Traumatic Anterior Instability: Arthroscopic Solutions
Augustus D. Mazzocca
Robert A. Arciero
Brian J. Cole
A. D. Mazzocca: Department of Orthopaedic Surgery, University of Connecticut, Connecticut.
R. A. Arciero: Department of Orthopaedic Surgery, University of Connecticut, Connecticut.
B. J. Cole: Department of Orthopaedic Surgery, Rush Presbyterian-St. Luke’s Medical Center, Chicago, Illinois.
INTRODUCTION
Instability of the shoulder is a common and complex problem. Classifying traumatic unidirectional instability from those patients with a traumatic multidirectional instability is important in the successful treatment of these patients.34 One of the most common mechanisms of an acute dislocation involves a collision or fall when the arm is in an abducted and externally rotated position. Although open Bankart repair has been the gold standard for treatment of this problem, arthroscopic techniques have improved and now provide results approaching the open method. The main tenet of the arthroscopic technique is to perform the same procedure that is done in the open technique, using arthroscopic methods. This entails the use of suture anchors, permanent sutures, and a method to address capsular redundancy. This will allow the surgeon to have all of the advantages of the arthroscopic technique while also assimilating all of the advantages of the open technique.
This chapter will review the pathology and biomechanics of specific lesions encountered in patients with traumatic anterior instability. It will review various imaging techniques for assistance in preoperative planning. The chapter will describe various arthroscopic techniques for capsular plication, anterior labrum repair, and rotator interval closure. Rehabilitation, postoperative care, results of surgery, and complications will also be detailed.
PATHOLOGY OF ANTERIOR INSTABILITY
This section will describe the specific pathoanatomy associated with various diagnoses. Understanding the anatomy and biomechanics of lesions observed in patients with traumatic anterior instability will facilitate repair of these lesions, essential in a successful outcome. The arthroscope is a tool that will allow the surgeon to evaluate tissue both visually and tactilely.
The overall stability of the glenohumeral joint involves passive and active mechanisms. Static or passive factors include joint conformity, adhesion/cohesion, finite joint volume, and ligamentous restraints, including the labrum.35 The ligaments and capsule are aided by receptors that provide proprioceptive feedback. When capsuloligamentous structures are damaged, alterations in proprioception occur that is partially restored with operative repair.29 The active mechanisms are primarily provided by the rotator cuff muscles. The static stabilizers are affected by congenital factors, which include glenoid hypoplasia, and disorders of
collagen structure that result in excessive joint laxity. The severity of the instability pattern may be influenced by patient age, seizure disorders, and psychological or secondary gain factors.
collagen structure that result in excessive joint laxity. The severity of the instability pattern may be influenced by patient age, seizure disorders, and psychological or secondary gain factors.
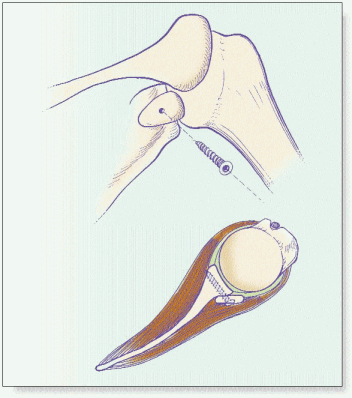
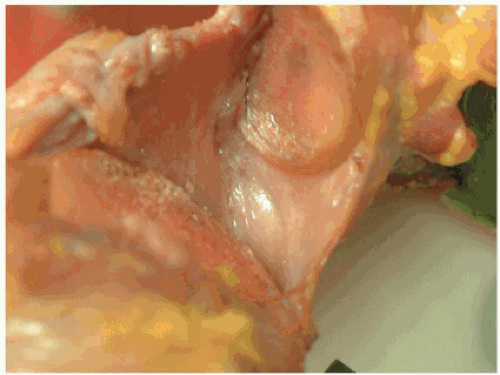 Figure 1-1 Cadaveric image of the inferior glenoid humeral ligament (IGHL) and anterior inferior labral complex. |
The Bankart Lesion
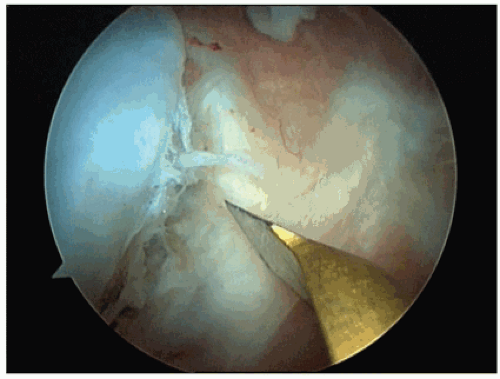
The inferior glenohumeral ligament (IGHL) complex is the primary ligamentous restraint to anterior glenohumeral translation, specifically with the arm in an abducted and externally rotated position60 (Fig. 1-1). The specific anatomy of the IGHL has been described as having anterior and posterior bands with an intervening axillary pouch.41 In a classic description of the pathology associated with a traumatic anterior dislocation, detachment of the anterior-inferior labrum and capsule (comprising the anterior band of the IGHL as a capsulolabral complex) is considered one of the major pathoanatomical features. This has subsequently been named the Perthes-Bankart lesion5,43 (Fig. 1-2).
The mechanism of how the Bankart lesion leads to instability has been studied extensively. A study was conducted that demonstrated that detachment of the anterior inferior labrum and capsule from the glenoid resulted in a nearly doubling of anterior translation. A Bankart repair was then performed, repairing the anterior IGHL and labrum back to the glenoid, which restored glenohumeral stability.21 In a follow-up study, the strain before failure for all bone-ligament-bone preparations was 27% in a cadaver study, and the authors concluded that plastic deformation of the capsule was a fundamental component of anterior instability.6 This is an important concept in capsular plication. It is important to mention that, in contradiction to Harryman’s study, Speer et al. reported that, after creating a Bankart lesion, there were only small increases in anterior translation when the specimens were loaded. These data have not been duplicated.
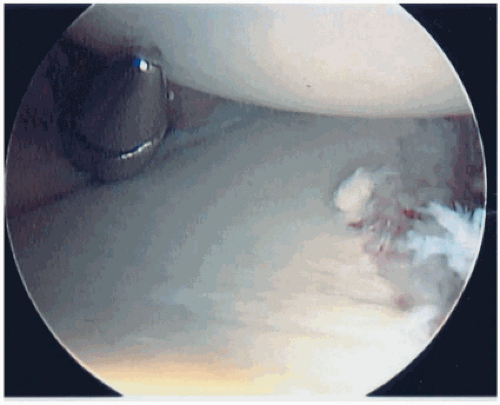
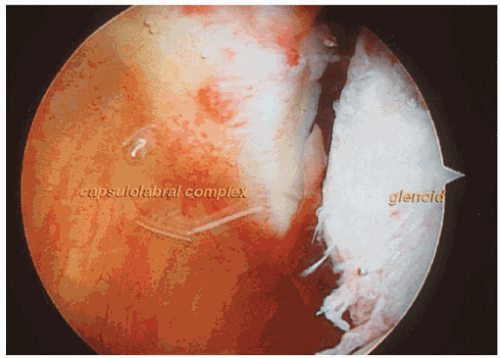 Figure 1-2 Arthroscopic view of a Bankart lesion, left shoulder, sitting position viewed from posterior (70-degree arthroscope). |
There was also some evidence that suggests that age plays a role in the type of pathology seen with anterior dislocations.21,52 Age has been determined to have an impact on instability. In a 1969 study of young and old primates, Reeves observed that IGHL detachment occurred in young shoulders and that the capsular ligaments tended to tear in the older ones.44 In a similar study of computed tomography (CT) arthrograms in humans, Ribbans found avulsion of the anterior glenoid labrum in 100% of the young patients and 75% of the older ones (greater than 50 years old).45 Associated fractures, tears of the rotator cuff, and capsular injuries were more common in those patients over 50 years of age.
Neviaser in 1993 added a differentiation between the Bankart lesion and what he termed the anterior labral ligamentous periosteal sleeve avulsion (ALPSA) lesion (Fig. 1-3).
In his description of both acute and chronic anterior dislocations, the anterior scapular periosteum does not rupture as in a Bankart lesion, and the anterior IGHL, labrum, and the anterior scapular periosteum are stripped and displaced in a sleeve-type fashion medially on the glenoid neck. This is an important diagnostic variant to recognize, because, in a chronic situation, a cursory inspection of the anterior inferior quadrant of the glenoid may not reveal evidence of trauma. However, closer inspection more medially will elicit a large, scarred labrum on the anterior portion of the glenoid neck38 in a medial location.
In his description of both acute and chronic anterior dislocations, the anterior scapular periosteum does not rupture as in a Bankart lesion, and the anterior IGHL, labrum, and the anterior scapular periosteum are stripped and displaced in a sleeve-type fashion medially on the glenoid neck. This is an important diagnostic variant to recognize, because, in a chronic situation, a cursory inspection of the anterior inferior quadrant of the glenoid may not reveal evidence of trauma. However, closer inspection more medially will elicit a large, scarred labrum on the anterior portion of the glenoid neck38 in a medial location.
Superior Labrum Extension
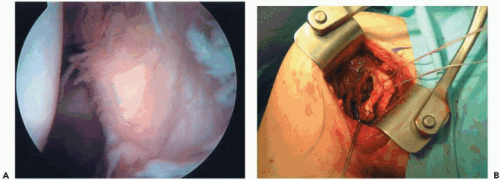
The advantage of an arthroscopic examination of the shoulder joint frequently leads to observations of additional lesions associated with anterior instability. Occasionally, the injury may extend inferiorly into the capsule or the axillary pouch. Taylor and Arciero reported one capsular tear in a series of 63 primary shoulder dislocations.56 These same authors described injuries that may also extend superiorly into attachment of the biceps tendon, producing a concomitant superior labrum anterior posterior (SLAP) lesion (Fig. 1-4, A and B). This lesion is generally observed when the dislocation involves an extreme type of trauma.14
In a variation of the anterior superior labrum lesion, the anterior supraspinatus can have partial or complete tears resulting in various amounts of instability. This has been called the SLAC (superior labrum, anterior cuff) lesion. This can be caused by both acute and chronic trauma and is addressed with suture anchor fixation.51
Humeral Avulsion of Glenohumeral Ligament Lesions
A third type of lesion can be observed, which is a lateral detachment of the IGHL from the humeral neck.39 This has been subsequently described as a humeral avulsion of glenohumeral ligament (HAGL)3,32 lesion (Fig. 1-5, A and B). Nicola described this entity and its proposed mechanism in 1942.39 A force applied in continued abduction tears the capsule from the neck of the humerus. A force started in abduction of 90 to 105 degrees, supplemented by impaction, tears the capsule from the neck of the humerus. Bach, in 1988, reported two cases fixed by open repair.3 Wolf et al., in 1995, found an incidence of 9.3% in a series of anterior instability patients. They also described an arthroscopic technique for repair. In this repair, a standard anterior inferior portal is made, and the bone is burred through this portal. An anterior lateral portal is created 2 cm lateral and 2 cm inferior to the coracoid process. A suture hook places monofilament absorbable suture through the capsule, and these are tied through the anterolateral portal over the subscapularis tendon.63 Both Field and Warner, in 1997, cited case reports of anterior instability treated with open techniques. Bokor et al., in 1999, reported 41 cases of a HAGL lesion in 547 shoulders, an incidence of 7.5%. Bui-Mansfield, in 2002, in a retrospective review of 307 patients with anterior instability, identified six cases, an incidence of 2%. Although relatively rare, this lesion must be examined for any anterior instability arthroscopic case. Taylor and Arciero described HAGL lesions after an acute anterior dislocation.56
Traumatic Bone Deficiency
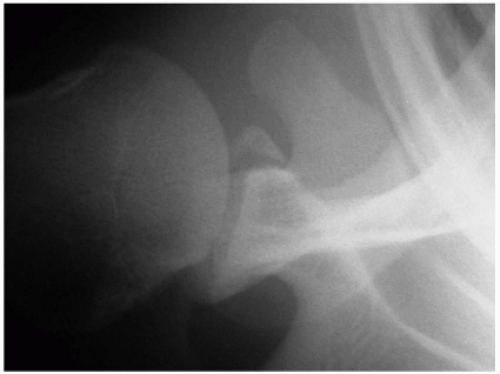
Fractures or various bone deficiencies can exist, involving both glenoid and humeral surfaces (Fig. 1-6). The anatomy of the glenoid and proximal humerus is consistent. The articular surface of the proximal humerus is similar to that of a sphere. It is composed of cartilage, subchondral and trabecular bone and is relatively soft even in young athletes. The glenoid has a consistent morphology
as well. It is pear-shaped with the inferior portion approximating that of a true circle enface.55 Bone lesions of the glenoid or humeral head place greater demand of soft tissue repairs and have been shown to cause recurrent anterior instability of the shoulder.6,23,50
as well. It is pear-shaped with the inferior portion approximating that of a true circle enface.55 Bone lesions of the glenoid or humeral head place greater demand of soft tissue repairs and have been shown to cause recurrent anterior instability of the shoulder.6,23,50
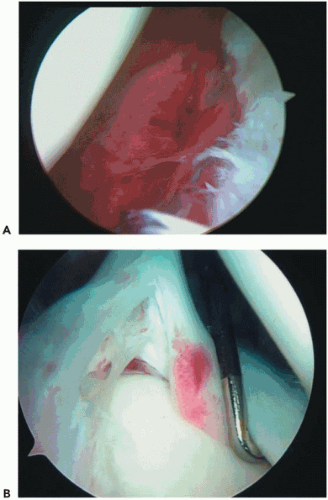 Figure 1-4 (A) Arthroscopic capsular tear. Sitting position, left shoulder viewed from posterior. (B) Arthroscopic superior labrum anterior to posterior lesion (SLAP), type IV. |
Humeral Bone Deficiency
The Hill-Sachs lesion is found on the humerus and is an impression fracture caused by the humeral head being dislocated anterior and impacting on the anterior glenoid. This is generally located on the posterior superior part of the humeral head. Burkhart and De Beer reported and defined what they describe as an engaging Hill-Sachs lesion, defined as a lesion in a functional position of abduction and external rotation. The long axis of the Hill-Sachs lesion is parallel to the glenoid and engages its anterior corner. A nonengaging Hill-Sachs lesion is where the impression fracture occurs when the arm is in a nonfunctional position of shoulder extension or shoulder abduction is less than 70 degrees. The nonengaging Hill-Sachs lesion passes diagonally across the anterior glenoid with external rotation, so there is continual contact with the articular surfaces. These shoulders are reasonable candidates for arthroscopic Bankart repair.9 It is important to understand that the Hill-Sachs lesion is created by the position of the arm when the dislocation occurs. The Hill-Sachs lesion that develops when the arm is at one’s side but with some extension of the shoulder will be located more vertically and superiorly than the lesion that occurs with the shoulder abducted and externally rotated. The Hill-Sachs lesion that develops with the arm at the side is generally a nonengaging lesion.
Burkhart and De Beer report three ways to address the engaging Hill-Sachs lesion. The first is with an open capsular shift procedure that restricts external rotation, not allowing the lesion to engage. The second approach fixes the impression fracture with a size-matched humeral osteoarticular allograft, which is reserved for large defects. The third is a rotational proximal humeral osteotomy that internally rotates the articular surface of the humerus.
Glenoid Bone Deficiency
Two types of lesions can occur involving the anterior inferior glenoid: the impression fracture and the avulsion fracture. The compression Bankart lesion is secondary to compression of the anterior inferior bony articulation of the glenoid or the humeral head. Repeated episodes of instability create the “inverted pair” lesion as well as a typical bony Bankart. Investigators in the past have recommended coracoid
transfer when the glenoid rim fracture comprised 25% of the anterior/posterior diameter of the glenoid.7 Burkhart et al. comment on the containment of the humeral head by the glenoid as a result of two geometric variables.10 The first is the deepening effect of a wire glenoid due to the longer arc of its concave surface; the second is the arc length of the glenoid itself. They caution in their article that if the bony fragment is excised or if there is an “inverted pair”-shaped glenoid, and if there is no bone augmentation, arthroscopic techniques may fail (Fig. 1-7). To diagnose this arthroscopically, the arthroscope is placed in the anterior superior portal, looking inferiorly on the glenoid. The bare spot of the glenoid is roughly in the center of the glenoid, and, with a calibrated probe, the distance from the anterior rim of the glenoid to the bare spot is measured, as well as the distance from the bare spot to the posterior glenoid rim. If there is a 25% reduction in the length from the anterior glenoid to the bare spot compared to the bare spot to the posterior glenoid, a bone procedure is indicated.10
transfer when the glenoid rim fracture comprised 25% of the anterior/posterior diameter of the glenoid.7 Burkhart et al. comment on the containment of the humeral head by the glenoid as a result of two geometric variables.10 The first is the deepening effect of a wire glenoid due to the longer arc of its concave surface; the second is the arc length of the glenoid itself. They caution in their article that if the bony fragment is excised or if there is an “inverted pair”-shaped glenoid, and if there is no bone augmentation, arthroscopic techniques may fail (Fig. 1-7). To diagnose this arthroscopically, the arthroscope is placed in the anterior superior portal, looking inferiorly on the glenoid. The bare spot of the glenoid is roughly in the center of the glenoid, and, with a calibrated probe, the distance from the anterior rim of the glenoid to the bare spot is measured, as well as the distance from the bare spot to the posterior glenoid rim. If there is a 25% reduction in the length from the anterior glenoid to the bare spot compared to the bare spot to the posterior glenoid, a bone procedure is indicated.10
Version and Hypoplasia Lesions
Increased glenoid retroversion and glenoid hypoplasia have been implicated in posterior or multidirectional instability.
IMAGING
Radiographs
Radiographic evaluation is required in assessment of shoulder instability. Fractures as well as assessment of anatomy are critical to evaluate prior to treatment. A standard anterior-posterior view of the arm in slight internal rotation is used to identify a fracture of the greater tuberosity. A true scapular anterior-posterior radiograph permits evaluation of a glenoid fossa fracture, if present. The West Point axillary view is used to assess bony avulsions of the attachment of the IGHL or bony Bankart lesions,47 or anterior-inferior glenoid deficiency. The Hill-Sachs lesion can be quantified and evaluated by examining the Stryker Notch view.
Computed Tomography Scan
The CT scan can be a very accurate means of determining glenoid version and overall glenoid morphology. The ability to reconstruct the anatomy of the glenoid in three dimensions by subtracting the humerus is an excellent technique. Knowing the character and shape of the articular surface can aide the surgeon in preoperative planning. Substantial bone loss may be a contraindication to arthroscopic stabilization.
Magnetic Resonance Imaging
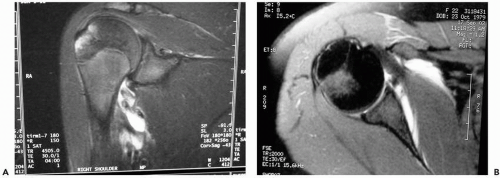
Magnetic resonance imaging (MRI) is used for assessment of associated pathology. Stoller, in 1997, reviewed contrast enhancement with intra-articular gadolinium diethylenetriamine pentaacetic acid (Gd/dtpa), which improved diagnostic ability for assessment of labral tears (both superior and anterior inferior), rotator cuff tears (both partial thickness and full), and articular lesions. When identifying a humeral avulsion of the glenoid labrum, MRIs identifying the humeral detachment of the inferior glenoid labrum (IGL) show that, as the IGL drops inferiorly, a midsagittal coronal oblique arthrographic image located toward the axillary pouch is converted from a full, distended U-shaped structure to a J-shaped structure53 (Fig. 1-8, A and B). This has been further defined by a follow-up study that describes the MRI appearance of a HAGL as an avulsion fracture from the neocortex in the humeral neck. A thin radiolucency was observed inferior to the anatomical neck of the humerus, and once again as the fluid-filled distended U-shaped axillary pouch transforms into a J-shaped structure by the extravasation of contrast material.8 The pressure of this lesion may also be a relative contraindication to arthroscopic stabilization.
SURGICAL OPTIONS: DECISION MAKING
The controversy surrounding open versus arthroscopic techniques for anterior labral stabilization has been ongoing since Johnson published his technique of arthroscopic staple fixation in Techniques of Anterior Glenohumeral Ligament Repair.26 Both open and arthroscopic procedures have involved using bone tunnels, staples, transglenoid sutures, rivets, bioabsorbable tacks, and suture anchors. Initial
studies reported recurrence rates of arthroscopic techniques from 0% to 44%. The earlier arthroscopic techniques were applied to many types of instability patterns and featured techniques that did not resemble principles of established open methods. The major advantage of arthroscopic repair for instability is the ability to accurately identify and treat the specific pathoanatomy, less iatrogenic damage to normal tissues (subscapularis), lower postoperative pain, and improved cosmesis. Some authors also report an easier functional recovery and improved motion than with the open repair method.11 Greater than five dislocations/subluxations has been thought of as a relative contraindication for arthroscopic repair.28,62 Indications for open technique would be bone abnormality, such as an “inverted pair” glenoid or a Hill-Sachs lesion involving greater than 20% to 30% of the articular surface. Some surgeons still advocate the open procedure in high-demand athletes; however, as arthroscopic techniques continue to improve and closely mimic what is done in an open procedure, recurrence rates are similar compared to open.
studies reported recurrence rates of arthroscopic techniques from 0% to 44%. The earlier arthroscopic techniques were applied to many types of instability patterns and featured techniques that did not resemble principles of established open methods. The major advantage of arthroscopic repair for instability is the ability to accurately identify and treat the specific pathoanatomy, less iatrogenic damage to normal tissues (subscapularis), lower postoperative pain, and improved cosmesis. Some authors also report an easier functional recovery and improved motion than with the open repair method.11 Greater than five dislocations/subluxations has been thought of as a relative contraindication for arthroscopic repair.28,62 Indications for open technique would be bone abnormality, such as an “inverted pair” glenoid or a Hill-Sachs lesion involving greater than 20% to 30% of the articular surface. Some surgeons still advocate the open procedure in high-demand athletes; however, as arthroscopic techniques continue to improve and closely mimic what is done in an open procedure, recurrence rates are similar compared to open.
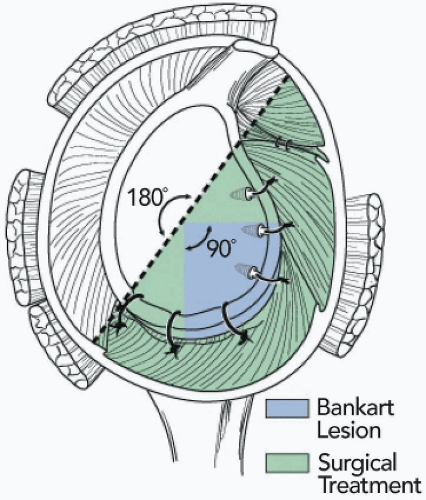
SURGICAL TECHNIQUES
A surgical technique, based on the idea of a 180-degree repair (Fig. 1-9), that is currently used with various modifications. This technique involves an inferior capsular plication, an anterior shift, a Bankart lesion repair with suture anchors, and a rotator interval closure. In operative treatment of an acute anterior dislocation within three weeks, only the Bankart lesion or the anterior inferior glenoid labrum tear is repaired with suture anchors. Generally, the inferior capsular plication and rotator interval closure are deferred for the late repair of the recurrent dislocator. When the repair is later than 3 weeks after the acute dislocation, capsular imbrication and rotator interval closure will be required because it is thought that there is capsular elongation that is commonly associated with repetitive microtrauma. Bigliani et al., in 1992, reported that there was a significant amount of elongation with any type of capsular failure, suggesting a plastic deformation of the capsule occurred.6 Some type of shortening is then required to return the capsule to its anatomical length.
Patient Position
The lateral decubitus, or beach-chair, position can be employed for instability surgery. The beach-chair position offers the advantage of being able to convert to an open procedure easily. When the beach-chair position is used, a sterile arm holder (Tennet Medical Engineering, McConnell, TX) is helpful for both holding a desired arm position and for applying a distraction force to the arm. For the lateral decubitus, a three-point distraction device that allows both longitudinal and vertical traction, enabling the humeral head to be lifted reproducibly from the glenoid, is used (Arthrex Inc., Naples, FL) (Fig. 1-10, A and B). A beanbag is used to stabilize the patient, and a hip-holder is used to stabilize the beanbag in case air is liberated. The patient is positioned in a 30-degree backward tilt to account and place the glenoid in a parallel orientation to the floor. In most cases, general endotracheal intubation is used for anesthesia, with an interscalene block for pain control. Due to the uncomfortable nature of the position, we advocate general anesthesia with or without the block. Preoperative antibiotics are administered intravenously prior to skin incision for portal placement.
Exam Under Anesthesia
An examination of both shoulders, with the patient under anesthesia and in the supine position, is performed, documenting forward elevation, external and internal rotation with the arm at the side, and external and internal rotation with the arm abducted to 90 degrees. An anterior load shift, a posterior “jerk” test, and sulcus tests are performed to assess dominance in instability. This exam under anesthesia is used to confirm and add further information, such as crepitus and/or other pathology that may be present, not to make the diagnosis. When performing the load and shift testing, care should be taken to compare both shoulders for the degree of humeral head translation. In addition, the amount of translation should be noted for each arm position with respect to the degree of humeral rotation and the position of the arm in relation to the plane of the scapula. Arm rotation and position will influence the degree of translation because of the changes that they have on ligament length.
Portal Placement
A standard posterior portal should be placed slightly more lateral than the joint line. If the portal is placed medial to the joint line, then it will require the surgeon to lever the arthroscope against the glenoid, making the stabilization procedure quite difficult.
An 8- to 10-mm incision is made, and then the blunt scope sheath and trocar is inserted atraumatically into the space between the glenoid rim and humeral head.
The anterior series of portals are then made using spinal needles for localization. The first anterior portal is made superior and lateral in the rotator interval, which should be made as high in the anterior superior quadrant as possible, still allowing the cannula to be placed anterior to the biceps tendon. Medial placement of the cannula will compromise access to the glenoid. Care should be taken not to allow the cannula to be posterior to the biceps tendon to avoid entrapment of the tendon with sutures. In general, a 7-mm by 7-cm cannula, either smooth or ridged, is placed for suture shuttling.
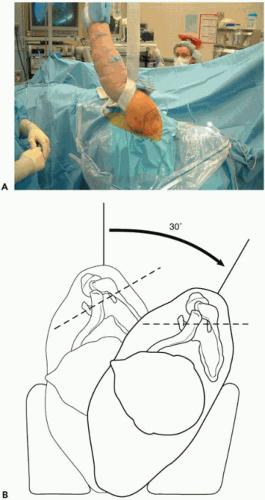 Figure 1-10 (A) Lateral position traction device (Arthrex Inc., Naples, FL). (B) 30-degree tilt positioning.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|