and 1/3 of the humeral fractures [24]. The direct trauma mechanism is the most common, while less frequently the indirect one, due to rotation traumas, leads to spiral or oblique fractures.
The clinical case shows the consequence of a fracture of the distal third of the right humeral diaphysis (Fig. 3.8). This site represents the least common one if compared with the fractures of the other two segments of the humeral diaphysis, the middle third (most common) and the proximal third (second most common). The fracture looks well healed, with bone callous formation, thus suggesting a secondary bone healing. The bone callous progress, though partly reshaped, looks like the type of fracture that could have been oblique or spiroid, meaning an indirect rotational trauma. There might have been a third fragment on the medial profile, where the callous is most overabundant. This hypothesis can be supported also by the slight varus deviation of the distal part of the segment. The remaining axes of the segment look well preserved, and the healing of the fracture clears (Fig. 3.9). This recovery picture does not show any alterations in the limb’s function.

Fig. 3.8
Fracture of the right humerus

Fig. 3.9
X-rays of the humerus antero-posterior view shows consequences of a fracture of the distal third of the bone segment with a mild varus deviation
3.4 Fracture of the Radius and Ulna
3.4.1 Fracture of the Medial Third of the Radius and Ulna
3.4.1.1 Morphological and Palaeopathological Description of the Subject
The subject is of average build, with particularly marked muscular imprints only at the pectoral girdle and at the upper arms. The clavicles and humeri show enthesopaties at the origin and insertion of the deltoid and subscapularis muscles, which are used respectively, for abduction and rotation of the arm. The inferior appendicular skeleton does not show any enthesopathic alterations, even though the femurs reveal an antero-posterior flattening of the diaphyseal superior third (platimery).
The presence of only two Schmörl’s nodes at the thoracic tract of the spine, together with a mild degree of arthritis, suggests a low ponderal and functional load of the column. The extra-vertebral arthritis, limited to the shoulders joint, may be linked to the subject’s advanced age.
The marked preauricolar grooves of the ileum, the hypertrophy of the pubic tubercle and the depressions of the hind symphysis area may be the signs of birth giving; tooth cavities and the loss intra-vitam of several teeth, may result from a calcium deficiency due to pregnancies [25–27].
The examination of the maxillary dento-alveolar complex, shows two abscesses, on the right first and second molar and the agenesis of the left second incisor and first molar. The height and horizontal cranial indices have average values (mesocranic and orthocranic) and the frontal crests are averagely diverging.
In addition to the fracture of the left radius and ulna, the palaeopathological study shows a likely muscular trauma of the diaphyseal distal third of the right fibula, three right rib fractures and one left rib fracture.
3.4.1.2 Description of the Fracture
This case shows a biosseous fracture of the diaphyseal medium third of the radius and ulna with synostosis and calcification of the interosseous membrane (Fig. 3.10 a, b). Radius and ulna fractures may lead to several complications, including Volkmann Syndrome, which is the most severe one, and post-traumatic radio-ulna synostosis, which is rather infrequent, since its incidence accounts for 3–9 % [28].


Fig. 3.10
(a) Consequence of radio-ulna diaphyses fracture with synostosis (b) Detail
The most common risk factors associated with this complication are as follows:
Fracture of both segments at the same level (11 %, that is the most common risk factor)
Delay in fracture consolidation
Closed cranial trauma, which increases the rate of formation of heterotopic ossifications
“Crush syndrome”, with severe damage to the soft tissues, and pluri-fragmented fracture
Lesion to the interosseous membrane
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








